heavily involves the
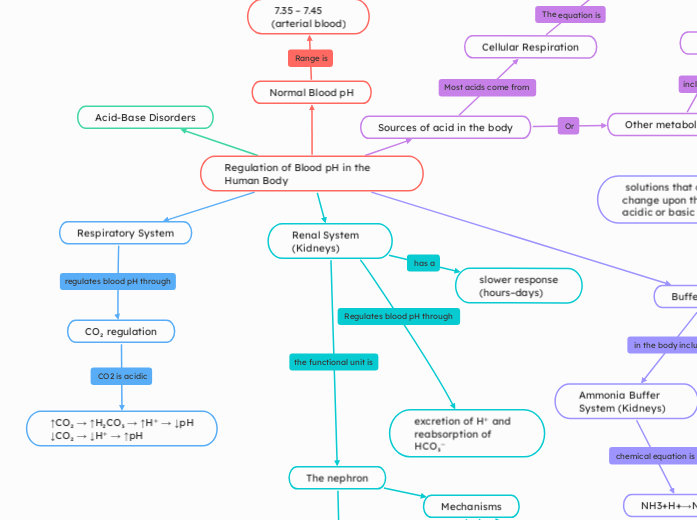
Regulation of Blood pH in the Human Body
Acid-Base Disorders
(medical applications)
Alkalosis (pH > 7.45)
Metabolic Alkalosis
high HCO₃⁻ or low acid
Acidosis (pH < 7.35)
Metabolic Acidosis
low HCO₃⁻ or high acid
Renal System (Kidneys)
The nephron
Key areas
Collecting Duct
traps H⁺ using NH₃ →NH₄⁺ (pee)
Distal tubule
Proximal tubule
metabolizes glutamine → 2 NH₄⁺ + 2 HCO₃⁻
Mechanisms
Secrete H⁺
Reabsorb HCO₃
slower response
(hours–days)
excretion of H⁺ and reabsorption of HCO₃⁻
Respiratory System
CO₂ regulation
Le Chatelier’s Principle
CO₂ decreases, equilibrium shifts left → fewer H⁺ → higher pH
CO₂ increases, equilibrium shifts right → more H⁺ → lower pH
↑CO₂ → ↑H₂CO₃ → ↑H⁺ → ↓pH
↓CO₂ → ↓H⁺ → ↑pH
Hyperventilation (↑ breathing rate):
CO₂ eliminated rapidly
Respiratory Alkalosis
Hypoventilation (↓ breathing rate)
CO₂ accumulates
Respiratory Acidosis
Buffer Systems
solutions that can resist pH change upon the addition of an acidic or basic components.
Ammonia Buffer System (Kidneys)
NH3+H+→NH4+
NH₃ freely diffuses, NH₄⁺ is trapped in urine and excreted
Generates new HCO₃⁻ for each H⁺ secreted
Protein Buffers
Hemoglobin in red blood cells
Reduces Hemoglobin's affinity for O₂ (facilitates delivery)
Bohr effect
Binds H⁺ directly
deoxygenated Hemoglobin binds more CO₂ and H⁺
Haldane Effect
Phosphate Buffer System
Urine & Intracellular Fluid
generate new bicarbonate (Le Chatelier’s Principle)
H2PO4−⇌H++HPO42
excrete H⁺ in kidneys via NaH₂PO₄ (acidic salt)
Bicarbonate Buffer System (Main System in Blood)
Act instantly to resist pH changes
CO2+H2O⇌H2CO3
H2CO3⇌H++HCO3
Sources of acid in the body
Other metabolic acids
Dietary intake or drug metabolism
Ketone bodies
fat metabolism, diabetic ketoacidosis
Lactic acid
anaerobic exercise
Cellular Respiration
CO2+H2O↔H2CO3
H2CO3 ↔H+ +HCO3−
carbonic acid dissociating into bicarbonate and hydrogen ions
Normal Blood pH
7.35 – 7.45 (arterial blood)
Ionization of intermediates in biochemical pathways
Oxygen delivery (Bohr effect)
Enzyme activity