Thorax and Abdomen
Thorax
Respiratory system
physiology
Gas transport
Oxy-hemoglobin binding curve
PCO2
Temp
Ph
CO2 transport
Plasma CO2
7% dissolved directly
Hemoglobin bound CO2
23%
Bicarbonate
about 70% of CO2
O2 transport
Hemoglobin
98% of O2 transport
Binds up to 4 O2 molecules
Respiration (gas exchange)
Respiratory control mechanisms
Neuronal influence
Conscious and unconscious can effect breathing rates
Brain stem control
Pons and medulla regulate respiration
Chemoreceptors
Periphrail
Responds to PO2, PCO2
and pH changes
Medulla
Sensitive to cerebrospinal CO2
Perfusion
Transfer efficiency
Oxygen availabilty
Hypoxia
Ventilation
Patterns of ventilation
Minute ventilation
Diameter of airways
viscosity of air
Airway resistance
Lung volumes and capacity
Gas laws
Dalton's law
How gases are exchanged in respiratory system
Boyle's law
How changes in lung volume affect air pressure
during breathing
High to low pressure
Vocalization
Voice is generated by airflow from the lungs. When the air from the lungs blows through the vocal folds
Ph regulation
controlling the amount of carbon dioxide (CO2) exhaled
Protection
Against pathogens
Sticky layer of mucous over cilia to trap large particles
Ciliated epithelium in watery saline layer
Conditioning of air
Humidifying
Add water vapor
Warming
To body temp
Gas excahnge
Transport
Movement of O2 and CO2 in
blood
Exchange 3
Gas exchange between
blood and tissues
Exchange 2
Gas exchange between alveoli
and lung capillaries
Exchange 1
Pulm ventilation
and alveolar ventilation
Alveoli
Tertiary bronchi
Secondary bronchi
L & R bronchi
Cardiovascular system
Blood
Pressure
Diastolic: The lowest pressure between heartbeats
Systolic: The highest pressure when the heart beats
Flow
Factors effecting blood flow
Viscosity
incr in viscosity = decr cardiac output
Length
Shorter vessel length = better flow
Diameter
Greater diameter = better flow
Friction force
Less friction = better flow
Pressure gradient
high to low pressure
temperature regulation
pathogen defense
remove metabolic waste
Transport vital substances
Physiology of the heart
Heart sounds
Second sound
Semilunar valves closing
First sound
AV valves closing
Cardiac output
Factors
Neural influence
SNS
Increases HR and contractility (Epi and norepi)
PNS
Reduces HR (acetylcholine)
Venous return
skeletal muscle pump, respiratory pump
Frank-Starling
Incr stretch= incer contraction force
Equation
HR x SV
Stroke volume
Amount of blood pumped by one ventricle in contraction
ejection fraction - % of EDV ejected with one
contraction
Cardiac cycle
EKG
T wave
Ventricular repolarization
QRS complex
Ventricular depolarization
P wave
Atrial depolarization
Phases
Isovolumetric relaxation
residual blood remains (end systolic volume
all valves closed
ventricles relax
Ventricular ejection
blood is ejected into arteries
Semilunar valves are open
Isovolumetric ventricular contraction
all valves are closed (no ejection)
ventricles contract
Atrial systole
additional blood enters ventricles
atria contracts
Late diastole
both atria and ventricle are relaxed
Mechanical events
Diastole
passive filling of ventricles
70% of blood volume
Relaxation
Systole
Atrial kick
Contraction
Conduction system
Bundle of His and purkinje fibers
spread electrical signal to ventricles
Av node
Subtopic
Slows down conduction to allow atrial contraction
SA node
initiates depolarization and sets HR
right atrium
cardiac cells
types
Contractile
99%
-90 mV resting membrane potential
respond to action potentials
Autorhythmic
-60mV pacemaker potential
1%
Generate action potentials
Characteristics
Contractility
Cardiac contractility is the heart's ability to contract and pump blood. It's also known as inotropy.
Conductivity
The heart's conductivity refers to the ability of its cells to generate and conduct electrical impulses that control the heartbeat:
Excitability
Cardiac excitability is the ability of heart cells to depolarize and repolarize and to propagate electrical activity to other cells
Rhythmicity
The heart's rhythmicity is the ability of the cardiac muscle to depolarize and repolarize in a stable and repetitive manner
Automaticity
The heart's automaticity is the ability of cardiac cells to spontaneously generate electrical impulses, or action potentials without external stimulation
Anatomy of the heart
Valves
Aortic
Aortic valve: Located between the left ventricle and aorta
Mitral/bicuspid
Mitral valve: Located between the left atrium and left ventricle
Pulmonary
Pulmonary valve: Located between the right ventricle and pulmonary artery
Tricuspid
Tricuspid valve: Located between the right atrium and right ventricle
Chambers
L ventricle
Left ventricle: Pumps oxygenated blood to the aorta, which distributes it to the rest of the body
L atrium
Left atrium: Receives oxygenated blood from the lungs through the pulmonary veins
R ventricle
Right ventricle: Pumps blood to the lungs to receive oxygen
R atrium
Right atrium: Receives blood from the body that's low in oxygen
Endocardium
keeps the blood flowing through the heart separate from the myocardium, or cardiac muscles
Myocardium
Coordination: The myocardium contracts in a coordinated fashion to resist fatigue.
Force generation: The myocardium generates enough force to supply the body's metabolic demands.
Contraction: The myocardium contracts and relaxes rapidly and involuntarily to pump blood throughout the body.
Pericardium
positions the heart in the mediastinum and limits its motion while providing a lubricated slippery surface for the heart to beat inside and the lungs to move outside
Major vessels
Pulmonary Veins
the right pulmonary vein carries oxygenated blood from the right lung to the left atrium
The left pulmonary vein carries oxygenated blood from the left lung to the left atrium of the heart
Pulmonary trunk
R pulm artery
Supplies blood to right lung
L pulm artery
Supplies blood to left lung
Inferior VC
Superior VC
The right and left brachiocephalic veins join to form the SVC
In the superior and middle mediastinum
R coronary
Marginal
supplies the majority of the myocardium of the right ventricle of the heart.
supplies blood to the bottom of the heart
L coronary
circumflex
Supplies oxygenated blood to the left atrium and the back and outer areas of the heart's left ventricle
Ant interventricular
supplies blood to the left ventricle, the interventricular septum, and a small section of the right ventricle's outflow tract
L subclavian
supply oxygen-rich blood to the upper body, including the left arm, neck, head, and back of the brain
L common Carotid
supplying oxygenated blood to the head and neck
R Brachiocephalic Trunk
R subclavian
supply oxygen-rich blood to the right upper extremity
R common carotid
Supplies blood to brain
openings
Aortic Hiatus
Azygos vein
Part of the azygos venous system, which helps circulate blood and deliver oxygen and nutrients to tissues. The azygos vein also creates a collateral pathway between the superior vena cava (SVC) and the inferior vena cava (IVC).
Located on the right side of the middle back of the chest, along the right side of the vertebral column
Desc. Aorta
The descending aorta is the part of the aorta that runs from the aortic arch down through the chest and into the abdomen:
Esophageal opening
Vagal trunks
Posterior vagal trunk
Supplies the foregut and midgut with visceral sensory and parasympathetic innervation.
Anterior vagal trunk
Supplies the abdominal esophagus, cardia, lesser curvature, and superior portion of the stomach. It also branches into the hepatic branch, which supplies the liver, gallbladder, and biliary apparatus.
move food and liquids from the mouth to the stomach.
Caval opening
T8
Inferior Vena Cava
L/R crus and arcuate ligaments
Left crus: Originates from the upper two lumbar vertebrae and intervertebral discs.
Right crus: Originates from the first three lumbar vertebrae and intervertebral discs
Central tendon
The vena caval foramen is an opening in the central tendon that allows the inferior vena cava and right phrenic nerve to pass through.
During inhalation, the central tendon is pulled down by the diaphragm, which expands the chest cavity and allows air to enter the lungs.
The central tendon is made up of multiple planes of fibers that intersect at various angles to form bundles that give it strength.
L/R Phrenic nerve
R
Right phrenic nerve: Controls the right side of the diaphragm
L
Left phrenic nerve: Controls the left side of the diaphragm
Mediastinum
The ascending aorta is a key part of the circulatory system, helping the heart pump blood throughout the body.
The ascending aorta is the initial portion of the aorta that extends behind the sternum, ending at the level of the T4 vertebral body.
The descending aorta is the part of the aorta that runs from the aortic arch down through the chest and into the abdomen:
Thoracic duct
courses posterior to the esophagus at the T7 level and crosses over the midline to the left side of the thorax around the T5 vertebral level.
The thoracic duct's primary function is to transport lymph from the body's tissues into the circulatory system:
Internal thoracic
vein
Deep in the chest, near the sternum
collects blood from the chest wall and breasts and returns it to your heart
artery
The ITA terminates at the level of the sixth rib, dividing into the superior epigastric and musculophrenic arteries.
The ITA originates from the subclavian artery, a few centimeters below the origin of the thyrocervical trunk.
The ITA runs along the inner surface of the anterior chest wall, about 2–3 centimeters from the sternum and slightly medial to the nipple.
Vagus nerve
The phrenic nerve originates from the C3 through C5 nerve roots in the spinal cord.
The phrenic nerve travels through the neck and chest, past the heart and lungs, to reach the diaphragm.
The phrenic nerve controls the diaphragm's contraction and relaxation and provides sensory information about touch and pain to the diaphragm and surrounding tissues.
Sympathetic chain
network of nerve fibers that runs parallel to the vertebral column on either side of the body
Function: Carries preganglionic fibers from the spinal cord that synapse in ganglia, which then send postganglionic fibers to the viscera
Regions: Divided into cervical, thoracic, lumbar, and sacral segments
Structure: Consists of 22 pairs of interconnected neuronal cell bodies
Location: Extends from the base of the skull to the coccyx
The esophagus is a muscular tube in the center of the chest that connects the throat to the stomach:
The esophagus is located in the mediastinum, behind the trache and in front of the spine. It passes through the diaphragm and enters the abdominal cavity.
Lubrication: The esophagus produces mucus to help food pass through.
The esophagus's primary function is to move food and liquids from the mouth to the stomach
Trachea
Larynx: The upper part of the trachea that contains the vocal cords.
Cricoid cartilage: A ring of cartilage that surrounds the trachea in the middle of the neck.
Mucosa: A substance that lines the cartilage rings.
Cartilage rings: The trachea is made up of circular cartilage rings that support the trachea and prevent it from collapsing when you exhale.
location
The trachea is located in the neck and upper chest, between the collarbones and below the larynx
Cartilage support
Air filtration
Disease defense
Temperature regulation
The trachea's primary function is to allow air to pass into and out of the lungs.
Thymus gland
The thymus gland is located in the upper chest, in the mediastinum, between the lungs, and in front of and above the heart:
The thymus gland's main function is to produce and mature T cells, a type of white blood cell that helps the body fight infection:
Great Vessels
The IVC's main function is to return blood from the lower body to the heart. The heart then pumps the blood to the lungs to pick up oxygen.
The IVC is located along the right side of the vertebral column and passes through the diaphragm.
Superior vena cava
The right and left brachiocephalic veins join to form the SVC
In the superior and middle mediastinum
Carries blood from the head, neck, arms, and chest to the heart
Aortic Arch
Distributes blood to the head and upper body, and helps regulate blood pressure
Between the ascending and descending aorta in the upper mediastinum
Pulmonary A/V
Pulm A
transport deoxygenated blood from the right side of the heart to the lungs for oxygenation
Pulm V
The pulmonary veins carry oxygen-rich blood from the lungs to the heart, where it is then pumped to the rest of the body
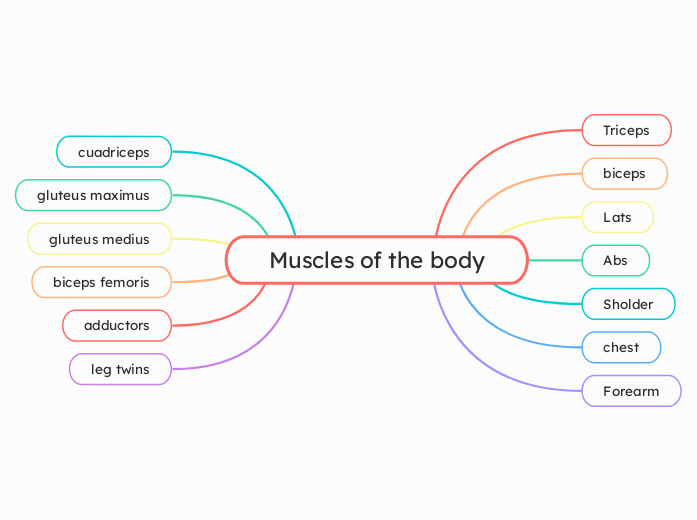
Rib cage
Scalenes
act as postural muscles in maintaining the position of the cervical tract or playing an active role in the movements of the neck
Posterior - 2nd rib
Anterior middle- 1st rib
Transversus thoracis
Helps to depress the ribs during forced exhalation
Located on the inner surface of the anterior thoracic wall
Innermost intercostals
They stabilize the ribs during normal breathing and depress the ribs during forced exhalation.
They are found in the middle two-thirds of the intercostal spaces, deep to the internal intercostal muscles and intercostal vessels and nerves.
Internal intercostals
The internal intercostal muscles contract to depress the ribs and push air out of the lungs during forced exhalation. They are also important for normal speech and singing.
The internal intercostal muscles are located in the middle of the three intercostal muscle layers in the thorax, deep to the external intercostal muscles. They extend from the front of the ribs, around the back, and past the bend in the ribs.
External intercostals
When you inhale, the external intercostal muscles contract, which raises and spreads the ribs apart, expanding the chest cavity and allowing the lungs to fill with air.
The posterior intercostal veins are a set of veins that drain the back of the thoracic cavity:
Neurovascular supply
Posterior intercostal vessels
Posterior intercostal vein
The posterior intercostal veins are a set of veins that drain the back of the thoracic cavity
Posterior intercostal artery
The posterior intercostal arteries are a set of blood vessels that supply the chest wall, back, and spine:
Intercostal nerves: ventral rami of T1-T12
Paired internal thoracic artery and veins
small paired vessel that drains blood from the chest wall, breasts, diaphragm, and part of the mediastinum back to the heart
a paired artery that supplies blood to the anterior chest wall, breasts, and upper abdomen
Paired ribs
11-12 are floating and not attached to anterior rib cage
8-10 articulate with cartilage superior to them
Ribs 1-7 attach to sternum via cartilage
Angle of rib
located lateral to the tubercle and is marked by a prominent linear ridge on the ribs external surface
an area of the body of tenth rib where its curvature changes sharply
Costal groove
provides an attachment site for the innermost intercostal muscle.
Superior aspect for neruo structures
Shaft
The shaft of the rib cage is the body of the rib, which is a flat, curved, and thin bone
Tubercle
Attach to transverse process of T vertebrae
The neck of a rib is the flattened part that connects the head of the rib to the body, or shaft
Head with 2 articular facets
Atypical
1,2,11,12
Typical
3-10
Boundaries of thorax
12 thoracic vertebral bodies
Sternum
Xiphoid process
Manubrium
Lateral
Ribcage
1st rib
Abdomen
Quadrants
LLQ
sigmoid colon, part of the descending colon, the left ovary (in females), the left fallopian tube (in females), the left ureter, portions of the small intestine (especially the ileum), and various blood vessels and lymphatics, including branches of the abdominal aorta and iliac arteries.
cecum, appendix, right ovary (in females), right fallopian tube (in females), right ureter, the lower pole of the right kidney, portions of the ileum (small intestine), and various blood vessels and lymphatics, including branches of the abdominal aorta and iliac arteries.
left portion of the liver, the larger portion of the stomach, the pancreas, left kidney, spleen, portions of the transverse and descending colon, and parts of the small intestine
right portion of the liver, gallbladder, right kidney, a small portion of the stomach, portions of the ascending and transverse colon, and parts of the small intestine
Peritoneum & Peritoneal Cavity
Subdivisions
Omental bursa
Allows stomach to move freely
Omental foramen
allows communication between the greater and lesser sacs of the peritoneal cavity
Formations
Omentum
Connects liver to stomach
Fat deposition, having varying amounts of adipose tissue. Immune contribution, having milky spots of macrophage collections. Infection and wound isolation
Mesentery
The mesentery is a fold of membrane that attaches the intestine to the wall around the stomach area and holds it in place.
The inner layer that covers the lungs, blood vessels, nerves, and bronchi
Parietal
The outer layer that attaches to the chest wall.
Diaphragm
dome-shaped muscle that separates the thoracic cavity from the abdominal cavity
Actions
Exhale
When the diaphragm relaxes, it moves upwards, compressing the chest cavity and pushing air out of the lungs.
Inhale
When the diaphragm contracts, it moves downwards, creating a vacuum in the chest cavity that pulls air into the lungs.
Nerve
Phrenic nerve
Sensory: The phrenic nerve provides sensation to the central tendon of the diaphragm
Motor: The phrenic nerve causes the diaphragm to contract when you inhale
C3 through C5
Lower internal intercostal arteries: Supply blood to the diaphragm
Inferior phrenic arteries: Often arise from the anterior trunk of the aorta above the celiac artery
Pericardiacophrenic artery: A branch of the internal thoracic artery
Musculophrenic artery: A branch of the internal thoracic artery
Superior phrenic arteries: Arise from the thoracic aorta
Anterio-lateral Abdominal Wall
Inuinal region
Inguinal canal
walls
Roof
formed by the medial crus of the aponeurosis of the external oblique, the musculoaponeurotic arches of the internal oblique and transverse abdominal muscles, and the transversalis fascia.
formed by the transversalis fascia, conjoint tendon, and deep inguinal ring.
Anterior
composed of the aponeurosis of the external oblique muscle and reinforced laterally by the internal oblique muscle.
Floor
lancunar ligament
superficial ring
The exit point for the inguinal canal, which allows passage for the spermatic cord in males, the round ligament in females, blood vessels, lymphatics, and the ilioinguinal nerve
Location: Located above the pubic tubercle, just superior to the crest of the pubis
Deep ring
serve as the entrance point of the inguinal canal, allowing the passage of the spermatic cord in males and the round ligament of the uterus in females
It is an opening in the transversalis fascia, forming the deep boundary of the inguinal canal.
Iliopubic tract
The iliopubic tract is a band of tissue that runs from the iliopectineal arch to the pubic bone
Inguinal ligament
The inguinal ligament is a band of tissue that runs from the pubic tubercle to the anterior superior iliac spine (ASIS) in the lower abdomen.
It's also known as Poupart's ligament or groin ligament
Spermatic cord
Lymphatic vessels
Fight infection
The lymphatic vessels of the scrotum drain into the superficial inguinal lymph nodes.
Cremaster muscle
raise and lower the testes in order to regulate scrotal temperature for optimal spermatogenesis and survival of the resultant spermatozoa.
Plexus
Helps regulate temperature
web-like network of veins in the spermatic cord that surrounds the testicular artery. It begins in the scrotum and extends into the inguinal canal.
Arteries
testicular
Also known as the internal spermatic artery, this artery branches from the abdominal aorta and supplies blood to the testis, epididymis, and spermatic cord.
cremasteric
A branch of the inferior epigastric artery, this artery supplies blood to the skin of the scrotum, including the cremaster muscle, and the layers of the spermatic cord.
Ductus deferens
Runs through the spermatic cord, inguinal canal, and pelvic cavity, looping over the bladder and ending at the ejaculatory duct
Carries sperm from the epididymis to the urethra
Layers
External spermatic fascia
Internal spermatic fascia
Neruovasculature
femoral artery
superficial circumflex
supplies blood to the skin, subcutaneous tissue, and superficial inguinal lymph nodes of the abdominal wall and groin
superficial epigastric
The superficial epigastric artery's main function is to supply blood to the skin and superficial inguinal lymph nodes of the anterior abdominal wall
External iliac
deep circumflex iliac
The deep circumflex iliac artery (DCIA) supplies blood to the muscles, skin, and bone of the lower abdomen and pelvis
inferior epigastric
The inferior epigastric artery supplies oxygen-rich blood to the abdominal wall, including the skin, muscles, and parts of the male reproductive system
Aorta
subcostal
The subcostal arteries supply the muscles and skin beneath the 12th rib of the anterolateral abdominal wall
posterior epigastric
Supplies blood to the upper part of the rectus abdominis muscle and the linea semilunaris
Internal Thoracic
superior epigastric
The superior epigastric artery supplies blood to the upper central abdominal wall and skin, and the upper rectus abdominis muscle:
musculophrenic
The musculophrenic artery is a branch of the internal thoracic artery that supplies the pericardium and abdominal wall:
Ilioinguinal
Iliohypogastric
Lateral cutaneous
T7-T9
Thoracoabdominal
T7-T12
Internal surface
Peritoneal fossae
supravesical
medial inguinal
Lateral inguinal
Peritoneal folds
Lateral umbilical
Median umbilical
Transverse section
Below umbilicus
Rectus sheath anterior to rectus
Above umbilicus
Rectus sheath splits around the rectus
Rectus shealth
fibrous compartment in the abdomen that contains the rectus abdominis and pyramidalis muscles
Pyramidalis
Function: Considered to have a minor role in stabilizing the abdominal wall by tensing the linea alba
Found at the base of the pubic bone, within the rectus sheath, anterior to the rectus abdominis muscle.
Rectus abdominis
Flexion of the spine
move the body between the ribcage and the pelvis.
Transversus abdominus
postural support and help contain and support the organs inside the trunk. It's also a main core muscle that supports the lumbopelvic region.
located between the ribs and pelvis, and wrapping around the trunk from front to back.
Internal oblique
The internal obliques work with the external obliques to help the trunk twist and turn. They also help with exhaling and stabilizing the spine.
The internal obliques are located on the sides of the trunk, just inside the hip bones, and on top of the external obliques.
External oblique
The external oblique's primary function is to rotate the trunk from side to side. It also helps stabilize the core, move the spine, and assist with breathing.
The external oblique is one of the outermost abdominal muscles, located on the sides of the abdomen, and sits on top of the internal obliques.
Fascia
Scarpa
allow for smooth movement, protect the underlying organs, provide structural support to the abdominal wall, role in maintaining fluid balance and tissue pressure in the region.
Scarpa's fascia is a thin membrane of connective tissue located in the lower abdomen and anterior abdominal wall:
Intermediate
Abdominal
attaches, stabilizes, encloses, and separates muscles and other internal organs.
The TLF supports the lower back, helps maintain spinal alignment, and protects the underlying muscles and spinal structures. It also contains nerve endings that help with proprioception, the body's ability to sense its position and movement.
Located on either side of the lumbar vertebrae, the TLF is most prominent in the upper lumbar region.
Camper
Extends from the xiphoid process to the inguinal ligaments, and past the pubic symphysis
Protects the abdominal organs, insulates to maintain a constant temperature, and separates the skin from the muscles
Posterior Abdominal Wall
Lymphatics
deep
Iliac
Follows the deep circumflex iliac artery and drains into the external iliac nodes
Lumbar
Follows the lumbar arteries and drains into the lateral aortic nodes
super
Follow the superficial circumflex blood vessels in the lumbar and iliac regions
Inferior vena cava
A large vein that receives venous drainage from all structures below the diaphragm. It's located on the posterior abdominal wall, to the right of the abdominal aorta and in front of the vertebral column.
Abdominal aorta
T12
The abdominal aorta is a large blood vessel that runs along the posterior abdominal wall, supplying blood to the abdomen and other parts of the body:
Muscles
Quadratus lumborum
The quadratus lumborum (QL) muscle is innervated by the subcostal nerve (T12) and the first three nerves of the lumbar plexus (L1-L3):
extensor of the lumbar spine, a stabilizer of the lumbar area, capable of pelvic tilting laterally and capable of acting as an inspiratory accessory muscle.
Iliacus
femoral nerve (L2–L4).
flexes and rotates the thigh bone
Psoas major
Hip flexion and external rotation
T12–L5.
L1-L4 spinal nerves and sometimes includes T12
The nerves of the posterior abdominal wall primarily originate from the lumbar plexus
Fasica
Thoracolumbar
The TLF spans the length of the back, from the neck to the sacrum. It's most developed in the lumbar region.
The TLF has three layers: anterior, middle, and posterior. The posterior layer extends from the neck to the loin, while the anterior and middle layers are limited to the lumbar region.
Psoas
The psoas fascia is a thick layer of connective tissue that covers the psoas major muscle in the posterior abdominal wall:
Abdominal Viscera
Kidney
Glands
Produce hormones that control many important body functions, including blood pressure, blood sugar, metabolism, and the body's response to stress
Afferent
These nerves travel from the kidney to the dorsal root ganglia along the spinal cord. The least splanchnic nerve is the primary afferent signaling nerve from the kidney to the brain.
Efferent
These nerves are sympathetic and originate from the neuraxis.
regulate renal function, including sodium reabsorption, glomerular filtration, and renin release.
Renal veins
carry filtered blood from the kidneys to the heart:
Renal arteries
supply oxygenated blood to the kidneys, adrenal glands, and ureters
Minor Calyces
Major Calyces
Renal pyramids
Renal pelvis
Renal hilum
remove waste products from the blood and produce urine. control blood pressure.
Pancreas
sympathetic innervation from the greater and lesser splanchnic nerves (T5-T12).
The pancreas receives involuntary innervation via the autonomic nervous system (ANS). Its parasympathetic innervation originates from the vagus nerve (CN X)
gastroduodenal
A small vessel that supplies blood to the head of the pancreas, the pylorus, and the proximal part of the duodenum.
superior mesenteric
A major blood vessel in the digestive system that supplies oxygenated blood to the pancreas and the lower parts of the intestine.
Transverse pancreatic artery
Also known as the inferior pancreatic artery, it supplies the pancreatic tail and body. It originates from the proximal splenic artery.
Dorsal pancreatic artery
A branch of the splenic artery that supplies the pancreas. It runs along the posterior margin of the pancreas and divides into left and right branches.
Greater pancreatic artery
The largest blood vessel that supplies oxygenated blood to the pancreas. It originates from the splenic artery.
Ducts
Accessory pancreatic
secondary drainage system for the main pancreatic duct, which can help reduce pressure and prevent acute pancreatitis.
Main pancreatic
drains pancreatic fluid from the pancreas, which contains digestive enzymes and fluids that help break down food.
Parts
Tail
Neck
Head
Endocrine
produce and release hormones that regulate blood sugar levels:
Exocrine
secretion of digestive enzymes, ions and water into the duodenum
Spleen
The vagus nerve (CN X) provides parasympathetic innervation to the spleen.
The celiac plexus provides sympathetic innervation to the spleen.
Splenic artery
supplies oxygenated blood to the spleen, stomach, and pancreas:
Splenic vein
carries blood from the spleen, pancreas, and part of the stomach to the liver
located in the upper left quadrant of the abdomen, behind the stomach and under the left ribs
Stores and filters blood
Gall Bladder
Location
RUQ
gastrointestinal organ located within the right hypochondrial region of the abdomen.
Stores bile
Liver
Parasympathetic nerves:
Originate in the dorsal motor nucleus of the vagus nerve in the brainstem.
Sympathetic nerves
Originate in the celiac and superior mesenteric ganglia, which receive pre-ganglionic neurons from the spinal cord.
Hepatic portal vein
a vein conveying blood to the liver from the spleen, stomach, pancreas, and intestines.
Left hepatic vein
Located between the left medial and left lateral sectors
Middle hepatic vein
Located between the right anterior sector and segment IV
Right hepatic vein
Located between the right anterior and right posterior sectors
Lobes
Caudate
between the left and right lobes, and in an anterior and superior position
Quadrate
Located on the inferior surface of the right lobe
Smaller than the right lobe
The largest lobe of the liver
Visceral
posteroinferior surface that faces the abdominal organs and other adjacent structures
Diaphragmatic
fits under the vault of the diaphragm which in front separates it on the right from the sixth to the tenth ribs and their cartilages, and on the left from the seventh and eighth costal
filters all of the blood in the body and breaks down poisonous substances, such as alcohol and drugs
Large Intestine
Cecum
connects the small intestine to the colon
Features
Omental Appendices
made of fat and the peritoneum, a serous tissue that lines the abdominal wall and covers most abdominal organs
Teniae Coli
Shorten the colon wall to create haustra
Run the length of the ascending, transverse, descending, and sigmoid colons
Haustra
slow down the movement of digested food through the colon
Pelvic
controls the lower part of the GI tract, including the rectum and anus
Vagus
regulates tone and volume in the large intestine
Veins
Inferior mesenteric vein
Drains the descending colon and sigmoid colon
Superior mesenteric vein
Drains the ascending colon, transverse colon, and ileocolic vein
inferior mesenteric artery (IMA)
Rectum
responsible for storing feces and then moving it toward your anus
Appendix
attached to the large intestine
LRQ
Colon
Sigmoid
Usually in the pelvis, but can become displaced into the abdominal cavity
Stores fecal matter until it's ready to leave the body
Transverse
Between the right and left colic flexures, usually at the level of the 10th rib
left side of the body, between the transverse colon and sigmoid colon
runs superiorly on the right side of the abdomen from the right iliac fossa to the right lobe of the liver
Right side of the abdomen
forming and propelling feces toward the rectum
producing and absorbing vitamins
absorbing water and electrolytes
Small Intestine
Superior mesenteric vein (SMV)
Drains blood from the small intestine
Superior mesenteric artery (SMA)
supplies oxygenated blood
Auerbach's myenteric plexus
sympathetic and parasympathetic
Meissner's plexus
parasympathetic input
Ileum
RLQ
receives blood supply from the superior mesenteric artery
contains finger-like projections called villi that increase the surface area for nutrient absorption
has a mucosa (inner lining), submucosa, muscularis externa (muscle layer), and serosa (outer layer)
Jejunum
LUQ
Attached to a long mesentery, allowing for mobility within the abdominal cavity
circular folds in its submucosa called plicae circulares
Duodenum
Ascending
Ligament of Treitz
anchors the duodenum
L2-L3
Inferior
L3
Descending
Ampulla of Vater
Where the pancreatic and bile ducts meet to release digestive juices into the small intestine
Major duodenal papilla
allows bile and pancreatic enzymes to flow into the duodenum
L1-L3
Superior
L1
break down food, absorb nutrients the body needs, and excrete unnecessary components
Stomach
Anatomy
Curvatures
Lesser
Greater
Sections
Cardia
Fundus
Body
Pyloric
Vessels
Arterial
Celiac Trunk
Gastric
Left
supplies the lower esophagus and part of the stomach
Short
supply blood to the fundus and proximal body of the stomach, including the cardiac orifice
Posterior
Supplies blood to the superior and posterior regions of the stomach, near the border of the cardia and fundus
Right
supplies blood to the lesser curvature of the stomach
Venous
Short gastric
Drain into splenic vain
L & R gastric veins
Drain into portal vein
Nerves
Parasympathetic
Sympathetic
Greater splanchnic nerve
T6-T9
Cardiac plexus
influences gastric function by regulating motility and acid secretion in the stomach
Function
Churns the food to help break it down mechanically and chemically
Esophagus
Passes through the thoracic cavity and into the abdomen
Neuro Vasculature
The vagus nerve is the primary motor nerve of the esophagus
Innervated by the sympathetic and parasympathetic divisions of the autonomic nervous system
Structure
Adventitia (outer connective tissue layer)
Muscularis propria (muscle layer with inner circular and outer longitudinal fibers)
Submucosa (connective tissue layer)
Mucosa (inner lining)
Functions
Vomiting, eructation, and the gag reflex
Transport food and liquids from the mouth to the stomach
Prevent food and liquids from entering the windpipe or nasal cavity