References
McCance, K. L., Huether, S. E., Brashers, V. L., & Rote, N. S. (Eds.). (2019). Pathophysiology : the biologic basis for disease in adults and children (Eighth edition.). Elsevier.
Chu, W. S., Ng, J., Waddington, S. N., & Kurian, M. A. (2024). Gene therapy for neurotransmitter-related disorders. Journal of Inherited Metabolic Disease, 47(1), 176–191.
Medscape. (n.d.). Embeda - morphine/naltrexone. Medscape Reference. Retrieved February 8, 2025, from https://reference.medscape.com/drug/embeda-morphine-naltrexone-999314
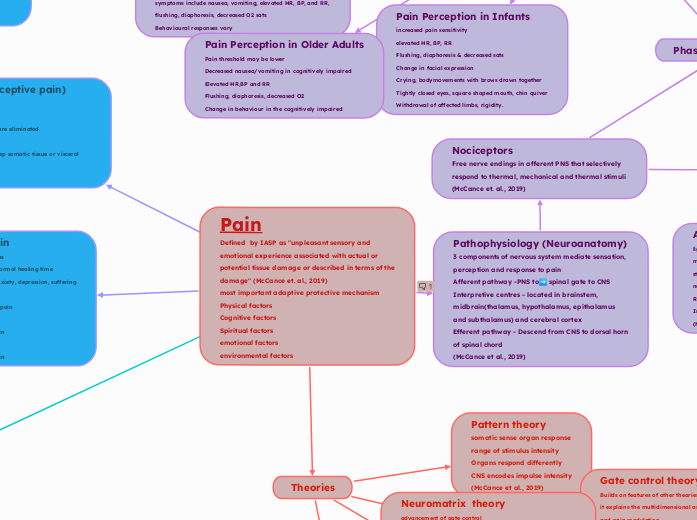
Pain
Defined by IASP as "unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of the damage" (McCance et. al., 2019)
most important adaptive protective mechanism
Physical factors
Cognitive factors
Spiritual factors
emotional factors
environmental factors
Defined as "unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of the damage" (McCance et. al., 2019)
Pharmacology
&
Phamacokinetics
non-opiod
Naproxen
Indication for use
Pain
500 mg PO initially, then 250 mg PO q6-8hr or 500 mg PO q12hr PRN; not to exceed 1250 mg/day naproxen base on day 1; subsequent daily doses should not exceed 1000 mg naproxen base
Extended release: 750-1000 mg PO qDay; may temporarily increase to 1500 mg/day if tolerated well and clinically indicated
Rheumatoid Arthritis, Osteoarthritis, Ankylosing Spondylitis
500-1000 mg/day PO divided q12hr; may increase to 1500 mg/day if tolerated well for limited time
Extended release: 750-1000 mg PO qDay; may temporarily increase to 1500 mg/day if tolerated well and clinically indicated
Dysmenorrhea
500 mg PO initially, then 250 mg PO q6-8hr or 500 mg PO q12hr (long-acting formula); not to exceed 1250 mg/day on first day; subsequent doses should not exceed 1000 mg/day naproxen base
Gout, Acute
750 mg PO initially, followed by 250 mg q8hr until attack subsides
Extended release: 1000-1500 mg qDay, followed by 1000 mg qDay until attack subsides
Migraine
750 mg PO initially, may give additional 250-500 mg if necessary; not to exceed 1250 mg in 24 hr
(medscape, n.d)
Metabolism & Excretion
Metabolism
: Metabolized in liver via conjugation
Metabolites: 6-Desmethylnaproxen, glucuronide conjugates
Enzymes inhibited: COX-1, COX-2
Elimination
Half-life: 12-17 hr
Clearance: 0.13 mL/min/kg
Excretion: Urine (95%), feces (<3%)
(medscape, n.d)
Pharmacokinetics
Absorption
Bioavailability: 95%
Onset: 30-60 min
Duration: < 12 hr
Peak serum time: 1-4 hr (tablets); 2-12 hr (delayed release empty stomach); 4-24 hr (delayed relase with food)
Peak plasma concentration: 62-96 mcg/mL
Distribution
Protein bound: <99%
Vd: 0.16 L/kg
(medscape, n.d)
Mechanism of Action
Inhibits synthesis of prostaglandins in body tissues by inhibiting at least 2 cyclooxygenase (COX) isoenzymes, COX-1 and COX-2
May inhibit chemotaxis, alter lymphocyte activity
decrease proinflammatory cytokine activity, and inhibit neutrophil aggregation;
these effects may contribute to anti-inflammatory activity
(medscape, n.d)
Acetaminophen
Indications for Use
Analgesia & Fever
immediate-release
Regular strength: 325-650 mg PO/PR q4hr PRN; not to exceed 3250 mg/day; under supervision of healthcare professional, daily doses of up to 4 g/day may be used
Extra Strength: 1000 mg PO q6-8hr PRN; not to exceed 3000 mg/day; under supervision of healthcare professional, daily doses of up to 4 g/day may be used:
extended-release
2 capsules (1300 mg) PO q8hr PRN; not to exceed 3.9 g/day
maximum dose
Acetaminophen containing products: Not to exceed a cumulative dose of 3.25 g/day of acetaminophen; under supervision of healthcare professional, daily doses of up to 4 g/day may be used
Tylenol Extra-Strength (ie, 500 mg/tab or cap): Not to exceed 3 g/day (6 tabs or caps); under supervision of healthcare professional, daily doses of up to 4 g/day may be used
Mechanism of action
Acts on hypothalamus to produce antipyresis
May work peripherally to block pain impulse generation; may also inhibit prostaglandin synthesis in CNS
(medscape, n.d)
Pharmacokinetics
Peak Plasma Time: 10-60 min (PO immediate-release); 60-120 min (PO extended-release); 6 hr (PO 500 mg, conventional tablet); 8 hr (PO 650 mg, extended-release tablet)
Peak Plasma Concentration: 2.1 mcg/mL (PO 500 mg, conventional tablet); 1.8 mcg/mL (PO 650 mg, extended-release tablet)
Onset: 1 hr
Distribution: 1 L/kg
Protein Bound: 10 to 25%
(medscape, n.d)
Metabolism & Excretion
Metabolism: Liver (microsomal enzyme systems); conjugation (glucuronic/sulfuric acid)
Metabolites: N-acetyl-p-benzoquinoneimine, N-acetylimidoquinone, NAPQI; further metabolized via conjugation with glutathione
Half-life elimination: 1.25-3 hr (adolescents); 2-5 hr (children); 4 hr (infants); 7 hr (neonates); 2-3 hr (adults)
Excretion: urine (principally as acetaminophen glucuronide with acetaminophen sulfate/mercaptate)
(medscape, n.d)
Ibuprofen
Indications for use
Pain/Fever/Dysmenorrhea
OTC: 200-400 mg PO q4-6hr; not to exceed 1200 mg unless directed by physician
Prescription: 400-800 mg PO q6hr; not to exceed 3200 mg/day
Inflammatory Disease
400-800 mg PO q6-8hr; not to exceed 3200 mg/day
Osteoarthritis
300 mg, 400 mg, 600 mg, or 800 mg PO q6-8hr; not to exceed 3200 mg/day
Monitor for gastrointestinal (GI) risks
Rheumatoid Arthritis
300 mg, 400 mg, 600 mg, or 800 mg PO q6-8hr; not to exceed 3200 mg/day
Monitor for GI risks
Metabolism & Excretion
Metabolism:
Rapidly metabolized in liver (primarily by CYP2C9; CYP2C19 substrate) via oxidation to inactive metabolites
Metabolites
Metabolite A: (+)-2-[4'-(2-hydroxy-2-methylpropyl) phenyl] propionic acid
Metabolite B: (+)-2-[4'-(2-carboxypropyl) phenyl] propionic acid
Elimination
Half-life: 2-4 hr (adults); 1.6 hr (children 3 mon to 1 year; 35-51 hr (day 3), 20-33 hr (day 5)
Excretion: Urine (50-60%; <10% unchanged); remainder in feces within 24 hr
(medscape, n.d)
Pharmacokinetics
Absorption
Rapidly absorbed (85%)
Bioavailability: 80-100%
Onset: 30-60 min
Duration: 4-6 hr
Peak plasma time (adults)
Conventional tablet: 120 min; Chewable tablet: 62 min
Oral suspension: 47 min
Peak plasma time (febrile children)
Chewable tablet: 86 min
Oral suspension: 58 min
Peak plasma concentration
Conventional tablet: 20 mcg/mL; Chewable tablet: 15 mcg/mL
Oral suspension: 19 mcg/mL
Distribution
Protein bound: 90-99%; concentrations >20 mcg/mL
Vd: 0.12 L/kg (adults); 0.164 L/kg (children)
Mechanism of Action
Inhibits synthesis of prostaglandins in body tissues by inhibiting at least 2 cyclo-oxygenase (COX) isoenzymes, COX-1 and COX-2
May inhibit chemotaxis, alter lymphocyte activity, decrease proinflammatory cytokine activity, and inhibit neutrophil aggregation; these effects may contribute to anti-inflammatory activity (medscape, n.d)
Opioid
Fentanyl
Indications for use
Surgery Premedication
50-100 mcg/dose IM or slow IV 30-60 min prior to surgery
Adjunct to regional anesthesia: 25-100 mcg/dose slow IV over 1-2 min
General Anesthesia
Minor surgical procedures: 0.5-2 mcg/kg/dose IV
Major surgery: 2-20 mcg/kg/dose initially; 1-2 mcg/kg/hr maintenance infusion IV; discontinue infusion 30-60 min prior to end of surgery; limit total fentanyl doses to 10-15 mcg/kg for fast tracking and early extubation
(medscape, n.d)
Metabolism
&
Excretion
Metabolism
Metabolized in liver by CYP3A4
Elimination
Half-life: 2-4 hr
Total plasma clearance: 8.3 mL/min/kg
Excretion: Urine (75%), feces (9%)
(medscape, n.d)
Pharmacokinetics
Absorption
Bioavailability: 50%
Onset: IV, immediate; IM, 7-15 min
Duration: IV, 0.5-1 hr; IM, 1-2 hr
Peak plasma time: IV (≤100 mcg), 30-60 min; IM, 1-2 hr
Concentration: 0.2-2 ng/mL (adverse effects occur at >2 ng/mL)
Distribution
Protein bound: 80-85%
Vd: 4-6 L/kg
(medscape, n.d)
Mechanism of action
Narcotic agonist-analgesic of opiate receptors;
inhibits ascending pain pathways, thus altering response to pain; increases pain threshold;
produces analgesia, respiratory depression, and sedation
(medscape, n.d)
Oxycodone
Indication for use
moderate to severe pain -Opioid-tolerant:: 10-30 mg PO q4-6hr
Opioid-naïve (initial dose): 5-15 mg PO q4-6hr
Chronic Severe Pain
Controlled-release products (eg, OxyContin, Xtampza ER) are indicated for the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate
(medscape, n.d)
Metabolism
&
Excretion
Metabolism
Metabolized in liver by CYP3A mediated N-demethylation to noroxycodone
This is the primary metabolic pathway of oxycodone with a lower contribution from CYP2D6 mediated O-demethylation to oxymorphone
Metabolites: Noroxycodone, oxymorphone (and glucuronide conjugates)
CYP2D6 poor metabolizers may not achieve adequate analgesia; ultra-rapid metabolizers (≤7% of Caucasians and ≤30% of Asian and African populations) may have increased toxicity as consequence of rapid conversion
Elimination
Half-life: 2-4 hr; 4.5 hr (OxyContin)
Excreted, urine: Free and conjugated oxycodone (8.9%), free noroxycodone (23%), free oxymorphone less than (1%), conjugated oxymorphone (10%), free and conjugated noroxymorphone (14%), reduced free and conjugated metabolites (up to 18%)
Clearance: 1.4 L/min
(medscape, n.d)
Pharmacokinetics
Bioavailability: 60-87%
Increases in peak plasma concentration by 100-150% and AUC by 50-60% following a high-fat and high-calorie meal
Onset:10-15 min (immediate-release)
Duration: 3-6 hr (immediate release); ≤12 hr (controlled release)
Peak plasma time: 1.5-1.9 hr (immediate-release); 4-5 hr (OxyContin 10-80 mg); 4.5 hr (Xtampza ER)
Steady state: 24-36 hr (Xtampza ER)
(medscape, n.d)
Distribution
Once absorbed, oxycodone is distributed to skeletal muscle, liver, intestinal tract, lungs, spleen, and brain
Protein bound: 45%
Vd: 2.6 L/kg
(medscape, n.d)
Mechanism of action
Narcotic agonist-analgesic of opiate receptors
inhibits ascending pain pathways, thus altering response to pain produces analgesia, respiratory depression, and sedation
(medscape, n.d)
Morphine
Indications for use
Used for Chronic severe pain
management of pain is severe enough to require daily, around-the-clock, long-term opioid treatment
alternative treatment options have been inadequate (medscape, n.d)
Metabolism & Excretion
Metabolism: Glucuronidation and sulfation in the liver to produce including morphine-3-glucuronide, (about 50%) and morphine-6-glucuronide, M6G (about 5 to 15%) or morphine-3-etheral sulfate; naltrexone extensively metabolized to 6-beta-naltrexol
Clearance: 20-30 mL/min/kg
Excretion: Morphine: 10% excreted unchanged in urine, 55-65 metabolites excreted in urine
(medscape, n.d)
Pharmacokinetics
Bioavailability: 20-40%
Peak Plasma Time: 7.5 hr
Protein Binding: 30-35%
Half-Life: 29 hr
Volume of distribution: 3-4 L/kg
(medscape, n.d)
Mechanism of action
Morphine is a pure opioid agonist,
relatively selective for the mu-opioid receptor;
inhibits ascending pain pathways, which causes alteration in response to pain;
produces analgesia, respiratory depression, and sedation
Naltrexone is a centrally acting mu-opioid antagonist
Naltrexone active & antagonizes when the tablet is either chewed, crushed, or dissolved
(medscape, n.d)
Chronic Pain
Lasting > 3-6 months
Pain lasts beyond normal healing time
Accompanied by anxiety, depression, suffering
Includes:
Persistent low back pain
Hyperesthesias
Phantomm limb pain
Cancer pain
Chronic Post-op pain
Acute Pain (nociceptive pain)
Lasts seconds to days
Sudden
relived when pain mediators are eliminated
Anxiety is common
Arises from cutaneous and deep somatic tissue or visceral organs
Referred pain
Felt in area away from point of origin
Impulses convey from several visceral neurons to one ascending neuron
Becomes hard for brain to distinguish
More receptors on skin promote pain experience at referred site.
(McCance et al., 2019)
Visceral pain
Transmitted by C fibres
Pain in internal organs and lining of body cavities
Transmitted by sympathetic affarents
Poorly localized - less nociceptors in visceral structures
Associated with nausea/vomiting, hypotension, restlessness, shock
Often radiates
(McCance et al., 2019)
Somatic Pain
occurs from muscle, bone, joints and skin
Sharp and well localized (A-delta fibres transmission)
Dull aching (C fiber transmission)
(McCance et al., 2019)
Pathophysiology (Neuroanatomy)
3 components of nervous system mediate sensation, perception and response to pain
Afferent pathway -PNS to➡️ spinal gate to CNS
Interpretive centres - located in brainstem, midbrain(thalamus, hypothalamus, epithalamus and subthalamus) and cerebral cortex
Efferent pathway - Descend from CNS to dorsal horn of spinal chord
(McCance et al., 2019)
Nociceptors
Free nerve endings in afferent PNS that selectively respond to thermal, mechanical and thermal stimuli (McCance et. al., 2019)
Phases of Nociception
modulation phase
Different mechanisms increase/decrease pain signal transmission
Can occur before, during or after pain perception (McCance et. al., 2019)
Neurotransmitters
Diverse Group of chemical messengers (Chu et al., 2024)
Inhibitory neurotransmitters
GABA, Glycine, norepinephrine, serotonin
Endogenous Opioids
inhibit pain impulse in brain, spinal cord and periphery
(McCance et al., 2019)
endorphins
They are endogenous morphins
Produced in brain
beta-endorphin binding in hypothalamus +pituitary gland =exhiliaration and natural pain releif
(McCance et al., 2019)
dynorphins
most potent endogenous opiod
bind with K receptors = blocked pain signal in brain
Involved in mood disorder and drug addiction
(McCance et al., 2019)
endormorphins
Bind with receptors in brain, brainstem and GI tract
Analgesic and antiinflammatory effects
(McCance et al., 2019)
Enkephalins
most prevalent of natural opioids found in
Hypothalamus
PAG matter
medulla
dorsal horn
Inflammation - mediator of excitatory neurotransmitters
Bradykinin, Leukotrienes, Prostaglandins, TNF-Alpha, Nitric Oxide, Substance -P, ATP
Cause release of substance P, CGRP, ATP.
Excitatory neuroTransmitters in brain and spinal cord
Reduce activation thresholds = increased nociceptor responsiveness
Glutamate, Aspartate, Substance P, Calcitonin
Placebo/Nocebo effect pathway
Cognitive expectations (Placebo = positive expectation, nacebo = negative expectations
(McCance et al., 2019)
Conditioned pain modulation pathway
Pain releif when 2 stimuli occur at same time from different sites
spinal-medullary-spinal pathway
basis of non pharmacological therapy i.e (acupuncture, cold/heat therapy
(McCance et al., 2019)
Segmental inhibition pathway
A-beta, A-delta and C fibre impulses arrive at same time at spinal level
Decrease in pain transmission occurs
example rubbing injured area for pain releif
(McCance et al., 2019)
Descending Inhibitory Pathway
neurotransmitters inhibit/facilitate pain
Afferent stimulation of PAG+raphe nucleus = efferent pathway stimulation = afferent pain signal inhibited @ dorsal horn
RVM stimulate efferent pathways = facilitation/inhibition of pain @ dorsal horn
Inhibitory pathways activate opioid receptors = inhibitory neurotransmitters released
(McCance et al., 2019)
Perception phase
conscious awareness of pain
Takes place primarily in reticular, limbic systems and cerebral cortex.
Made of 3 systems' interactions - Sensory-discriminative system., affective-motivational system and cognitive-evaluative system
Pain perception changes with age
(McCance et al., 2019)
Pain Perception in Older Adults
Pain threshold may be lower
Decreased nausea/vomiting in cognitively impaired
Elevated HR,BP and RR
Flushing, diaphoresis, decreased O2
Change in behaviour in the cognitively impaired
Pain Perception in Infants
increased pain sensitivity
elevated HR, BP, RR
Flushing, diaphoresis & decreased sats
Change in facial expression
Crying, bodymovements with brows drawn together
Tightly closed eyes, square shaped mouth, chin quiver
Withdrawal of affected limbs, rigidity.
Pain Perception in Children
Pain threshold lower than in infants
symptoms include nausea, vomiting, elevated HR, BP, and RR, flushing, diaphoresis, decreased O2 sats
Behavioural responses vary
Cognitive-evaluative
system
Learned behaviour of pain experience
can modulate perception of pain
mediated through cerebral cortex
Pain threshold and tolerance are subjective and influence individual's perception of pain
Gender, genetics, culture, role expectations, role socialization, age, physical and mental health influences occur
(McCance et al., 2019)
affective-motivational system
behaviours and response to pain
mediated through reticular formation, limbic
Projects to prefrontal lobe
(McCance et al., 2019)
Sensory-discriminative system
mediated by somatosensory cortex
Identifies presence, character location and intensity of pain
(McCance et al., 2019)
Transmission phase
conduction of impulse along A-delta and C fibres into dorsal horn of spinal cord (primary order neurons)
Synapses formed with excitatory or inhibitory interneurons (2nd order neurons)
Impulse synapse with projection neurons (3rd order neurons)
Impulse crosses midline of spinal cord to brain through 2 spinothalamic tracts.
anterior spinothalamic carries fast impulse (acute sharp pain)
lateral spinothalamic carries slow impulse (dull/chronic pain)
Impulse project to somatosensory cortex for interpretation/intensity - to other areas for response
(McCance et al., 2019)
Transduction phase
Stimulation of nerves in periphery
Begins with tissue damage due :
exposure to Inflammatory chemicals stimuli (bradykinin, histamine, leukotreines, prostaglandins, interleukins (IL-1, IL-6, IL-7, IL-17)
mechanical or thermal stimuli
Nociceptors activated
(McCance et al., 2019)
Types
A- beta fibres
Large myelinated
Transmit touch and vibration sensations
Donot normally transmit pain
Play a role in pain modulation
(McCance et al., 2019)
Unmyelinated
C-fibres
Polymodal
Stimulated by mechanical, thermal and chemical nociceptors
Slowly transmit dull, aching or burning sensations
Sensations are poorly localized and longer lasting
(McCance et al., 2019)
A-delta fibres
lightly myelinated fibres
medium sized fibres
stimulated by mechanonociceptors and/or mechanothermal nociceptors
Rapidly transmit "fast" pain sensations
Initiates reflex withdrawal before pain sensation is perceived
(McCance et al., 2019)
Theories
Neuromatrix theory
advancement of gate control
brain produces inputs patterns of impulses from various inputs
genetic
sensory-discrimative
affective
motivational
evaluative cognitive
Patterns may originate from brain with no external input
Pain experiences involve extensive network of brain regions
Showcases the plasticity of brain
Provides a holistic consideration of pain
Pain can be felt in the absence of input i.e phantom limb pain
(McCance et al., 2019)
Gate control theory
Builds on features of other theories of pain
it explains the multidimensional aspects of pain perception and pain modulation
Pain transmission is regulated by impulses to the spinal cord, where substantia gelatinosa cells act as a gate.
Spinal gate regulate pain transmission to higher centres in CNS
Large myelinated a-delta + small unmyelinated C fibres respond to painful stimuli
Fibres terminate in interneurons of substantial gelatinosa and open spinal gate to transmit perception of pain
Nociceptive stimulation (touch sensor)
Spinal gate closure from nonnociceptive A-beta fiber stimulation reduces pain perception.
(McCance et al., 2019)
Pattern theory
somatic sense organ response
range of stimulus intensity
Organs respond differently
CNS encodes impulse intensity
(McCance et al., 2019)
Specificity theory
intensity d/t amt of tissue injury
Pricking finger vs cutting hand
Applies to acute pain
(McCance et al., 2019)