Thyroid Storm:
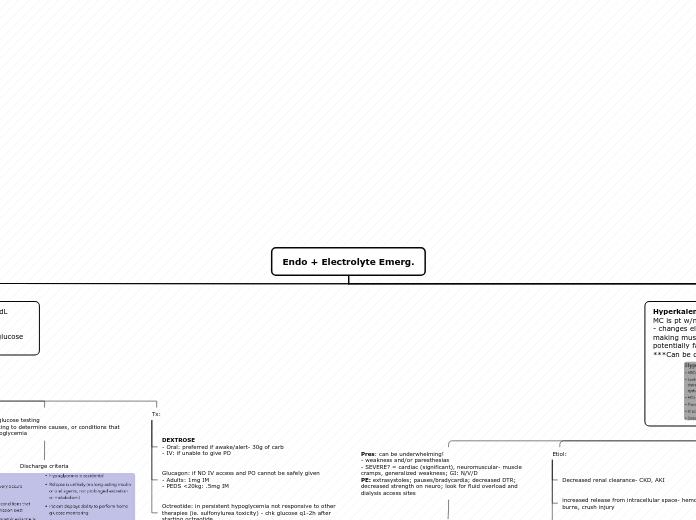
Endo + Electrolyte Emerg.
Myxedema coma- life-threatening hypothyroidism
- hallmark= AMS
- precipitated by: sepsis, cardiac dz, resp. distress, CNS dz, cold exposure, drug use, non-compliance w/tx
Tx: Thyroxine IV bolus
s/sx: severe hypothermia, hypoventilation, hyponatremia, hypoglycemia, hytoTN, rhabdo, AKI
Pituitary apoplexy- spontaneous hemorrhage or infarction of preexisting pituitary adenoma
- SUDDEN, severe headache
Tx: admit ICU + CS + neurosurg consult + endo, ophthalmology, and neurology
CT (non contrast) and MRI may show sellar mass and hemorrhage
RF: pregnancy, head trauma, pituitary radiation, dopamine agonist tx
Pheochromocytoma- catecholamine secreting tumor in adrenal medulla
- more common in women
- episode often precipitated by: abd movement, trauma, drugs, idiopathic
- HALLMARK = HTN
Tx: Control HTN w/alpha blocker; BB AFTER alpha blockage
*avoid BB alone
Dx: Fhx, elevated urinary catecholamine; CT or MRI of abd/pelvis; MIBG scan to detect tumors not seen on CT or MRI
s/sx: Catecholamine EXCESS= HTN crisis- HA, CP, palp, SOB, sweating
Subtopic
Hyperkalemia: serum K >5.5 mEq/L
MC is pt w/missed dialysis w/ESRD
- changes electrochemical gradient of cells, making muscles weak and cardiac dysrhythmias potentially fatal outcomes
***Can be d/t lab error, so repeat labs
Tx: if ECG manifestations or pt is hemodynamically unstable then first tx is STABILIZE MYOCARDIUM
1. Stabilize myocardium w/Calcium gluconate or Ca chloride - this will reverse ECG changes
2. intracellular K transfer w/regular insulin
3. decrease total K w/Furosemide
- can also use Kayexelate (binds K, not used much), Hemodialysis (if hemodynamically unstable, or if pt is dialysis dependent), or Patiromer (binds K)
EKG: marker for clinically significant hyperkalemia
1. tall, peaked T waves (>6.5)
2. flattening of p wave, prolongation PR interval and widening of QRS (>7)
3. loss of p waves leading to sine-waves: fusion of wide QRS w/ST-T segments (8-10)
Etiol:
altered transfer to intracellular space- acidosis, insulin deficiency, succinylcholine
increased release from intracellular space- hemolysis, rhabdo, burns, crush injury
Decreased renal clearance- CKD, AKI
Pres: can be underwhelming!
- weakness and/or paresthesias
- SEVERE? = cardiac (significant), neuromuscular- muscle cramps, generalized weakness; GI: N/V/D
PE: extrasystoles; pauses/bradycardia; decreased DTR; decreased strength on neuro; look for fluid overload and dialysis access sites
Cardiac pres: 2nd or 3rd degree heart block; wide complex tachycardia; progression to vFib; asystole
Hypoglycemia: serum glucose <70mg/dL
- clinical syndrome of altered autonomic dysfunction and impaired cognition
- sx of hypoglycemia appear at varying glucose levels
Hyperglycemia: FBG >90-130mg/dL or Postprandial BG >180
- W/U: Thorough H&P
- minor sx: UA looking for ketones and BMP to see if increased gap metabolic acidosis
- ill appearing/hemodynamically unstable/suspect HHS or DKA: ABCs, 2 large bore IV- NS 1-2L; cardiac monitoring
Tx:
- Mild-mod: may only need IV fluids
- DKA and HHS:
1. correct intravascular vol. depletion: NS 1L/hr; LR may be better option to avoid hyperchloremic non-anion gap metabolic acidosis
2. manage electrolyte abnormalities: replace K+ and Bicarb
- K+ b/w 4-5 is NL
>5.5= insulin infusion
3.5-5.5= add K to fluids
<3.5= hold insulin, add K and restart insulin later
3. insulin replacement: IV infusion of regular insulin (preferred); at 10units/hr in 70kg pt
4. ID underlying cause and tx that - infx= abx
DDX:
DKA
MCC: infection, disruption of insulin therapy, presentation of new onset DM
usu. in T1DM; younger people
absolute insulin deficiency; hyperglycemia, anion gap acidosis; dehydration
HHS- hyperosmolar hyperglycemic state
MCC: poorly controlled T2DM w/underlying infxn
usu. in T2DM; older people
Hyperglycemia, hyperosmolar, dehydration, *WITHOUT significant ketoacidosis*
Presentation:
- mild: may be asx
- BG >180 (renal threshold) = polyuria/dipsia/phagia/wt loss
- MOD: abd pain, Kussmaul resp, hypoTN, ketotonic breath, tachycardia
- SEV: seizures, focal weakness, lethargy, coma, death
complication: cerebral edema- usually in children and young adults; preceded by HA, lethargy, neuro, bradycardia, respiratory arrest