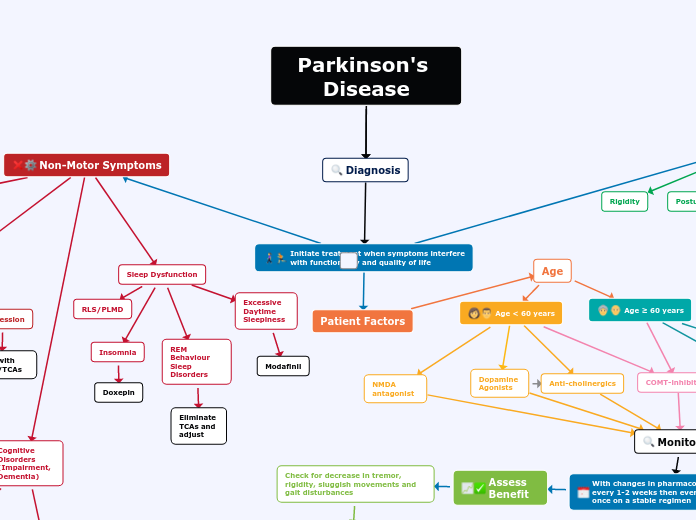
Diagnosis
Parkinson's Disease
- Reduce the dose of or discontinue medications contributing medications
-Non-pharm → change positions slowly, avoid large meals/excessive alcohol, increase fluid intake, elevate head on pillows
- Consider initiation of domperidone, fludrocortisone or midodrine
Assess for Complications
Hallucinations
- Gradually decrease dose + eliminate PD medications w/ potential for hallucinations in the following order : Anticholinergics, MAO-B inhibitors, DA, Levodopa
- If above fails, consider antipsychotics (quetiapine, clozapine)
Freezing
- Increase levodopa dose
- Add DA or MAO-B
- Non Pharm → sensory cues + devices
Dyskinesias
- Increase (diphasic) or reduction (peak-dose) in levodopa dose
- Add DA
- Increase dose of DA if on concurrent therapy
- Add Amantadine
Motor Complications "Wearing Off"
-increase Levodopa dose if patient does not have dyskinesia or increase frequency if patient has dyskinesia. Addition of a dopamine agonist, COMT or MAO-B inhibitor can also be considered.
Lower dose of Levodopa
Treat with SSRIs/TCAs/Benzodiazepines
Anxiety
Adjust dopaminergic drugs
Autonomic Dysfunction (GI disorders, Orthostatic Hypotension, Sexual Dysfunction, Urinary Incontinence)
Urinary Incontinence
Oxybutynin, Tolterodine, Propantheline
Sexual Dysfunction
Sildenafil
Orthostatic Hypotension
Fludrocortisone, Domperidone, midodrine
GI Disorders
PEG, stool softeners, Lactulose, Domperidone
Excessive Daytime Sleepiness
Modafinil
Monitoring
With changes in pharmacotherapy follow-up every 1-2 weeks then every 3-6 months once on a stable regimen
Assess Benefit
Check for decrease in tremor, rigidity, sluggish movements and gait disturbances
Suboptimal Response
Consider, increasing the dose of the agent; initiating Levodopa/Dopamine agonist; adding therapy (i.e. dopamine agonist, MAO-B i, COMT-i, etc); changing time of administration/formulation
mild bradykinesia
Non-Motor Symptoms
Patient Factors
Age
Age ≥ 60 years
Dopamine precursor + decarboxylase
Age < 60 years
COMT-inhibitors
NMDA antagonist
Initiate treatment when symptoms interfere with functionality and quality of life
Rigidity
MAO-B inhibitors
Dopamine Agonists
Anti-cholinergics
Motor Symptoms
Sleep Dysfunction
RLS/PLMD
REM Behaviour Sleep Disorders
Eliminate TCAs and adjust
Insomnia
Doxepin
Mood Disorders (Anxiety, Depression)
Depression
Treat with SSRIs/TCAs
Cognitive Disorders (Impairment, Dementia)
Treat with acetylcholinesterase inhibitors such as donepezil, rivastigmine or galantamine
Gradually discontinue anticholinergic medications
Akinesia
severe bradykinesia
Postural instability
Tremor