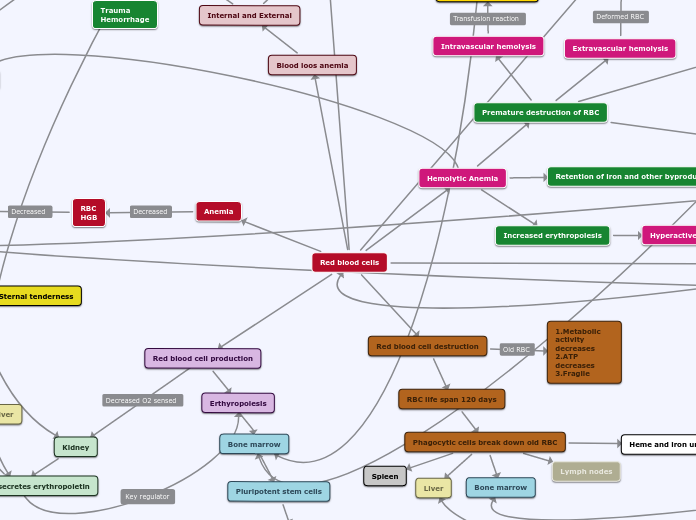
Hematology
1:48anemia
Auto Hemolysis
cold antibod.
poor tx
warm antibod.
immunosuppresion
indirect coombs
measures the antibodies in the serum. direct coombs
tests the antibodies attached to the RBC: adds antibodies for the antibodies--> agglutination if pos.PNH
present
changes into aplastic anemiathrombosis
hemolysis
androgen
steroid
flow cytometry
CD55: decay accelerating factor DAFCD59 homologous restriction factor HRFolder tests as sucrose hemolysis and HAM tests are abandonedthalmsemia
major
anemia with massive hepatosplenomaegalygenetic testsminor
presents like iron deficiency with microcytic anemia but it does not response to Fe. also has inc. reticulocytes unlike Fe anemiaElectropherisis: > 3% A2SC
trait
diluted urine
SCD
clinincal
aplastic crisis
inc. hg F and so protects from cirisisexchange transfusion
for acute crisis or chronically post the attack : CVA, chest crisis..transfusion
preferred leukofiltered to reduce allergic reactionaplastic anemia
Cyclosporine clastogenic assay to differentiate from fanconi anemia.acute
Iron def.
treat empirically without further tests.if no responce to treatment, consider thalasemia trait and do electropherisiFe: until Ferritin normailze.Reticulocytosis in 3-7 dsInc. Hg in 2-3 w and normailze in 1 m,avoid tea and soda with meal as it prevents absorptionFe in multivitamin is not sufficient. need 3-6 mg/k and for adult 325 tid.coagulation dis.
thrombophilia
test
factor V lyden
factor V mutation
activated prot C resistance
prot s
free total
prot c
prot c activity
2- clot
coagulation clotFibrinogen turned into Fibrin with the enzyme thrombindeep bleedingTopical thromin
local bleeding, like from a tooth,cryoprecipitate
factor 8 onlyfactor concentrates
1- clot
plts connected to the endothelium through V.W.F forming plt clot,superficial bleedinglow plts
dec. production
BM failure syn
Wiskott aldrich
T cell immuno deficiencyT.A.R
thrombocytopenia + absent radiusFanconi anemia
is insidious , unlike aplastic anemia which is acute.25% don't have the dysmorphic features; the triphalangeal thmbs.Tx
BM transplantDx: DNA breakage test, clastogenic assay DABclinical
insidious; unlike the acute presentation of aplastic anemia75 % have the charachteristic thumbtransient myelodysplasia
mostly in down syn.congenital infection
trapping
vascular
Hemangiomas
Kasabach-meritt synmicro angiopathic dis.
HUS
hypersplenism
auto immune
neonatal
autoimmune destruction like R.H dis. from different maternal -baby genesdrugs
Heparin
can evolve into DICeven from heparin for lines patencyimmunodeficiency
Congenital
AIDS
connective tissue dis
ITP
splenectomy
for chronic ITPplt transfusion
stops the bleeding but does not increase the numberwith BM aspiration
Steroid
steroid is contradicted without BM aspiration because if it was due to leukemia it causes partial treatment and subsequent resistence.the effect is slower than IvIGwithout BM aspiration
IVIG
Winrho
for Rh+ positive onlyworks by overloading the spleen with RBC causing hemolysis so it preserves the pltscauses hemoglubinurea from the hemolysisplt dysfuncion
acquired
NSAID
Myeloproliferative dis
Uremia
congenital
imapired plt adhesion to V.W.F
Bernard Soulier
etio
deficiency in plt glycoprot Ib
impaired adhesion in presen V.W.F
large plt
plt aggregation
Glanzman
deficiency plt glycoprotein IIbb/IIIaVon Welliberand
produced from the endotheliumconnects the plts to the endotheliumbleeding immediatelycarries prot 8. so will results in secondarty low prot VIIIsuperficially bleeding: i.e bleeding into skin and mucosafactor replacement
concentrates are contrandicates b/o they have factor 8 but not V.W.FFFP
cryopreipitate
EACA
Amicar: aminocabroic acid adjunct to DDAVP in the acute bleeding or for shrot period after surgery, 1 week.DDAVP
release v.w.f from endothelium but with limited quantities.good for chronic txcan cause depletion of V.W.F in rare types of the diesease. type 2 bcan be given q 48 hrs; to allow regeneration of VWF stores.nasal DDAVP
can be given after head trauma prophylactically.Blood type O have low normal level of VWconfirrmation
DDAVP stimulation
repeating the tests above before and after DDAVP stimulationquality
in VWF type 2 which is mainly malfunction of the factorPlt functin tests
with epinephrine and collagen
this replaced the old fasioned bleeding time but is more reliable.Ristocetin induced plt aggregation
Ristocetin co factor
testing the function of vwfquantity
Factor VIII
usually low if VWF is low. because VWF is carrier prot for factor 8low factor VIII level
prolonged PTT
VWF titers.
Multimer analysis
Immuno electropheresis
Onc
Solid tumors
Ewing sarcoma
systemic inflammatory
painful mass in mid bone
osteogenic sarcoma
high ALphosphatase
pathologic fx
painless lesion in distal bone
60% at the knee
Retinoblastoma
prog
secondary tumor: osteogenic sarcoma
25 % b/l
strabismus and impaired vision
glucoma
photophobia in neonate and tearing.diff
congenital glucoma
wilm's
IVP or CT shows distorion of the kidney calicyles unlike neuroblastoma which showes displacement.Prog
associated syn
Beckwith Wiedman syn
NF
hemihypertrophy
aniridia
Neuroblastoma
< 1 yr. good
spontaneus recovery
ferritin
blasts on peripheral smear
catecholamines
Diarrhea
HTN
Opsoclonus
periorbital ecchymoses
legs pain
MDS
pre leukemiclab
large plts
dec. retic.
dimorphic RBC
Lymphoma
Secondary malignancy
breast ca
labs
Cu
ESR
cyclic fever
immunodefciency
lymphdenopathy
above the diaphragm, in contrast to Burkett's. specially the supraclavivular node whick is always considered pathologic mostly T cells.Leukemia
Burkitt's lymphoma
Tumor lysis
Inguinal lymphadenopathy
gerneralized lymphadenopathy in the leukemia/ lymphoma typecervical lymphadenopathy in the african typeAbd mass
intessusception
CML
tx
chemo
interferon
Busulfan
hydroxyurea
because it's stem cell disease.phases
slowly turns into AMLBlast crisis
the terminal phase: massive HSM and lymphadenopathy, anemia and thrombocytopenia accelarated phase
chronic phase
2 yrs. w/o chemo; 4 yrs with chemoBM
philadelphia chromosomeIncre. B12
Low LAP
leukocyte alkaline phosphates LAP: can differentiate between leukocytosis from CML vs sepsis or Leukomoid reaction; latter seen in Down syn,
thromobytosis
basophilia
Neutrophilia
AML
also know as ANLL: acute non lymphocytic leukemiacongenital leukemia
presents in the first month. HSM, infiltration and WBC > 100000dx
DIC
in M3 specially after chemoneed pre treatment with Retnoic acid which matures the PreWBC to neurophilesleukoerythroblastic reaction
auer bodies
in M1 and 2 and 3distinguish primitive WBC from sepsis vs AMLInfiltration
common in type M4 and M5 , the monocyte tumor b/o monocyte existence on tissuresgum hypertrophy
skin and bones
usually facial bonesCNS
Hyperviscosity syn
WBC > 100000especially in M5respiratory distress
blurry vision
headache
ALL
special types
Leukemia lymphoma syn
agressive T cell leukemia
Prognosis
recurrence
testicular recurrence
mediastinal mass
massive lymphdenopathy and HSM
WBC > 100000
hg and platelets normal
treatment
BMT
as last resort after multiple failuremedical
PCP prophlyxis
Dapsone
if allergic to bactrimbactrim
3 ds/weekCNS chemo
Intrathically: first one is rubinoside then MTX after. Repeat x18 over 2 yrs.Chemo
maintenance
30 ms. daily MP6 + weekly MTX + monthly vincristine/solumedrolconsolidation
3-6 msCNS sanctuaryInduction
3 weekly cycles ( vincristine x 4Ds, Dounurubicin X 4 ds, Aspargene x 1d) plus daily steroids.Then BM should be cleared.prognosis
high risk
WBC at diagnosis
> 10000
Age
< 1 or > 10
BM post induction
3
M3: blasts > 25% after the first induction. clears after multiple induction
2
M2: refractory leukemia. failed to induce remission even after multiple chemo
cytometry
Pre B is the most common and best prognosisT cell is more common in older pts.B cell: borkette
Philadelphia chrmosome
polidy: DNA index
presentation
Rehumtoid like dis. responding to steroid
Bone pain
can mimic grwoth pain and responds well to steroids as well; however this results in selecting steroids resistant leukemic cellson xray :new leukemic lines over the metaphisisOrganomegaly
2/3
Lab
initial w/u should include CBC, LDH, Uric acid and ESRsmear
blasts
atypical lymphocytes can mimic blasts: seen in viral infectionsneed manual diff and smear to differentiate bothCBC
WBC
+/- lymphoblastsLow 1/3
High 1/3
normal 1/3
normal
pancytopenia
anemia, thrombocytopenia
others
Neonatal purpura fulminans
prot S or C homozygous
need plasma exchange.sepsis
Tumor lysis syn.
post chemo or spontaneus, specially in Borkette's lymphoma prevention
Hydration and Allopurinol
tx sympt. hypocalcemia
urine ph
keep neutral.acid urine: prevents Ca/Po4 crystalsAlkaline urine: prevents uric acid crystalspresentaion
lytes abnormailties
Ca/Po4
precipitation occur if Ca/PO4 > 60phosphate rises firstHypocalcemia is next.ARF
Arrythmia
Leukorythroblastic reaction
early prematures nucleated RBc and WBC
Dx
tear drop RBC
primitive WBC
nucleated RBC
etiologies
spleenectomy
like in SSDBM failure
RBC then will be formed in other organs like spleen and liver such as in thelasemia.
BM infiltraion
by turmors so it releases early cell linescan see teardrop RBC as well