av cheyenne andrew 6 år siden
175
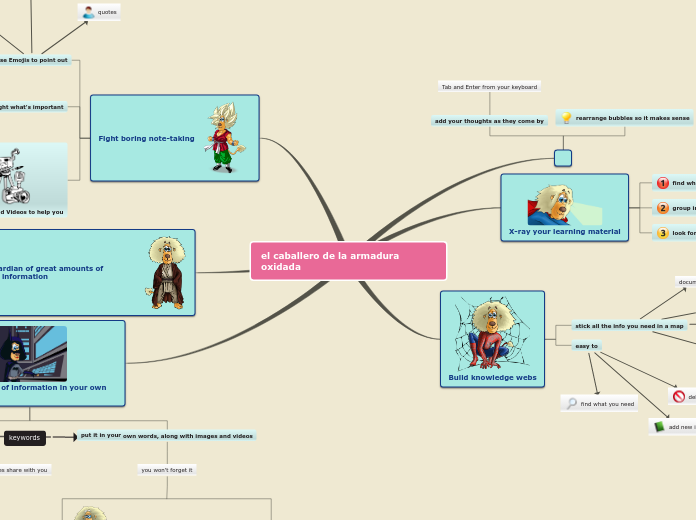
Cheyenne's Mind map
In medical settings, ethnographic research has been instrumental for over fifty years. Despite its long history, there is a notable gap in studies focusing on socio-cultural processes within hospitals.