Obsessive-Compulsive Disorder (OCD)
Emotional Impact:
Depression
Social withdrawal
Feelings of shame or embarrassment
Anxiety and distress
Treatment Approaches:
Lifestyle changes: stress management, mindfulness, exercise
Support groups and peer support
Medication (e.g., selective serotonin reuptake inhibitors or SSRIs)
Cognitive-Behavioral Therapy (CBT), particularly Exposure and Response Prevention (ERP)
Long-Term Outcomes:
Preventing relapse with consistent follow-up care
Building resilience through coping strategies
Role of ongoing therapy
Importance of early intervention
Associated Disorders:
Excoriation (skin-picking)
Trichotillomania (hair-pulling)
Hoarding Disorder
Body Dysmorphic Disorder
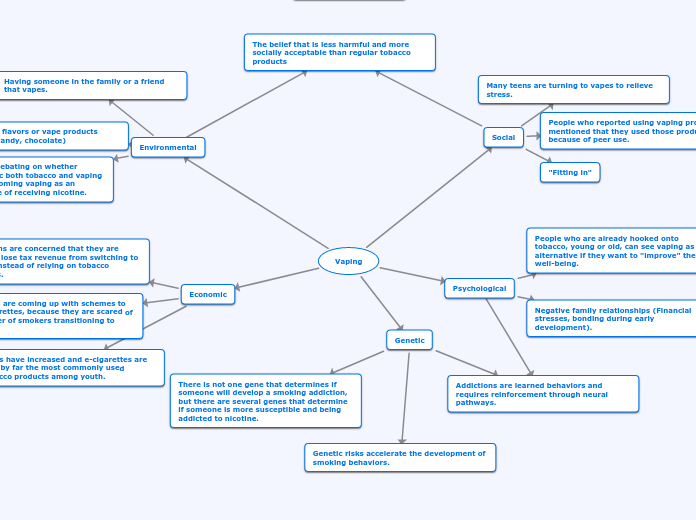
Causes & Risk Factors:
Family history of anxiety disorders
Environmental factors (e.g., traumatic events)
Brain structure and functioning (e.g., overactivity in certain neural pathways)
Genetic predisposition
Behaviors
Compulsions:
Arranging items until “just right”
Counting or repeating actions
Repeated checking
Excessive cleaning/washing
Obsessions:
Unwanted sexual or aggressive thoughts
Doubts about safety (e.g., leaving doors unlocked)
Fear of contamination
Intrusive thoughts
Pathophysiology
Key Brain Regions:
Thalamus:
Hyperactivity in this region reinforces obsessive thoughts and behaviors.
Acts as a relay station, filtering sensory information.
Basal Ganglia:
Dysfunction contributes to compulsive behaviors.
Plays a role in the initiation and control of movements and habits.
Includes structures like the striatum.
Anterior Cingulate Cortex (ACC):
Dysregulation leads to heightened awareness of perceived "errors."
Associated with error detection and emotional regulation.
Orbitofrontal Cortex (OFC):
Overactivity in the OFC contributes to excessive worry and intrusive thoughts.
Involved in decision-making and evaluating rewards.
Brain Circuitry Dysfunction
Associated with hyperactivity in specific brain regions,
Cortico-striato-thalamo-cortical (CSTC)
Involves complex interactions between brain circuits
Environmental factors
Epigenetics:
Environmental stressors, infections (e.g., PANDAS syndrome), and trauma may modify gene expression and contribute to OCD development.
Neuroinflammation:
Elevated cytokines and inflammatory markers in OCD patients suggest a possible role of immune dysregulation.
PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections):
Inflammatory processes may alter brain function in susceptible individuals.
In some cases, OCD is triggered by autoimmune responses following streptococcal infections.
Genetic
Variants in genes regulating serotonin (e.g., SLC6A4), glutamate, and dopamine pathways have been implicated.
Family studies indicate a heritability rate of 45-65% in first-degree relatives.
Neurotransmitters
Glutamate:
Emerging research implicates glutamate in OCD, suggesting excitatory-inhibitory imbalances in neural circuits.
Dopamine:
Hyperactivity in the striatum exacerbates compulsions.
Altered dopamine activity may influence compulsive behaviors and habit formation.
Serotonin (5-HT):
SSRIs (Selective Serotonin Reuptake Inhibitors) help restore serotonin balance.
Dysregulation affects mood, anxiety, and inhibitory control.
Reduced serotonin signaling is a significant factor in OCD.