to treat and prevent amebic liver abscesses
Group A, β-hemolytic Streptococci
α-hemolytic Streptococci
The most common causes of subacute bacterial endocarditis, if introduced into the bloodstream following tooth extraction or tonsillectomy, particularly in individuals with damaged heart valves. That is because they have capability to synthesize dextran from glucose, which allows them to adhere to fibrin-platelet aggregates at damaged heart valves.
Present in large numbers in the mouth, and can cause dental caries.
Viridans Streptococci is a large group of commensal streptococcal bacteria that are α -hemolytic.
Viridans Streptococci
Streptococcus pyogenes.
Prevention of streptococcal infections (usually with benzathine penicillin monthly injection for several years) in persons who have had rheumatic fever is important to prevent recurrence of the disease.
Rheumatic fever can be prevented by prompt treatment of group A streptococcal infection of the throat with penicillin.
Therapy with a combination of vancomycin + aminoglycoside (streptomycin or gentamycin) is essential for severe infections such as endocarditis.
Penicillin is the drug of choice. In cases of allergy, erythromycin is the alternative.
Laboratory diagnosis
Lab diagnosis of post-streptococcal diseases: bacteriological tests are
confirmatory, diagnosis is mainly clinically
Anti-DNase B : high titer , 80 units or more confirm diagnosis of acute glomerulonephritis
. C-reactive protein (CRP):
Presence of CRP together with a high ASO and elevated ESR
(erythrocyte sedimentation rate) help the diagnosis and follow up of
cases of rheumatic fever
Acute phase protein, made in the liver and appears in serum in active
rheumatic fever and in other degenerative and inflammatory
conditions.
Anti-streptolysin O (ASO): high ASO titers 1/200 or more is significant
and indicates recent streptococcal infection.
Diagnosis of streptococcal diseases: practical part
Diseases caused by Str. pyogenes:
Post-streptococcal diseases:
Inflammation is caused by an immunologic (antibody) response to M proteins
Differences between ARF and AGN:
AGN
Majority recover, rarely
chronic GN
Anti-DNase B, CRP, ESR
Not needed
Not common
Less common than ARF
Ag-Ab complex deposition
on glomerular basement
membrane (type III
hypersensitivity)
Nephritogenic strains
2,4,12,49 and 59-61
3 weeks after Str. pyogenes
skin infection (impetigo)
mainly
ARF
Sequelae
Damage to heart muscles and
valves
Diagnosis
ASO, CRP and ESR
Required (long acting
penicillin)
Recurrence
Frequency
More common than AGN
Cross-reactivity between
heart tissue and Abs to M
protein
Strains involved
Rheumatogenic strains
1,2,5,6,18 and other
Occurrence
1-4 weeks after Str. pyogenes
throat infection
and others bearing different M proteins are
nephritogenic and cause acute glomerulonephritis (AGN)
Some strains of Str. pyogenes bearing certain M proteins are rheumatogenic and
cause acute rheumatic fever (ARF)
Disorders in which a local infection with group A Streptococci (pharyngeal or
skin) is followed weeks later by inflammation in an organ that was not infected
by that organism.
Toxigenic diseases:
Necrotizing fasciitis (exotoxin B)
Scarlet fever (exotoxin A)
Streptococcus toxic shock syndrome (exotoxin A and C)
Invasive diseases: are diffusing and rapidly spreading infection e.g. erysipelas,
puerperal sepsis, osteomyelitis and acute bacterial endocarditis.
Pyogenic local infections:
Streptococcal impetigo (pyoderma): a skin infection if caused by
nephritogenic strains , may be followed by acute glomerulonephritis
. Streptococcal sore throat and follicular tonsillitis: rheumatic fever is
its most serious complication .
Virulence factors:
- Pyrogenic exotoxins: there are 3 antigenic types
Pyrogenic exotoxin "c"
Pyrogenic exotoxin "B"
Pyrogenic exotoxin "A" (erythrogenic toxin)
Streptolysins (hemolysins): there are 2 types
Streptolysin "S": Oxygen-stable, and non-antigenic. Responsible for
β-hemolysis
Streptolysin "O": Oxygen-labile and antigenic. The antibody (ASO)
develops after group A infections. The titer of ASO is used in the
diagnosis of rheumatic fever.
. Invasive Enzymes
Hyaluronidase: It is a spreading factor that degrades hyaluronic acid
in between cells
DNase (sterptodornase): degrades the DNA in necrotic tissue or exudate,
thus promoting the spread of infection.
Streptokinase (fibrinolysin): dissolves fibrin in clots, thrombi, and
emboli. It can be given intravenously for treatment of pulmonary emboli
and coronary artery thrombi.
M protein:
Some M types are rheumatogenic, while others are nephritogenic.
Str. pyogenes has over 150 distinct M types
It is the most important virulence factor as it is antiphagocytic.
Culture: Facultative anaerobes, β-hemolytic
✔ Morphology: Gram-positive cocci arranged in chains.
Colonizes the upper respiratory mucosa, especially the oropharynx
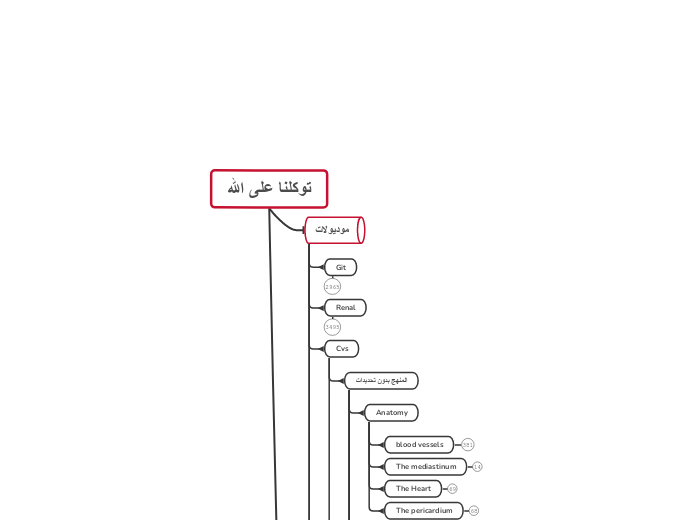
توكلنا على الله
مواد
فارما git
Therapeutic strategies for GERD & peptic ulcer
# [introduction to pharmacology](https://www.mindmeister.com/2523269469)
- purpose of application
- agricultural
- genetics
- toxicolog
- clinical
- techniques used
- behavioral
- immuno
- biochemical
- molecular
- organ system
- pulmonary
- renal
- cardiovascular pharmacology
- neuropharmacology
- key terms
- Steady-state concentration
- elimination half life
- plasma half life
- Lethal dose LD50
- Effective dose ED50
- Therapeutic index
- Potency
- mitigation
- Divisions
- pharmacokinetics
- elimination
- excretion
- lungs
- sweat
- breast milk
- intestinal tract
- bile and feces
- kidneys
- urine
- metabolism
- if the drug is metabolized, it may be
- inactivated
- chloramphenicol
- alcohol
- phenytoin
- maintained active
- digitoxin to digoxin
- amitriptyline to nortriptyline
- diazepam to desmethyl diazepam
- activated
- methyldopa to alpha-methyl nor adrenaline
- levodopa to dopmine
- distribution
- binding to drug carriers
- binding affinity
- lithium 0%
- morphine 35%
- warfarin 99%
- alpha-1-acid glycoprotein
- protase inhibitors
- steroids
- basic drugs
- Albumin
- acidic drugs
- organs that receives most of the drug initially
- kidney
- brain
- rate-determening factors
- binding to plasma protein
- lipid solubility
- regional blood flow
- cardiac output
- absorbtion
- Bioavailability
- Bioequivalence
- 100% bioavailability
- None-intravenous administration
- reduced due
- First pass effect on the liver
- inactivation within the GIT
- bacteria
- digestive enzymes
- Gastric acid
- Relative bioavailability
- compared with a another
formulation or standard
- Absolute bioavailability
- compared to IV administration
- AUC oral / AUC i.v x 100%
- factors affecting absorption
- physiochemical factors
- Plasma protein binding
- Dosage form
- Lipid solubility
- Particle size
- physiological factors
- Gastro-intestinal blood flow
- Area of absorption surface
- Metabolism
- Food
- Gastric pH
- Intestinal motility
- Gastric emptying
- involves passage through
- endocytosis
- facilitated diffusion
- active transport
- filtration
- passive diffusion
- Routs of administration
- Parenteral
- Inhalation
- Topical
- enema
- ear drops
- eye drops
- Cream or lotion
- intravenous
- Enteral
- gastric feeding tube
- oral
- Pharmacodynamics
- Effect
- Action
- classification of drugs
- antagonis
- inhibitor or receptor blocker
- intrinsic activity is 0
- affinity but no efficacy
- inverse agonist
- intrinsic activity is -1
- affinity and negative efficacy
- partial agonist
- pentazocine at meo receptors
- pindolol at beta receptors
- both agonist and antagonist activity
- intrinsic activity between 0 and 1
- affinity but partial efficacy
- agonist
- intrinsic activity = 1
- maximal response
- affinity and efficacy
- Affinity
- Targets
- systemic level
- Tissuey level
- Cellular level
- Molecular level
- receptors
- specialized receptors
- proteins in plasma membrane
- ion channels
- respond to
- growth factors
- autoacoids
- neurotransmitters
- hormons
- generalized receptors
- nucleic acids
- enzymes
- types of actions
- Neutralization
- Chelating agents
- forms complex with heavy metals
- calcium disodium edetate
- antacids
- neutralize gastric acid
- charcoal and kaolin
- adsorption
- Cytotoxic
- antibiotics
- anticancer drugs
- replacement
- iron
- anemia
- insulin
- diabetes millitus
- levadopa
- Parkinsonism
- inhibition
- Theophylline
- inhibits phosphodiesterase
- Digoxin
- inhibits Na-k ATPase
- NSAIDs
- inhibits cyclooxygenase
- Acetazolamide
- inhibits carbon anhydrase
- Allopurino
- inhibits xanthine oxidase
- neostigmine and physostigmine
- inhibit acetyl cholinesterase
- both
- acetylcholine
- depresses SA node in heart
- stimulates intestinal smooth muscle
- depression
- quinidine depresses the heart
- benzodiazepines depresses CNS
- stimulation
- pilocarpine stimulates salivary
glands and GIT
- adrenaline stimulates heart
- Pharmacogenomics
- Pharmacotherapy
- SANE criteria
- Preferred drug
- Efficacy
- Need
- Affordability
- Safety
- Rule of right
- right cost
- right does
- right patient
- right drug
- using drugs to active a therapeutic objective
- General anesthesia
- Supplementation
- Prevention
- Mitigation of pain or fever
- Cure of infection
- Pharmacogenetics
- Pharmacoepidemiology
- Pharmacoeconomics
- Toxicology
- duration of toxicity
- chronic
- sub-acute
- acute
- classification
- other
- chemical structure
- reactivity
- physical state
- lethality
- relatively hermless
- practically non toxic
- slightly toxic
- moderately toxic
- highly toxic
- extremely toxic
- type of effect
- teratogenicity
- mutagenicity
- carcinogenicity
- source
- plant
- animal
- use
- solvents
- food additives
- pesticides
- target organ
- nephrotoxic
- neurotoxic
- hepatotoxic
- cardio toxic
- reversibility
- examples
- CNS
- largely irreversible
- liver
- usually reversible
- depends on capacity of the
tissue to regenerate
- concepts
- groups at highest risk
- common between the two groups
- keys to effective management
- supportive care
- carful attention
- substance and amount are
usually hard to obtain
- adolescence
- mortality and morbidity of poisoning is higher
- large doses and multiple drugs
- intentional
- children1-3 years
- single substance and small amount
- due to hyperactivity and curiosity
- not intentional
- poisoning is the most common
- management concept
- Paracelsus concept
- drugs may have toxic side effects
- toxin
- toxic substance
Cardio vascular pathology
Neoplasms
Inflammatory disorders
Direct infection
Rickettsia
Immunological
Type IV
Graft rejection
ANCA
p-ANCA
Churg-Strauss
Esonophil mediated
Microcropic Polyangiitis
Necrotizing vasculitis
PAN, but involves small vessels
No Temporal Variability in lesions
Hemoptysis
c-ANCA
Type II
Type III
SLE/Rheumatoid arthritis
Drug induced
Hep B induced
All vessels
Kawasaki Syndrome/Mucocutaneous Lymph Node Syndrome
Severe segmental transmural necrotizing destruction
Aneuryms, MI, and thrombosis in children
Autoantibodies against endothelium and SMC
Treat with IVIG
Increase AB clearance
Oversaturate neutrophil Fc receptor
Japanese epidemic
Children
Often affecting coronary arteries
Medium to Small
Wegners Granulotomous
Untreated- Death 1yr
Mucosal ulcerations of nasalpharynx
Chronic sinusitis
Bilateral nodular and cavitar infiltrates
Persistent pneumonitis
M > F around 40
Limited Wegners Granulotomous
No renal involvement but other two classic symptoms
Classic Triad
Focal or Necrotizing Renal Disease
Crescentic Glomerulitis
Focal necrotizing or granulomatous vasculitis
Mainly in lungs
Acute Necrotizing Granulomas of URT and LRT
Burgers Disease/Thromboangitis obliterans
Mainly males
Tibial/Radial arteries
Ulcerations of fingers and toes
extending to V/N
Segmental, thrombosing, acute/chronic inflammation
Granulomatis formation
Thrombosis has microabscesses
Genetic influences
Hypersenstivity reaction to tobacco
Polyarteritis Nodosa
Hemorrhages
Atrophy
Infarcts
Ulcerations
Young Adults
Transmural necrotizing inflammation
Systemic
Temporal Variability
Later Stage
Fibrosis replacement of transmural inflmmation
Acute Stage
Inner half fibrinoid necrosis
Transmural inflammation
Branching points/ Bifurcations
1) Kidney, 2) Heart, 3) Liver, and then 4) GI
Doesn't involve Arterioles, Caps, and Vens (mainly medium)
No glomerulonephritis
Spares pulmonary circulation
Large-Medium
Takayasu arteritis
Fibrosis involving all layers
Patchy necrosis
Hemiparesis to focal weakness
Dizziness
Low BP Upper limbs
Upper limp pulselessness, coldness, and numbness
Blindness
Females over 40
Granulomatous vasculitis(media) w/ obliteration of lumen
Pulmonary/coronary/Renal arteries
Arch of Aorta
great vessels of arch
Giant Cell (Temporal) Arteritis
Therapeutic trail of steroids
Papaular nodular temporal artery
50 and above, M:F 1:1
Elastin of Large Arteries
Polymyalgia rheumatica
Elevated ESR (blood sed-rate)
Fragmentation of internal elastic lamina
Granulomatous inflam of intima/ inner media
Temporal artery/ Head
Lead to blindness
Weakening
Aortic Dissection
Retrograde
Aortic Root
disrupt Aortic Valvular apparatus
Type B
Beginning distal subclavian
Type A
Ascending portion/
Ascending + Descending
Most common/
Dangerous
Compress spinal ateries
Transverse myelitis
Adventia
Peritoneal
Pleural
Pericardial
Lumen
"Double bareled" aorta
Arterial cannulation
Men, 40-60
Ruptures
Execruting radiating back pain
First two layers
ascending aorta
Intimal tear
Anyeurms
False/Pseudoaneurysm
Hematoma
True
Saccular
Fusiform
Weakness of Media
Acquired Weakness
Timing of intervention
Over 50% death rate ruptured
5% death rate unruptured
Into retroperitoneal space
Chances increase as size of increases
Large (5cm))-Prostehtic grafts
Occlusion of branch vessels
Renal/Mesenteric/Vertebral
Aysmptomatic
Abdominal mass
Impingement on adjacent structures
Erosion of verebrea
Urter
Distal to renal arteries/Proximal to bifurcation
Age 50 and older
Abdominal aorta
Iatrogenic (disease due to medical treatment)
Encroachment Mediastinum
Respiratory difficulties
Recurrent laryngeal nerve
Persistent Cough
Difficulty Swallowing
Obliterative endarteritis Vaso Vasorum
Tree bark appearance in intima
Aorta Arch
Valve ring dialation
Valvular insufficiency /
most commone cause death
Valvular Regurgation
Massive left vent hypertrophy
Tertiary stage
Mycotic (infective)
Sepsis
Salmonella Gastroenteritises/ Aorta
TB/Bacterial Abscess
Common sites
Splenic
Mesenteric
Cerebral vessels
Congenital
Berry aneuryms
Marfan's syndrome
Narrowing
Brain- infarction/haemorrhage
Eyes- HTN retinopahty
Nephrosclerosis-Kidney
Regulation/ Arterioles
Factors
Blood Volume
Cardiac
Neural
Endocrine
Malignant (210/120)
End organ failure
Stage II (160/100)
Stage I (140-159/90-99)
Arteriosclerosis
Arteriolosclerosis
Necrotizing Arteritiolitis
Fibrinoid Necrosis
Severe Chronic HTN
Response to trauma
Hyaline
Chronic Benign HTN
Plasma protein leakage
Medial Calcific Sclerosis
Atherosclerosis
Locations
Circle of Willis
Internal Carotid
3. Thoracic Aorta, Femoral, Popliteal arteries
2. Coronary Arteries
1. Distal abdominal Aorta
Clinical mainfestations
Peripheral vascular disease
Gangrene
Ischemic Bowel Disease
Cerebreal vascular disease
Chronic ischemic encephalopathy
TIA
Stroke
AAA
Coronary Heart Disease
Angina
Chronic inflammatory response to intima/ Endothliel injury
Stable plaque
Fibrin Cap
Size of nectrocic plaque core
Hemodynamic Stress
Presence of inflammatory cells
Thickness of Cap
Atherosclerotic plaque
Components
Intra/extracellular lipids
ECM
Cells
Hyper thrombotic
Superimposed thrombis
Fatty Streaks
Fatty Dots
Macrophages
TNF
Foam Cells
Major Risk Factors
More impotant after age 45
AS induced gangrene
Cigarette smoking
Hypercholesterolemia
Other associated risk
Chlamydia pneumoniae
High carb diet
Postmenopausal estrogen deficiency
Type A personality
Lack of exercise
C reactive protien
Persistent prothombic events
High PA-1 inhibitor
Lipoprotein (a)
homocystenemia
Folate (B-9) or Colbamine (B-12) defiency
ROS damage
Connective Tissue
Media
Smooth Muscle Cells
Change function upon intima migration
Make Fatty Streak to Fibrofatty atheroma
Elaborate ECM
Vaso- constriction/dialtion
Intima
Dysfunction
Activation
Activators
Viruses
MHC molecues
Bacterial products
Cytokines
Release prothrombin factors
Impaired vasodilation/ anti inflammatory
gene expression/protein synth
Stimulation
Oxidize LDLs
Lipids are cytotoxic to endothelium
Regulate Cell Growth
TGF-Beta
Fibroblast Prolif
PDGF
Inflammatory/Immunity regulation
VCAM1/ ICAM1
IL-6
IL-1
Modulate flow
NO/ Endothelin
Release Anti/Pro thrombic factors
Maintain permeablity
Heart pathology
Vasoconstriction
Stimulated by
A1 Activation
Decrease NO
increase Endothelin
increase Thromboxane A2
Contributes to acute plaque changes
Cornary intraluminal thrombosis
Complete occulsion
Superimposed due to acute plaque changes
Acute plaque changes
Eccentric
Low SMC
Rich lipid and inflammatory cell core
Thin fibrous cap
Stable
Initating event
Rupture/Ulveration
Fixed Coronary obstruction
Critical stenosis
Collaterals
When insufficent leads to disease
70% of 1 or more major coronaries
Increased cardiac demand
Circumflex infarct of heart
Watershed infarct of brain
Hypoxemia
Chronic Ischemic Heart disease
Sudden Cardiac Death
AMI
Dressler's syndrome
Ventricular aneurysms
Mural Thrombi
Rupture
Septum
Acute Heart Failure
Papillary muscle dysfunction
Arrhythmias (75% - 90%)
Not relieved by vasodilators
Gross- Micro Changes
Scarring (2 mths+)
Dense collagenous scar
Firm/Grey, Scarring (2-8 wks)
More collagen than cells
Red/Grey depressed border (10-14 days)
Granulation tissue form
Maximum softening (7-10 days)
Phago/ Hella macs
Central softening/ (3-7 days)
Hyperemic border
Early Macs / Myofibers destruction
Mottling (1-3 days)
PMNs
Dark Mottling (4-24hrs)
Early PMNs/ Coaug Necr/Contraction bands (12-24)
Early Coagulation Necrosis (4-12hrs)
Wavy fibers (1-4hrs)
Myocardial function
Microvascular injury (1hr+)
Loss of ATP from (0-40 mins)
Irreversible injury (20-40 mins)
Loss of contractility (2 mins)
Subendocardial
Can occure with prolonged hypotension
Transmural infarcts
More serious
Other 10% causes
Emboli
Left sided mural thrombus
5:1 M 45-55.....2:1 M 55-80......1:1 80+
Angina pectoris
Unstable
Crescendo pain
Prinzmetal
Relieved by Vasodialators
Coronary artery Spasm
ST segement elevation
Occurs at rest
Typical
Relieved by rest/Vasodialators
Fixed critical stenosis
Physical activity/
emotional excitement
Most Common
Congestive Heart Failure
Systemic Edema
Backward failure
Pulmonary edema
Pulmonary Hypertension
Right Sided failure
Systemic Venous congestion
Foward Heart Failure
Decreased CO
Renal Hypoperfusion
RAS activation
Na+/ H2O retention
Compensatory Mechanisms
Myocardial dilation
Decompensated Heart Failure
Even at rest the heart cant perfuse sufficently for needs
Compensated Heart Failure
Frank Starlings law
Dilation to increase contraction force
Myocardial Hypertrophy
Eccentric hypertrophy
Concentric hypertrophy
Catecholamine stimulation
Types and Causes
Chamber failure
Right sided
Cor Pulmonale (primary lung disease)
Left Sided Failure
Left Sided
Features
Dyspnea
Orthopnea
Paroxysmal nocturnal dyspnea
Ischemic Heart Disease
Mitral/Aortic valve disease
Systemic Hypertension
Diastolic dysfunction
Tamponade
Constrictive Pericarditis
Hypertrophic
Hypertensive Heart Disease
Systolic dysfuction
Cardiomyopathy
Dilated Heart
Volume Overload
MI
Basic info
Blood Supply
Most flow during Diastole
RCA
LCA
LAD
LCrfA
Valves
Aortic/Pulmonary
Open During Styole
2nd Hrt sound
Have Cordae tendineae
Mitral/Tricupsid
Closed During Sytole
First Heart Sound
Layers
Pericardium
Endocardium
Myocardium
Epicardium
Wall thickness
LV:10-15
RV:3-5 mm
Weight
F:200-250
M:250:300
Nephrotic Syndromes
Secondary Amyloid (AA caused)
Hodgkins lymp
Renal cell carcionma
Osteomyelitis
Chrons
Behcet syndrome (systemic inflammation of blood vessels)
RA
Death due to end-organ failure of affected organ
Very poor prognosis
Survival drops severely as yrs pass 50% yr 1 to 5% 10 years
Biopsy needed
Other Systemic Presentations
Skin
Purpura
Easy bruising
Neuro
Orthostatic hypotension
Neuropahty
Ischemic stroke
GI
Hemarrahge
Hepatomegaly
Heart Block
Arrhythmias
CHF
Electrolyte abnormalities
Fanconi's syndrome (loss of renal tubal reabsorptive function)
Renal insufficiency in 50% by diagnosis
Either caused by AL or AA amyloids
Subendothelial/Mesangial fibrils
Congo Red Stain
(+) w/ apple green birefringence
Nodular, amorphous hyaline matierial in mesangium/capillary lopps
Membranous Nephropathy
Subepithelial IC deposits with GBM spike formation
Subepithelial fine granular deposits of IgG/C3 in BM
Diffuse thickening of GBM w/ minor increase in cellularity
Associated Causes
Penicillamine
Gold
Mercury
Captorpril
Malaria
Syphilis
Hep B
Tumors
DNA SLE
Complement Activation
MAC activated damage of GFM
IC deposition
In situ/ cirulating
Heymann Nephritis
Supports in situ
Sub Epithelium
Bad Progonsis
>10gm proteinuria
>50
Males
Presentation
Renal Vein Thrombosis
Late Renal Insufficiency
20 year follow up
25% develop ESRD
50% persistent proteinuria/ stable or gradual loss of renal function
25% spontaneous remission
Microscopic hematuria (50%)
FSGS
Patchy fusion of foot processes/effacement
Negative or Non Specific granular IgM/C3 deposits
Secondary FSGS
Anything that causes a reduction in renal mass
Hyperfiltration Injury
50% recurrence post transplant
ESRD by 5-20 yrs
Persistent proteinuria/progressive decline in renal function
Progresses to Massive Proteinura/Microscopic hematuria
Present asymptomatic proteinuria
Secondary to
Malignancies(lymphoma)
Heroin
Chronic reflux nephropathy
Morbid obesity
Higher incidence seen in adult AA
10-15% of idiopathetic nephrotic syndromes seen in children
Minimal Change
Fusion of foot processes
IF
N
May involve circulating glomerular permeability factors
No immune complex/inflammatory injury
Podocyte
diffuse effacement and detachement
Progression
Adults have worse prognosis
Not likely to progress to CRF/ESRD
1/3 Rule
Many Relaspes
Few Relaspes
No Relaspe
Remission with Steroids within 8 weeks
Labs
Physical Exam
Pedal
Periorbital
No HTN
Bland Urine sediment
Serum
Normal creatinine
Low albumin
Selective protienuria
Can also be seen
Renal cell carcinoma
Children/ 15% in adults
Diabetic Nerophaty
Pathogensis
Systemic hyperglycemia
Timeline
20+ yrs
Decline in GFR 1-24
Median 12
HTN
Persistent heavy proteinuria
10-20 yrs
Macroalbuminuria
Nephrotic syndrome
7-13 yrs
Microalbuminuria
.3- 3g/24 hr
Initially
Increased GFR/ Glomerular hydrostatic pressure
Glomerulosclerosis
Later Lesions
Diffuse global glomerulosclerosis
Hyaline arteriolosclerosis
Ischemia
Tubular atrophy/interstitial fibrosis
Fibrin Cap/Capsular drop
Kimmeslstiel-Wilson nodules
Lipids/Fibrin
More of Early lesions
Earliest lesions
Hyperfiltartion injury
Thickening of GBM
Mesangium epxansion
Reccurance after transplant
Info
Seen in 25-40% of type 1/2 diabetics
Leading cause of ESRD (1/3 of all patients)
Basic presentations
Normal Complement levels
Hyperlipidemia/Lipiduria
Edema
Heavy proteinuria (>3.5gm/day)
Pathology of the Oral Cavity
Oral Lichen Planus
Lips
violaceous or skin colored
5 Ps
Pruritic, Planar, Purple, Polygonal, Papules
Oral mucosa
lacy, white pathches
Wickham's striae
Common
chronic dz
Cheilitis
cheilosis
angular stomatitis
deep cracks
may become infected
may ulcer & crust
may bleed
corner(s) of mouth
Iron
Zinc
B2
riboflavin
Candida (Thrush)
KOH stain
causes hypea to blossom
normal flora
Overgrowth
DM
Hyperglycermia
Sugar
Corticosteroid use
Chemotherapy
Anti-biotics
Strain of C. albicans present
Congenital Conditions
Palantine torus
DD
sq. cell carcinoma
does not have to be treated
unless
dentures
outgrowth of bone in the hard palate
Cleft palate/Cleft Lip
Surgery
6 wks - 9 mo
Uvula
often split
Folic acid deficiency
Virus
IBD drugs
Genes
Pyogenic Granuloma
benign
may ossify
surgery
may regress spontaneously
may exhibit rapid growth
may become ulcerated
highly vascular peduncular lesion
pregnant women
children
teens
gingiva
red to purple in color
Hairy Leukoplakia
BENIGN
Etio
EBV
THINK
HIV
70% of hairy leuko. found in HIV+ pts
one of first signs
raised white areas
CANNOT be scraped off
Herpangina
NOT a herpes infection
hand-foot-mouth
may see on palms and soles
7 days
located
plalate, tongue, anterior tonsillar pillars
vesicular eruption
Coxsackie A virus
Herpetic stomatitis
Virus Reactivation
Immunosuppression
URI
Diet
Lysine
dormant stage
Argenine
foods
nuts
chocolate
spinach?
gelatin
reese's PB cups and Jello
activates virus
hormonal changes
menses
preg.
Allergies
excessive UV light
Fever
Stress
injury
nuclei full of viruses!
Recurrent infection
1-2 weeks
@ site of primary inoculation
less painful
Primary Infection
may only have one episode
2-4 weeks
painful
malaise
virus dormant in local ganglia
lesions initially appear as vesicles
Herpes simplex
1 & 2
Aphthous Ulcer Stomatitis
aka
canker sores
Histopathology
rimmed
erythema
hyperemic
shallow
lips and gums
Gross Morphology
Zn deficiency
Crohn's dz
hormone changes
before men
AI
Allergy
Microbiology
# [Microbes](https://www.mindmeister.com/2523182037)
- Cellular Microbes
- Prokaryotes
- Bacteria
# [Bacteria](https://www.mindmeister.com/2523165399)
Atypical
Borrelia spp.
Legionella
Coxiella Burnetii
Bordetella pertussis
Other
Legionella spp.
Mycobacterium tuberculosis
Acid Fast
Gram
Gram negative
Facultative anaerobic
microaerophilic or anaerobic
- Borrelia
ANAEROBIC
Spirochetes
- Leptospira
- Treponema
- T.pallidum
- T.trachomatis
Anaerobic Gram Negative Cocci
- Veillonella
Anaerobic Gram Negative Bacilli
Opligate intracellular
Chlamydia spp.
- Chlamydia
- C.pneumoniae
- C.trachomatis
Chlamydia trachomatis serotypes
Lt, L2, L3
Dx: Lymphogranuloma venereum(LGV)
Rx: I. Doxycycline, II. Erytheromycin
D thru K
Dx: Inclusion conjunctivitis in newborns, Infant pneumonia, Cervicitis, Nongonococcal urethritis in men
Rx: -Neonatal ophthalmia: prophylaxis with Silver nitrate, treatment with P.O. Erythromycin, - Infant pneumonia: P.O. Erytheromycin, or P.O. Azithromycin, - Cervicitis:
A, B, & C
Dx: Trachoma (a leading cause of
blindness in the world)
Non spore forming
- Fusobacterium
- Prevotella
- Porphyromonas
- Bacteroides
Bacteroides Melaninogenicus
Dx: Aspiration pneumonia, periodontal abscess
Rx: clyndamycine
bacteriodes fragilis
Dx: trauma related abdominal, pelvic abscesses
Rx: metronidazole
obligate intracellular
Coccoid
Chlamydophila
Pneumoniae
Dx: Community acquired atypical pneumonia
Rx:
Pisttaci
Dx: Atypical Pneumonia from bird dropping
Rx: I. Doxycycline, II. Erythromycine
coccobacillus
Non motile
Non spore forming
Intracellular
Rickettsia spp.
- Coxiella
- Ehrlichia
- Orientia
- Rickettsia
- R.typhi
- R.prowazekii
- R. Rickettsii
Aerobic Gram Negative Cocci
- Moraxella catarrhalis
- Neisserie
NEISSERIA
gonorrhoeae
Dx: UTI, Cervisitis, Gonococcal Disease, PID, bacteremia, septic arthritis, ophthalmia neonatorum
Rx: - adult : oral Ceftriaxon & doxycycline -neonate: oral ceftriaxon & erythromycine & erythromycine eye drops
meningitidis
Dx: meningitis
Rx: prophylaxis with vaccine, stop spread with rifampin, treat with ceftriaxon
- -capsule
- N.gonorrhoeas
- +capsule, utilize maltose
- N.meningitidis
ENTERICS
Klebsiella pneumoniae
Dx: Pneumonia, & Nasocomial sepsis & UTI
Rx: I. Ceftriaxon, II. Aztreonam, or ciprofloxacin
ZOONOTIC
Yersinia
Yersinia pestis
Entercolitica
Dx: Pseudoappendicitis, mesenteric adenitis, rectal bleeding, ileal perforation, ERYTHEMA NODOSUM, REITER'S Reactive Arthritis
Rx: I. no Rx, II.Gentamicin or ciprofloxacin
Pestis
Dx: infection of Bubonic ( lymph nodes ), lung, septicemic
Rx: I. Streptomycin, or gentamicin II. Doxycycline, or ciprofloxacin
Pasteurella multocida
Dx: caused most commonly by cat bite, or scratch, less commonly from dogs; Cellulitis, wound infection
Rx: I. P.O. Amoxicillin/calvunate given with food, II. Doxycycline, or Ciprofloxacin,
Brucella
Dx: Brucellosis, Acute, relapsing, or chronic febrile disease
Rx: I. P.O. Doxacycline & I.M. Gentamicin, II. Ciprofloxacin & Rifampin, III. TMP/SMX & Gentamicin
Francisella tularensis
Dx: Ulcero-glandular(skin and lymph node), Oculo-glandular, GIT, pneumonia, & bacteremia
Rx: I. Gentamicin, II. Doxycycline
HAEMOPHILUS
Ducreyi
influenzae
DIPLOCOCCI
Moraxella catarrhalis
PSEUDOMONAS AERUGINOSA
Dx: Pneumonia in cyctic fibrosis & immunocompromised, Osteomyelitis, burn wound infection, UTI, sepsis, malignant otitis externa, corneal infection with contact lens, endocarditis in I.V. drug abuser
Rx: I. ciprofloxacin, II. piperacillin, or Cefepime, or ceftazidime, or ticracillin, or piperacillin, or Meropenem, or Aztreonam III. IV Polymyxin -Otitis:ear drops polymyxim
VIBRIONACEAE
Helicobacter pylori
Non-invasive methods:
Serological diagnosis: for detection of anti H. pylori antibodies in the patient’s serum
PCR: for detection of the bacterial genes in the gastric juice, gastric biopsy or faeces.
ELISA: for detection of H. pylori antigen in the stool.
Urea breath test: A capsule of 14C or 13C labeled urea is ingested by the patient. If the organism is present, the urease activity generates radiolabeled CO2 that could be detected in the patient’s breath.
Invasive method:
Culture is done on Skirrow’s medium at 37˚C in microaerophilic humid environment and incubated for up to one week. Growing colonies are identified morphologically and biochemically.
Smears are stained with Gram stain or special histologic stains to detect the characteristic morphology.
Rapid urease test in which gastric biopsy is placed in a medium containing urea with pH indicator. If H. pylori is present, the urease enzyme splits urea and results in color change.
Specimen: gastric mucosa biopsy obtained by endoscopy.
Pathogenesis and Virulence factors:
A contact secretion system enables the bacteria to inject its proteins in the epithelial cells of the stomach.
They are produced by some strains and coded by a gene within a pathogenicity island
These proteins are Vacuolating cytotoxin (VacA) that causes vacuolation and apoptosis of cells and Cytotoxin associated protein (CagA).
The production of ammonia along with other proteins results in an inflammatory process that causes damage to the gastric mucosa leading to acute gastritis, gastric & duodenal ulcers, and gastric carcinoma
Then, it attaches deeply to the gastric mucosa by adhesins away from the gastric acidity.
The buffering action of ammonia produced by the enzyme urease helps to neutralize the gastric acidity protecting the organism
H. pylori penetrate the mucous layer of the stomach helped by its flagella.
The only significant reservoir of infection appears to be humans.
Iatrogenic role is also documented.
H. pylori infection is most likely acquired by oral to oral and by feco oral routes.
Cultures are incubated for up to one week.
Skirrow’s medium is used for culture.
It grows best at 37˚C.
Helicobacter needs microaerophilic and humid environment to grow.
They have darting motility using multiple polar sheathed flagellae.
Helicobacter pylori are small Gram negative, comma, S shaped rods.
Infection phlays a key role in the pathogenesis of a number of gastroduodenal diseases including
gastric adenocarcinoma
mucosa-associated lymphoid tissue lymphoma
chronic gastritis
peptic ulcer disease,
It may affect both children and adults.
Helicobcater pylori colonizes the stomach of more than half of the world's population
Obligate intracellular bacteria
Gram positive
Anaerobic
Anaerobic Gram Positive Rod
- Eubacterium
- Mobiluncus
- Bifidobacterium
- Propionibacteriums
- Actinomyces
- Lactobacillus
- Clostridium
Gardnerella vaginalis
- C.botulinum
Food pisoning
- C.perfringen
- C.tetani
Anaerobic Gram Positive Cocci
- Peptococcus
- Peptostreptococcus
Aerobic
Aerobic Gram Positive Cocci
- -catalase
- Streptococcus
- gamma hemolysis
- Enterococcus
GROUP D include Enterococci & Non-enterococci
- beta hemolysis
- -bacitracin
- S.agalactiae
GROUP B aka Streptococcus agalactiae
- +bacitracin
- S.pyogenase
GROUP A aka Streptococcus pyogenes
- alpha hemolysis
- -capsule, -queilung
- S.viridans
- +capsule, +queilung
- S.pneumoniae
STRIPtococcus group
Streptococcus pneumoniae
Viridans
- +catalase
- Staphylococcus
- - coagulase
- -novobiocin
- S.saprophyticus
- +novobiocin
- S.epidermidis
- +coagulase
- S.aureus
Aerobic Gram Positive Rod
Acid Fast
Nocardia spp.
- Erysipelothrix
- Listeria
- Bacillus
- B.anthracis
- B.cereus
- Corynebacterium diptheriae
- Rhodococcus
- Mycobacterium
- M.avium-interacellulare
- M.leprae
Poorly stained
- M.tuberculosis
- No nucleus
- Eukaryotes
- Protozoa
- Algae
- Fungi
Mycology
Moulds
Dermatophytes
epidermophyton, trichophyton, microsporum
athlete's foot, ringworm
disease of skin, hair, nails
Dimorphics
sporothrix schenckii (different)
entry through skin, spreads through lymph
paracoccidioides
P. brasiliensis
RES, skin, mucous membranes
wide spectrum of disease
blastomyces dermatitidis
pulmonary infection
coccidioides immitus
can be chronic or fatal
mostly self-limited RI
histoplasma
infects healthy, but more fatal in immunocompromised
resides in RES
bird droppings
characteristics
spores inhaled in lung, then infects skin & bones, LN, CNS
yeast @ 35 deg, mould @25
Zygomycetes
fatal in immunocompromised
common contaminent
non-septate hyphae
Aspergillus
aspergillosis
invasive
pulmonary aspergilloma
allergic bronchopulmonary aspergillosis
secondary opportunistic
cause disease in presence of underlying condition
septated hyphae
hyphae: filamentous structures
Yeast
Cryptococcus
C. gattii
decaying wood, eucalyptus
CGB agar turns blue
C. neoformans (opportunistic)
soil
environmental sources
Candida
systemic/invasive
mucocutaneous
diaper rash, skin & nails, oral, vulvar
Therapy
antifungals
flucytosin & grisofulvin
inhibit NA synthesis
polyenes (amphotericin)
damage cell membrane
azoles (ketoconazole, etc)
inhibit cell membrane
most are subclinical or self-limiting
NOT Abx
Host Defenses
cell-mediated immunity
toxins
aflatoxins
alkaloids
hepatotoxins (mushrooms)
allergies
tissue damage due to inflam, immune response, granulomas
traumatic implant
inhalation
Lab Diagnosis
serology
molecular techniques
culture
Ag detection
Direct microscopy
KOH, stains, etc
deep mycoses
opportunistic
by less virulent fungi
systemic
by dimorphic fungi
internal organs
subcutaneous
deeper layers of dermis, subcut, & bone
cutaneous mycoses
epidermis, hair, nails (dermatophytes)
superficial mycoses
outer skin, hair (dermatophytes)
dimorphic
single cell
yeast
moulds
mycelium
mat of hyphae
nonseptate hyphae
single continuous cell
septate hyphae
contain septa (transverse walls)
reproduction
sexual
forms spores after mating
asexual
budding, hyphae separation
haploid nucleus
metabolism
obligate aerobes, require carbon
cell structure
cell wall w/chitin
cell membrane w/sterols
nucleus, organelles
- Helminths
- Nucleus
- Noncellular Microbes
- bacteriophage
- lysogenic cycle
- host cell remains alive
- lytic cycle
- host cells lyse and die
- Viruses
# [VIRUS](https://www.mindmeister.com/2523241481)
- Viral Structure
- envelope
- carbohydrate envelope
- lipid envelope
- protein envelope
- spikes : structures that protrude
out of the envelope
- covered the capsid
- capsid
- composed of subunits, capsomers
- protein coat surrounding the nucleic acid
- nucleic acid
- RNA
- single linear, segmented linear,
segmented double stranded
linear
- DNA
- circular – single stranded, double stranded
- linear – single stranded , double stranded
- contain either DNA/RNA but never both
- Size
- wide range
- Host Range
- some are very specific
- determined by presence of
specific receptors on the cell
- narrow host range
- infect invertebrates, vertebrates,
plants, protest, fungi or bacteria
- Characteristics
- viroid : piece of RNA without a protein coat
- virion : intact, fully assembled, infective virus
- contain single type of nucleic
acid, either DNA/RNA but never
both
- obligately intracellular parasites
- smaller than bacteria
- not visible in the light microscope
- not retained by bacterial filters
- Viruslike Agents
- prions
- sensitive to protein denaturing agents
- not sensitive to radiation treatment
- resistant to inactivation by
heating to 90 degree celcious
- viroids
- differ from viruses in six ways
- viroid particles are not apparent in infected
tissue without the use of special
techniques
- copied in the host cell nucleus
- does not produce proteins
- do not require a helper virus
- exist inside cells as particles
- consists of a single circular RNA
molecule of molecular weight
- plant infected
- an infectious RNA particle
smaller than a virus
- Taxonomy
- characteristics to divide viruses
into taxonomic groups
- presence/absence DNA intermediate
- type of virus release
- with/without envelope
- with/without tails
- number of capsomers in icosahedral viruses
- diameter of the virion or nucleocapsid
- presence of envelope
- capsid symmetry
- nucleic acid characteristics
- nature of host
- names of viruses
- genus and sp. : virus
- subfamily : ends with virinae
- family : ends with viridae
- International Commitee for
Taxonomy of Virus (ICTV)
- type of host
- presence/absence of envelope
- the sense (+ve/-ve) of single stranded RNA
- nucleic acid strandedness
- nucleic acid type
- used to be classified based on
host preferences
- bacterial viruses
- plant viruses
- animal viruses
- General Morphology (capsid architecture)
- complex viruses
- enveloped viruses
- polyhedral viruses
- helical viruses
- Family
- RNA Virus
- example : Picornaviruses,
Togaviruses, Rhabdoviruses and
Retroviruses
- after maturation, viruses are released by
budding or through ruptures in the host cell
membrane
- dependent RNA polymerases
synthesizes the double stranded
RNA
- multiplication occurs in the cytoplasm
- DNA Virus
- example : Adenoviruses,
Herpesviruses, Papovaviruses and
Hepadnaviruses
- capsid protein which is synthesis
in the cytoplasm
- transcription and translation
produce viral DNA
- DNA is released into the
nucleus of the host cell
- Isolation and Cultivation
- viral infections
- patterns of viral infection or disease
- persistent
- latent
- infection by individual human viral pathogens
- growth of animal viruses
- in cell cultures
- in embryonated eggs
- in living animal hosts
- quantifying viruses
- plaque assay : the number of plaque directly
relates to numbers of infectious virus particles
applied to the plate
- growth of bacteriophages
- plaque method : mix
bacteriophages with host bacteria
and nutrient agar
Parasitology
# [parasite](https://www.mindmeister.com/2523153442)
Diagnosis of Parasites of the Digestive System Fecal Specimens
Fungi, plant cells, pollen grains and plant fibers.
Charcot-Leyden crystals: due to disintegration of eosinophils.
Macrophage: present in bacterial and parasitic infections.
Eosinophils: indicate an immune response related to parasitosis.
White blood cells (PMNL): may indicate inflammation.
Red blood cells (RBCs): may indicate ulceration.
Helminth egg and larvae.
Trophozoites and cysts of intestinal protozoa.
- platyhelminthes
- cestode
- Extra-intestinal or Tissue cestodes
- Coenuruscyst of Multicepsmulticeps.
- Cysticercoid of Hymenolepisnana.
- Cysticercuscellulosaof Taenia solium.
- Hydatid cyst of Echinococcusgranulosus.
- Sparganum-plerocercoidesof Spirometra.
- nematode
- non-intestinal nematode
- Dracunculus medinensis
- Onchocerca volvulus
- Loa loa
- Brugia malayi
- Wuchereria bancrofti
- arthropods
# [Bugs (Arthropods)](https://www.mindmeister.com/2523160886)
- Myriapoda
- Millipedes
- Centipedes
- Arachnids
- Other
- Mites
- Crabs
- Scorpions
- Ticks
- Lone Star Tick
- Dog Tick
- Deer tick
- Spiders
- Not Poisonous
- Funnel Weaving Spider
- Jumping Spider
- Garden Spider
- Poisonous
- Hobo Spiders
- Banana Spider
- Black Widow
- New node
- Brown Recluse
- Crustaceans
- Lobsters
- Crayfish
- Shrimps
- Insects
- Water Insects
- Many insect larvae
- Caddisfly
- Mosquito
- Water Beetle
- Springtail
- Crawling
- Caterpillars
- Praying Mantis
- Flying
- Beetles
- Moths
- Butterflies
- Hornets
- Flies
- Bees
- protozoa
- non-intestinal
- free living amoeba
- trypanosoma
- leishmania
- malaria
- intestinal
- coccidia
- Sarcocystis spp.
- Isospora (Cystoisospora) belli
- Cyclospora cayetanensis
- Cryptosporidium spp.
- flagellates
- non-pathoden
- enteromonas hominis
- retortamonas intestinalis
- diantamoeba fragilis
- trichomonas hominis
- chilomastix mesnili
- giardia lamblia
- amoebas
- non-pathogen
- i.butschulii
- e.nana
- e.coli
- e.hartmanni
- pathogen
- entamoeba histolytica
Physiology
Cardiovascular System
Cardiology
Heart
Activities
hypertension
stroke
cardiac output
congestive heart failure
Heart beat
above 100
tachycardia
below 60
bradycardia
irregular
Blood circulation
Systemic circulation
Pulmonary circulation
systole
systolic pressure
diastole
diastolic pressure
Conductive system
Perkinje fibers
right and left bundle branches
bundle of His
atrioventricular node(AV node)
pacemaker
sinoatrial node(SA node)
Inside
Four Vessels
Pulmonary vein
Superior or inferior vena cava
Pulmonary Artery
Aorta
Four valves
Atrioventricular Valves
Semilunar Valves
Insufficiency
Regurgitation
bicuspid valve
tricuspid valve
pulmonic valve
aortic valve
Four chambers
Lower
separated by interventricular septum
Right ventricle
Left ventricle
Upper
separated by interatrial septum
Right atrium
Left atrium
Outside
Wall
endocardium
子主题 1
myocardium
Disease: Pancarditis
epicardium
pericardial sac
inner visceral layer
pericardial cavity
pericardial fluid
Disease: pericarditis
outer parietal layer
carry away the waste materials
distribution of nutrients,water,oxygen,and hormones
Location
weight less than 0.5kg
size of fist
in the thoracic cavity, between two lungs
cone-shaped
Blood Vessels
hematopoiesis
Pancytopenia
Aplasia
Composition
other dissolved materials
protein
immunoglobulins
fibrin
water
carry away the waste materials and carbon dioxide from produced by the cells
carry oxygen,nutrients,hormones and water that needed by the cells
Renal Physiology
Biochemical tests of renal function
Renal Plasma Flow: Use measurement of substance PAH as it is secreted by the tubules & only 20-30% filtered by glomerulus. 10% of plasma flow though goes to non-functioning parts of kidney.
GFR Measurement: via creatinine, as they are freely filtered & not absorbed. Can compare blood creatinine vs urine creatinine. If ratio is high then decreased GFR & renal function. Good for comparing before & after of one patient, but not good for between pt's.
Urinanalysis: for glucose, creatinine, drugs,
Bicarbonate Handling
NET ACID EXCRETION = NH4+ EXCRETION + URINARY TITRATABLE ACID (PHOSPHATE) - HCO3- EXCRETION
PHOSPHATE BUFFER: H+ can bind to phosphate & be excreted in the urine. Only small amounts of phosphate in body though.
AMMONIUM SYNTHESIS: Ammonium can bind to Cl- & H+ & be secreted as a compound in the urine. Only a small amount can be excreted this way. When ammonia is formed from glutamate, 2 ammonium ions & 2 bicarbonate ions are formed which are reabsorbed. The collecting duct however secretes NH3 which can combine to H+ and form NH4+ which is then excreted due to impermeability to this ion. Systemic acidosis & hypokalaemia promotes this function.
SECRETION OF H+: More H+ is secreted than HCO3- is absorbed
PRODUCTION OF 'NEW' HCO3-: via ammonium (below) & phosphate. Everytime a H+ is excreted in this way, has the effect of adding 1 'new' HCO3- to the body. Also glutamine metabolism creates 2 new HCO3- molecules while also producing 2 NH4+ ions.
NET LOSS OF BICARBONATE IONS: When alkalosis occurs, for every 1H+ less in the body, 1 HCO3- is also lost as they are usually required as a pair. In effect this is like adding 1 H+ to the blood, so pH goes up.
Drugs: Diuretics
K+ SPARING
Spironolactone inhibits the Na+/K+/ATP pump in the late distal tubule that is usually up-regulated by Aldosterone. It is an aldosterone antagonist. Prevents hypokalemia in vulnerable pt's.
LOOP
Frusemide acts on the Na+/2Cl-/K+ co-transporter in the thick ascending limb
THIAZIDES
Hydrochlorothiazide acts on the Na+/Cl+ co-transporter in the late distal tubule
Disease
COLLECTING TUBULE
Solutes absorbed: Na+ (5%), usually impermeable to H20, however, H20 (5% in water loading, >24% in dehydration). Influenced by ADH.
Na+/K+ antiporter in luminal membrane. ADH causes insertion of aquaporins, increasing H20 reabsorption.
LATE DISTAL TUBULE
Solutes absorbed: NaCl (5%). Fine tuning System. Influenced by Aldosterone. Without =2%, with=5%
Specialisations: Na+/K+/ATPase pump in basolateral membrane that may be up-regulated by Aldosterone. Also a Na+/Cl+ co-transported using energy from other pump to drive.
THICK ASCENDING LIMB
Solues absorbed: impermeable to H20. NaCl, K+, Ca2+, Mg2+, HCO3- (all 25%),
Specialisations: Na+/K+/ATPase pumps in basolateral membrane. A co-transporter that moves 1Na+, 2Cl-, 1K+ into tubular cell. This also drives Ca2+ & Mg2+ into cell. This section is also part of counter-current mechanism.
THIN DESCENDING LIMB
Solutes absorbed: only 10% water. A little urea & Na+ passive diffuses as well.
Specialisations: Part of the counter current mechanism in the vasa recta. H20 is drawn out via oncotic pressure differences and not via active transport
CHRONIC RENAL FAILURE: Stage 1: GFR>90 Stage 4: GFR=15-29 Stage 5: GFR=90%)
Bicarbonate reabsorption: H+ from Na+/H+ pump combines with HCO3- in lumen forming H2CO3. This then dissociates into CO2 + H20. These then diffuse into tubular cell. They thnen reform and H+ is pumped out while HCO3 is co-pumped with Na+ into capillary.
Specialisations: Brush border filled with protein carrier molecules & Na+/K+/ATP pumps. Also a Na+/H+ pump in luminal membrane & a basolateral HCO3-/Na+ co-transporter for bicarbonate handling.
ACUTE RENAL FAILURE: Abrupt decline in GFR & accumulation of nitrogenous waste (creatinine + urea). COMPLICATIONS: Fluid overloas, pulmonary oedema, heart failure, hyperkalaemia.
Post-renal: Bladder outflow obstruction, neurogenic bladder, urethral stricture, ureteric obstruction (stone), carcinoma
Test: Hydronephrosis on abdominal U.S
Intra-renal:
Vascular: Hypertension, Polyarteritis
Glomerular (presence of haemeturia, lipiduria & proteinuria): glomerularnephritis is usual cause & is divided into types:
2) Nephrotic Syndrome: associated with high proteinuria & caused from diseases such as Diabetes, Hep B, HIV, Obesity. Also associated with hyperlipidemia & oedema.
1) Nephritic Syndrome: inflammatory condition associated with low urine volume & haematuria
Tubulo-interstitial: 1) Acute tubular necrosis (usually resolves), from unresolved pre-renal problem 2) Interstitial nephritis: DRUGS like penicillins, aspirin, NSAIDS (Analgesic nephropathy).
Pre-Renal: SHOCK, Hypovolaemia, Renal artery stenosis.
Test: bland urinary sedement (little protein/cells, high serum urea compared to creatinine.
Nephron: Renal Corpuscle (Glomerulus) + Renal tubule
Nephron structure
Atrial Natriuretic Peptide (ANP)
Secreted in the atria, it inhibits Na+/H20 reabsorption by decreasing secretion of Renin & Aldosterone. Also acts by vasodilating the afferent arteriole & increasing GFR & decreasing reabsorption of Na+. Overall effect is Total Blood Volume is reduced.
Other Effects of ANG 2 besides increase in Aldosterone
Osmoreceptors in the Hypothalamus
If osmolarity becomes higher than normal, cells will shrink in the hypothalamus, which stimulutes thirst centres and the production of ADH
ADH has several effects:
2) Acts on V2 receptors in arterial smooth muscle, resulting in vasoconstriction & increased BP
1) Acts on V2 receptors, increasing water reabsorption in kidney through direct insertion of aquaporins in the collecting tubule
Other Specialised cells outside the nephron (includes below):
Zona Glomerulosa Cells of the adrenal glands
Produce Aldosterone in response to 2 stimuli which increases ACTH & thus Aldosterone secretion:
Results in 1) Upregulation & activation of basolateral Na+/K+ pumps in the distal tubule & collecting duct. 2) Stimulating NaCl/H20 reabsorption in GIT, salivary & sweat glands 3)May stimulate Vasopressin/ADH release from posterior pituitary 4) Increases renal efferent tubule resistance, increasing hydrostatic pressure & thus GFR
2) Increased [K+]
1) Increased ANG2
Specialised Cells: Cells of the Juxtaglomeular apparatus
Extraglomerular mesangial cells (5b)
Role is poorly understood but is believed to help with the renin-angiotensin-aldosterone system
Macula Densa Cells (7)
Located in the distal convoluted tubule close to the glomerulus
Sense changes in NaCl concentration as a result of more reabsorption following a slower GFR as a result of decrease in BP. Respond in 2 ways
2) Stimulates release of Renin by JG cells via prostaglandins
1) Decrease resistance to flow in the afferent arteriole thereby increasing hydrostatic pressure & increasing GFR
1) Juxtaglomerular (JG)/Granular cells (6)
Located in the wall of the afferent arteriole
They secrete renin in response to a) increased sympathetic (beta-1) stimulation & b) renal hypoperfusion caused by hypotension or volume retention c) stimulation by the macula densa cells
Tubules
Ureters
Passes down to the bladder
Loop of Henle
Sets up a counter-current mechanism that concentrated the urine
Subtopic 1
Arterioles: come off the renal arteries
Efferent arteriole conducts the unwanted blood away from the glomerulus back to the circulation
Afferent arteriole conducts blood into the glomerulus
Bowman's space
This area is where all blood once passed through glomerular capillary membrane passes into. This space then drains into the proximal convoluted tubule
Glomerulus cell
Summary
3) Podocytes (3b): locate outside the basement membrane, these are arranged alongside each other, leaving filtration 'slits' between them. This allows small solutes to pass through but prevents albumin & larger proteins from exiting the blood stream
2) Mesangial cells (5a): may play a role in changing size of surface area of glomerus capillaries
1) Endothelial cells(1)-leakiest in the body located on top of a basement membrane
Jextamedullay nephrons: make concentrated urine-go deep into medulla
Cortical nephrons: cannot concentrate urine as much, don't go deep into medulla
# [Histology](https://www.mindmeister.com/2524225232)
- Epithelial
Tissue
- Simple
- Pseudostratified columnar
- Protection, secretion, particularly of mucus;
propulsion of mucus by ciliary action.
- Single layer of cells of differing heights,
some not reaching the free surface; nuclei
seen at different levels; may contain
mucus-secreting cells and bear cilia.
- Lining of nasal cavity, trachea, and bronchi;
nonciliated type in male's sperm-carrying
ducts and ducts of large glands; ciliated
variety lines the trachea, most of the upper
respiratory tract.
- Protection, secretion of mucus, enzymes,
and other substances ciliated type propels
mucus (or reproductive cells) by ciliary
action, absorption.
- Single layer, tall cells with round to oval
nuclei; some cells bear cilia; layer may
contain mucus-secreting unicellular glands
(goblet cells).
- Nonciliated type lines most of the digestive
tract (stomach to anal canal), gallbladder,
and excretory ducts of some glands; ciliated
variety lines small bronchi, uterine tubes,
and some regions of the uterus.
- Limited protection, secretion, absorption
- Single layer, cube-like cells with large,
spherical central nuclei.
- Glands; ducts; portions of kidney tubules,
thyroid gland, ovary surface
- Reduces friction; controls vessel
permeability, performs absorption and
secretion.
- Single layer, disc-shaped central nuclei and
sparse cytoplasm, thin, flat
- kidney glomeruli, air sacs of lungs; lining of
heart; blood vessels; lining of ventral body
cavity
- Stratified
- Transitional epithelium
- Stretches readily and permits distension of
urinary organ by contained urine
- Resembles both stratified Squamous and
stratified cuboidal; basal cells cuboidal or
columnar: surface cells dome shaped or
squamous-like, depending on degree of
organ stretch.
- Lines the ureters, urinary bladder, and part
of the urethra; renal pelvis.
- Columnar epithelium
- Protection; secretion
- Multiple layers, basal cells usually cuboidal;
superficial cells elongated and columnar.
- Rare in the body; small amounts in male
urethra and in large ducts of some glands.
- Cuboidal epithelium
- Protection, secretion, absorption
- Multiple layers, generally two layers of
cube-like cells.
- Largest ducts of sweat glands, mammary
glands, and salivary glands.
- Squamous Epithelium
- Provide physical protection against
abrasion, pathogens, and chemical attacks.
- Multiple layers, basal cells are cuboidal or
columnar and metabolically active; surface
cells are flattened (squamous); in the
keratinized type, the surface cells are full of
keratin and dead; basal cells are active in
mitosis and produce the cells of the more
superficial layers
- Nonkeratinized type forms the moist linings
of the esophagus, mouth, and vagina;
keratinized variety forms the epidermis of
the skin, a dry membrane.
- Muscle Tissue
- Smooth muscle
- Propels substances or objects (foodstuffs,
urine, a baby) along internal passageways;
involuntary control.
- Spindle-shaped cells with central nuclei; no
striations; cells arranged closely to form
sheets.
- Mostly in the walls of hollow organs.
- Cardiac muscle
- As it contracts, it propels blood into the
circulation; involuntary control.
- Branching, striated, generally
uninucleate cells that interdigitate at
specialized junctions (intercalated
discs)
- The walls of the heart.
- Skeletal muscle
- Voluntary movement; locomotion;
manipulation of the environment; facial
expression; voluntary control
- Long, cylindrical, multinucleate cells;
obvious striations
- In skeletal muscles attached to bones or
occasionally to skin.
- TRAN PHAM
- Connective Tissue
- Blood
- Transport nutrients gases, waste, chemicals, heat,
immunity, clotting, growth factor.
- Pale pink discs (erythrocytes), no nuclei,
platelets, leukocytes are larger.
- Heart and blood vessels
- Bone/ Osseous tissue
- Bone supports and protects (by enclosing); provides levers for the muscles to act
on; stores calcium and other minerals and fat; marrow inside bones is the site for
blood cell formation (hematopoiesis)
- Hard, calcified matrix containing many collagen
fibers; osteocytes lie in lacunae. Very well
vascularized.
- Bone
- Cartilage
- Hyaline
- Supports and reinforces; has resilient
cushioning properties; resists compressive
stress.
- Amorphous but firm matrix; collagen fibers form an
imperceptible network; chondroblasts produce the matrix and
when mature (chondrocytes) lie in lacunae.
- Forms most of the embryonic skeleton; covers the ends of long bones
in joint cavities; forms costal cartilages of the ribs; cartilages of the
nose, trachea, and larynx
- Elastic cartilage
- Maintains the shape of a
structure while allowing
great flexibility.
- Similar to hyaline cartilage,
but more elastic fibers in
matrix
- Supports the external ear
(pinna); epiglottis.
- Fibrocartilage
- Tensile strength with the ability to
absorb compressive shock.
- strucure
- Matrix similar to but less firm than that in
hyaline cartilage; thick collagen fibers
predominate.
- Intervertebral discs; pubic
symphysis; discs of knee
joint.
- Dense connective tissue
- Elastic tissue
- Allows recoil of tissue following
stretching; maintains pulsatile flow
of blood through arteries; aids
passive recoil of lungs following
inspiration.
- Dense regular connective
tissue containing a high
proportion of elastic fibers.
- Walls of large arteries; within
certain ligaments associated
with the vertebral column; within
the walls of the bronchial tubes.
- Dense irregular
- Able to withstand tension exerted in many
directions; provides structural strength;
helps prevent overexpansion of organs
such as the urinary bladder
- Primarily irregularly arranged
collagen fibers; some elastic
fibers; major cell type is the
fibroblast.
- Fibrous capsules of organs
and of joints; dermis of the
skin; submucosa of
digestive tract.
- Dense regular
- Provides firm attachment;
conducts pull of muscles; reduces
friction between muscles;
stabilizes relative positions of
bones
- Primarily parallel collagen
fibers a few elastic fibers; major
cell type is the fibroblast.
- Between skeletal muscles and skeletal (tendons
and aponeuroses); between bones or stabilizing
positions of internal organs(ligaments); covering
skeletal muscles; deep fasciae.
- Loose connective tissue
- Reticular
- Fibers form a soft internal skeleton
(stroma) that supports other cell types,
including white blood cells, mast cells,
and macrophages.
- Network of reticular fibers in a typical
loose ground substance; reticular cells lie
on the network
- Liver, Kidney, spleen, lymph
nodes, and bone marrow
- Adipose
- Provides padding and cushions
shocks; insulates (reduces heat
loss); stores energy reserves
- Matrix as in areolar, but very sparse:
closely packed adipocytes, or fat cells,
have nucleus pushed to the side by
large fat droplet
- Deep to the skin, especially at
sides, buttocks, breasts; padding
around eyeballs and kidneys.
- Areolar
- Wraps and cushions organs; its
macrophages phagocytize bacteria;
plays important role in
inflammation; holds and conveys
tissue fluid.
- Gel-like matrix with all three
fiber types; cells: fibroblasts,
macrophages, mast cells, and
some white blood cells.
- Widely distributed under epithelia of
body, e.g., forms lamina propria of
mucous membranes; packages organs;
surrounds capillaries.
- Nervous Tissue
- function
- Transmit electrical signals from sensory receptors and
to effectors (muscles and glands) which control their
activity.
- structure
- Neurons are branching cells; cell processes that may be quite
long extend from the nucleus-containing cell body; also
contributing to nervous tissue are nonirritable supporting cells
(not illustrated)
- location
- Brain, spinal cord, and nerves
موديولات
cns
Practical physiology
Sensation, Pain Control & Ascending Tracts
Sensations
They are divided into 3 types according to their site of origin:
Somatic sensations:
e.g., sense of position, movements, muscle tension, deep pressure, relation of the body parts to each other, relation of the body to the space, deep pain & sensations which adjust body equilibrium and detected by the non-auditory labyrinth in the inner ear.
Definition: they are sensations which come from muscle, ligaments, joints and capsules.
They are subdivided into:
Proprioceptive (kinesthetic, deep) sensations:
Cutaneous (superficial) sensationse.g., pain, touch, temperature & pressure.
They originate from soma (body).
CAVERNOUS SINUS
Superior
Internal carotid artery.
Optic tract
Optic chiasma
Lateral
Temporal lobe (uncus) of the cerebral hemisphere.
Medial
Sphenoid air sinus.
Pituitary gland (hypophysis cerebri)
Position: situated on either side of the body of the sphenoid and sella turcica in the middle cranial fossa.
The cavernous sinus (2 cm long, 1 cm wide) is a large venous space, its interior is divided into a number of small spaces (caverns) by trabeculae, hence the name cavernous sinus.
ماسكلو
Skin 1
Parasites affecting Skin
Skin infections
DIAGNOSIS OF SKIN INFECTIONS
REMEMBER
Tetanus is a totally preventable disease using tetanus toxoid and tetanus antitoxin as active and passive immunoprophylaxis, respectively.
Alpha toxin is the most important virulence factor for C. perfringens, while tetanospasmin is the virulence factor of C. tetani.
C. perfringens causes gas gangrene following massive trauma, while C. tetani causes tetanus following trivial (minor) trauma.
C. perfringens and C. tetani are anaerobic Gram-positive spore forming bacilli.
Protein M, fibrinolysin, hyaluronidase and secreted toxins are important S. pyogenes virulence factors.
S. pyogenes: Gram positive cocci in chains and catalase negative.
Protein A, coagulase and secreted toxins are important S. aureus virulence factors.
S. aureus: Gram positive cocci in clusters and catalase positive.
S. pyogenes infections are pyogenic and invasive.
S. aureus infections are pyogenic and localized.
Soft tissue infections can be uncomplicated (superficial) or complicated (deep).
Osteomyelitis and septic arthritis are very important musculoskeletal infections.
For viral infections, stained smears of vesicle fluid are examined under the microscope for typical cytopathology. Vesicular fluid could be examined for viral Ags (with immunological techniques e.g. ELISA) or for viral nucleic acids (with molecular techniques e.g. PCR).
Microscopic examination of a KOH preparation of skin scales, nail scrapings, or loose hair is useful for fungal infections.
Ultraviolet light (Wood's lamp) is helpful in diagnosing some fungal infections.
Staining and/or culturing of a specimen of pus or exudate are often adequate for diagnosis of bacterial infections.
FUNGAL INFECTIONS OF SKIN, HAIR AND NAILS
Fungal Infections of Nails
Thickening (Fig. 27) with loss of the nail can occur.
Onychomycoses are infections of the nails by fungi. This is caused mainly by
and occasionallyو أحيانا by Candida spp.
dermatophytes (Trichophyton and Epidermophyton) i.e. tinea ungium
Dermatophytes (Ringworm Infection)
Clinical disease:
Tinea lesions acquire a second name according to the anatomical site i.e. T. capitis (scalp), T. pedis (foot), T. corporis (trunk), T. cruris (groin), T. barbae (beard), T. manum (palms) and T. ungium (nails).
Dermatophyte lesions are circular (ringworm) with active (extending) edge and healing centers (Fig 26).
Source of infection:
Geophilic: from the soil.
Zoophilic: animal (cat, cattle) to man, the lesion is usually inflamed and oozing.
Anthropophilic: man, to man, the lesion is usually benign.
Taxonomically, they belong to 3 genera which are:
All produce the same clinical affections; tinea or ringworm lesion (Fig 26) which has an inflamed circular border surrounding a clear area of relatively normal skin.
Epidermophyton
Trichophyton
Microsporum
Dermatophytes are filamentous fungi (molds) that cause superficial infection of keratinized structures (skin, hair, and nail) (Cutaneous mycosis).
Tinea Versicolor
A superficial mycosis caused by the lipophilic yeast Malassezia furfur , characterized by presence of hypopigmented or hyperpigmented circular lesions, covered with branny scales on the upper trunk, neck and shoulders
VIRAL SKIN INFECTIONS
Measles Virus
A live attenuated vaccine is given by injection at 12 to 15 months of age. Another dose is recommended before school entry. It may be given in combination with mumps and rubella (MMR) vaccines
Laboratory diagnosis is rarely used
Easy to diagnose clinically.
Clinical
Encephalitis (rare
Bronchopneumonia and otitis media (with or without secondary bacterial infection)
Infection produces a lifelong immunity.
As the fever subsides the maculopapular rash appears all over the body (Fig 24). The rash is caused primarily by cytotoxic T cells attacking the virus-infected endothelial cells in the skin.
Prodroma is characterized by fever, conjunctivitis, cough, and Koplik' s spots (bluish white ulcerations on the buccal mucosa opposite the lower molars).
The disease lasts for 7 to 11 days; prodromal phase of 4 days followed by an eruptive phase of 5 to 8 days.
Incubation period: 8-12 days.
Infection occurs by droplets. Primary multiplication occurs in the respiratory mucosa from where it passes to the regional lymph nodes and the reticulo endothelial system to pour in the blood causing viremia then it localizes in the skin and mucous membrane.
Causes measles, a highly contagious disease of children.
Humans are the only natural host
Single antigenic type.
An enveloped RNA virus with helical symmetry.
Papilloma Viruses
They cause warts at cutaneous or mucosal sites. Cutaneous warts e.g. plantar warts (Fig 23) are generally painless, firm, dry, and rough. They may remain stable or regressتقل spontaneouslyتلقائيا.
Human papillomaviruses (HPV) are small non-enveloped DNA viruses with icosahedral capsid.
Molluscum Contagiosum Virus (MCV)
Transmitted by close contact and sexually. It is common in children and immunocompromised persons. The disease is generally harmless and selflimiting.
An enveloped ds DNA poxvirus, and is characterized by development of numerous small, umbilicated pink nodules (Fig 22), on the face, genitalia, or the rectal area.
Herpes Simplex Virus Type I (HSV-1)
Others e.g. keratoconjunctivitis, encephalitis.
Herpes labials
crops of vesicles at the mucocutaneous junction of the lips or nose.
Acute gingivostomatits
occurs as vesicular lesions in the mouth in children with fever and irritability.
Reactivation of latent virus leads to recurrent disease. The virus travels back down sensory nerves to surface of body and replicates, causing tissue damage and vesicular lesions. Stimuli for reactivation include fever, emotional or physical stress and exposure to strong sun light.
The virus then migrates along axons to sensory nerve ganglia where it becomes latent and escapes the immune response. In general, HSV-1 becomes latent in the trigeminal ganglia.
HSV-1 is transmitted by contact. Primary infections usually begin in early childhood through a break in the mucus membranes or via minor abrasions in the skin. Initial infections are usually asymptomatic and involve the mouth or the face.
Lesions caused by HSV-1 are, in general, above the waist (non-genital).
It is an enveloped DNA virus with icosahedral symmetry, 120-200 nm. The envelope is derived from the nuclear membrane of the infected cell.
Viruses either infect the skin
or as a part of their systemic disease (Secondary viral infections) forming skin rash e.g. measles, rubella (German measles), Epstein Barr virus (infectious mononucleosis), varicella zoster virus (chickenpox), coxsakie (hand foot mouth disease) and herpesvirus type 6 &7 (roseola).
primarily (Primary viral infections) e.g. herpes simplex virus type 1 (HSV-1)
Bacterial Infections of the Skin
Skin infections often follow a break in normal skin integrity by trauma. Skin infections associated with pus formation are known as pyoderma. Common presentations of skin infections and their bacterial causes are presented in (Table 1 & Fig 10).
Other bacterial infections involving the skin include:
Malignant pustule caused by Bacillus anthracis
Clinically, a papule first develops which rapidly changes into a vesicle, then a pustule, and finally a necrotic ulcer with black eschar سوداءندبة(Fig 20). The infection may disseminateينتشر, giving rise to septicemia. For treatment, ciprofloxacin is the drug of choice. Doxycycline is an alternative drug.
The infection is by the entry of spores through injured skin i.e. following trauma.
Anthrax is primarily a disease of sheep, cattle, and horses. Humans are rarely affected (zoonosis).
Cutaneous anthrax refers to infection of the skin by Bacillus anthracis which is a large aerobic, spore forming, gram-positive bacilli, arranged in long chains (Fig 19). Spores are in the center of the non-motile bacilli.
Leprosy caused by Mycobacterium leprae
Leprosy also known as Hansenʼs disease is a long term chronic infection caused by the bacterium Mycobacterium leprae (Lepra bacilli)
Mycobacterium leprae
Diagnosis is confirmed by using polymerase chain reaction test (PCR) on a skin sample.
For laboratory diagnosis, scrapings or biopsies from nose, ear and skin lesions are taken. Histopathological examination reveals the characteristic lesion. Staining with modified Ziehl-Neelsen (Z.N.) technique (5% H2SO4), shows intracellular bunches of acid-fast bacilli (Fig 18).
Lepra bacilli with modified Z.N. stain. Red (acid fast) bacilli in bundles can be seen inside macrophages
Primarily based on clinical findings.
Clinical forms:
Tuberculoid leprosy :
CMI(cell mediated immunity) is maintained.
Lesion contains low number of bacilli and is therefore less infective than lepromatous form.
Hypopigmented macular skin lesions with thickened superficial nerves and significant anesthesia.
Lepromatous leprosy:
It can be lethal
Cell mediated immunity (CMI) is reduced.
Lesion contains large number of bacilli and is therefore highly infectious.
Multiple skin nodules giving the typical leonine (lion like) facies.
Bacteriologic characters:
Cannot be grown in vitro
Stained deep red with modified Ziehl-Neelsen technique.
Acid and alcohol fast bacilli
Staphylococcal Scalded Skin Syndrome
Staphylococcal scalded skin syndrome (SSSS), also called Lyell's disease, starts as a localized lesion, followed by widespread erythema and exfoliation (sloughingتقشير) of the epidermis. This disorder is caused by Staph. aureus epidermolytic which elaborates يفرز an epidermolytic toxinسم محلل للجلد. The disease is more common in infants than in adults. Fig 16. Scalded skin syndrome.
Folliculitis and Skin abscesses
Skin abscess (Fig 15): an infection of the dermis and deeper layer of the skin. A localized form called furuncle (boil) is an infection of hair follicle with involvement of subcutaneous tissue. A carbuncleمجموعة من الدامل التجاورة is a confluenceتجمع of multiple furunclesدمامل forming a large indurated painful lesion with multiple draining sites. Staph. aureus is the most common cause of skin abscesses.
Folliculitis (Fig 14): an infection of the hair follicles caused by Staph. aureus.
Erysipelas and Cellulitis
Cellulitis (Fig 13): an infection involving the inner layers of the skin (dermis and subcutaneous fat). Characterized by redness with ill-defined borders, commonly caused by group A streptococci or Staph. aureus.
Erysipelas (Fig 12): an infection that involves the more superficial layers of the skin involving blockage of the dermal lymphatics, characterized by redness with welldefined edges and edema. It is caused mainly by group A streptococci.(strept. Pyogenes)
Impetigo
Normal Flora of the skin
It is the micro-organisms that live normally and permanently on skin and cause no harm, such as Staphylococcus epidermidis, Corynebacterium spp. and Candida albicans. They contribute to the maintenance of healthy skin.
Skin Histological and gross structure
SKIN APPENDAGES
Keratinous appendages
Nail
Hair
Structure of hair:
مطع عرضى للجذر الشعرة root و ما حوله من البصيلة follicle
Shaft projecting above the surface of the skin
It is formed of 4 layers (Fig. 10)
Cuticle
It is formed of scale like non-nucleated cells.
It is the outermost layer of the shaft (hard keratin)
Cortex
It is composed of Keratinized fusiform cells rich in pigment (give colour of hair).
It surrounds the medulla.
Medulla
It contains poorly keratinized vacuolated cells (soft keratin) separated by air space.
It is the central core of the shaft.
It is the part of hair projecting above the surface of the skin.
Root embedded in the skin.
NB.: Mass of cells inside hair bulb or hair matrix contains stem cells and melanocytes.
It is surrounded by hair follicle (Fig. 11).
Mass of cells inside hair bulb around dermal papilla (Hair matrix).
Its expanded terminal part, indented and its concavity fits shape of dermal papilla (vascular connective tissue) in the dermis.
It is embedded part of hair (not exposed part).
The follicle.
It is formed of two sheathes
External Root Sheath.
NB.: Arrector Pili Muscle is smooth muscle fibers originating from the papillary layer of the dermis. It extends superficially to underlie sebaceous gland to be inserted into papillary layer at an oblique angle to the dermal sheath.
The dermis that surrounds the hair follicle is dense and forms a sheath of connective tissue called connective tissue dermal sheath.
The epithelium of the external root sheath is separated from the dermis by a noncellular membrane called glassy membrane which is their thickened basal lamina.
Below this level, it is formed by cells of the Malpighian layer.
Above the level of the sebaceous gland duct it contains all layers of the epidermis.
It surrounds the internal root sheath and is continuous with the epidermis.
Internal Root Sheath.
of soft keratin, 3 layers:
Henle's layer:
Formed of one layer of elongated cells rich in hyaline granules.
Huxley's layer:
Transparent two or three cell layers.
Cuticle cells:
Flat overlapping scaly cells rich in soft keratin and lying in contact of the hair.
A tubular invagination of the epidermis extending into the dermis and surrounding the hair (Fig. 11)
Its color, size, distribution varies according to race, sex, and body region.
It is a keratinized filamentous structure projecting on the epidermis.
Skin glands:
انواع الغدد بشكل عام
Sebaceous glands.
NB.: Acne is the most common disease involving the sebaceous glands and hair follicles. Obstruction of the duct results in accumulated secretion followed by bacterial infection. It is usually seen in teen agers with increasing sex hormones.
It is lined by stratified squamous epithelium
It opens into the upper part of the hair follicle at the junction of its upper 1/3 with the lower 2/3.
Ducts converge to open in a large short duct.
Cluster of acini opens into a single short duct.
Sebum helps to keep thin skin and its hairs soft and water proof.
Sebum passes through the short duct into the lumen of hair follicle.
This process produces the oily secretory product of the gland, called sebum.
The epithelium of this gland is modified and along its base is a row of columnar or cuboidal cells (basal cells). These cells divide and fill the acinus of the gland with larger, polyhedral cells (secretory cells) that enlarge, accumulate secretory material and undergo degeneration.
It is lined with a stratified epithelium that continues with the external root sheath of hair follicle.
Compound acinar or alveolar gland.
Sebaceous gland connected to the hair follicle.
They are holocrine glands; meaning that the entire cells become part of the secretion.
They are simple alveolar glands.
Sebaceous glands present mainly in the dermis of thin skin.
Sweat glands
There are two main types of sweat glands:
apocrine and eccrine sweat glands of the skin
Apocrine Sweat Glands
They differ from the eccrine sweat glands in
NB.: Cerminous (wax) glands of the external ear and glands of Moll in the eyelids are modified apocrine sweat gland.
Their secretion is a cloudy viscous odorless fluid secreted by merocrine mechanism. Once it is secreted it acquires a "distinctive" odor as a result of bacterial degradation
They function after puberty under hormonal control
Their ducts open into the hair follicles at location superficial to the entry of sebaceous gland duct.
The lumina of the secretory portion are wide and dilated and the secretory cells are low cuboidal
Their secretory portion present deep on dermis
They are present only in axilla, breast, pubic and perineal regions
They are larger than eccrine glands
Eccrine Sweat Glands
They are formed of 2 portions:
Conducting portion.
Its main function;
Duct cells excrete ions, urea, lactic acid and some drugs.
Conduct the secreted sweat
It is lined by denser staining stratified cuboidal epithelium. As a duct reaches the epidermis, its wall is formed by the surrounding epithelium.
surface (sweat pore).
It is continuous with the secretory unit at its base.
Secretory portion.
it is embedded in the dermis and formed of 3 types of cells:
Myoepithelial cells
Its main function; their contraction aid in expressing the gland's secretion into the duct system.
The cytoplasm contains both actin and myosin filaments.
They are present between the secretory cells and their basement membrane.
Clear cells
Its main function; secrete watery secretion.
The basal cell membrane is highly folded to increase surfacearea (for ions and water transport).
The cytoplasm is pale (no secretory granules, abundant glycogen granules, so, appear clear).
Their bases are broad and the apices are narrow.
More numerousعديدة than the dark cells.
Dark cells
Its main function; secrete mucus.
They contain many apical mucinogen granules or secretory vesicles.
They are pyramidal cells with narrow bases and wide apices.
They are merocrine gland.
They are simple coiled tubular glands.
They are present in the dermis of both thick and thin skin.
Types of the Skin (table 1)
Thin Skin
Thick Skin
Layers of skin
Formed of: (Fig. 5)
Deeper reticular layer.
I t is richly supplied by nerves and nerve ending (Pacinian corpuscles and Krause end bulbs).
It contains a rich network of blood (regulate the body temperature) and lymph vessels. Arteriovenous anastomoses are also present in some areas.
Type I collagen fibers and a network of thick elastic fibers.
It is formed of dense irregular connective fibers, running in different directions:
It is the deeper layer of the dermis.
Superficial papillary layer.
NB.: The epidermis is fixed to the dermis through basement membrane, dermal papillae and hemidesmosomes.
The papillary layer is characteristically forms the dermoepidermal junction with the epidermis superficially to provide better fixation and stability for the two parts. This also increases the surface area for better nutrition of the epithelial layer
It contains :
Many blood capillaries and nerve receptors (Meissner's corpuscle and Krause end bulb).
Connective tissue cells especially fibroblasts, macrophages and plasma cells.
Type III collagen fibers, elastic fibers and type VII collagen fibers that form anchoring fibrils.
It forms dermal papillae interdigitating with epidermal ridges.
The superficial layer formed of loose connective tissue.
Its thickness varies in the different regions and it is thickest at the back.
It contains sweat glands, sebaceous glands and hair follicles.
It is mesodermal in origin.
It forms a connective tissue layer under the epidermis.
EPIDERMIS
There are 4 types of cells in the epidermis:
Keratinocytes
Keratinocytes of epidermis are arranged in 5 layers (Figs. 2 &3):
NB.: The Malpighian layer of the skin is generally defined as both the stratum basale and spinosum as a unit.
Stratum corneum (horny layer)
These dead cells are continuously shed off from the surface and replaced through successive mitotic division of the basal layer.
Lipid accumulation in the intercellular spaces contributes to the high water proof properties of this layer
Flat keratin scales (tonofilaments) replace the cytoplasm.
It consists of flattened dead non-nucleated keratinocytes with no organelles and no nuclei.
Acidophilic scaly layer (15-20 layers) of flattened dead non-nucleated keratinocytes.
It is thicker in thick skin.
It is the most superficial layer of the epidermis.
Stratum lucidum (clear layer)
Cells are formed of packed immature keratin.
Their plasma membranes are thickened.
No cell organelles can be seen.
Extremely flattened cells.
It is formed of tightly packed flattened cells without nuclei or organelles but they contain densely packed keratin filament.
It appears as a clear unstained or lightly stained homogenous layer.
It is thick in thick skin.
Stratum granulosum (granular layer)
Contain 2 types of granules:
Membrane coated granules (lamellar granules).
Keratohyalin granules: non membranous.
No mitochondria and no nuclear envelope (degenerated nuclei) can be seen.
Tonofilaments can be seen.
The cells are full of irregularly shaped non membranous granules.
They contain intensely basophilic keratohyalin granules (source of the amorphous protein component of soft keratin).
Consists of 3-5 layers of flat cells with flat nuclei.
Stratum spinosum (prickle cell layer)
The cells of superficial layer contain membrane-coating granules (lamellar granules). The content of these granules are lipids and lipoprotein, released by exocytosis into the intercellular space and cement the cells together to be impermeable to water and foreign substance.
The cytoplasm is full of many tonofilaments, ribosomes and few mitochondria.
The synthesis of keratin continues in this layer, which are assembled into bundles of tonofilaments to provide cohesion among cells and resistance to the epidermal abrasion as they terminate at desmosomes.
The cells are adherent to each other by many desmosomes.
Langerhans cells are present in this layer.
The cells become smaller as they become near the surface.
Their nuclei are central in position.
Less basophilic than the basal layer.
It is thicker in thick skin (palms and soles).
It is formed of 4-6 layers of polyhedral cells.
As the keratinocytes divide by mitosis, they move upward in the epidermis and form the second layer of keratinocytes, or stratum spinosum.
Stratum germinativum (Germinal or Basal Layer):
The basal cells are attached to their neighbors by desmosomes and to the basal lamina by hemidesmosomes.
The cytoplasm is rich in cytokeratin filament (intermediate filament), ribosomes and few mitochondria.
Melanocytes and Merkel’s cells are present in this layer.
This layer is continuously undergoing mitotic division because it is responsible for constant renewal of epidermal cells.
The nuclei are oval and basal with occasional mitotic figures.
It consists of a single layer of basophilic columnar epithelial cells (rich in ribosomes) resting on a clear wavy basement membrane.
Keratinocytes divide, grow, migrate up, undergo keratinization, or cornification.
It represents about 85% of the epidermal cell population.
Langerhans cells.
They recognize, phagocytose and process foreign antigens and then present them to T-lymphocytes for an immune response. So, these cells function as antigen presenting cells (APCs) and are part of the immunologic defense of the skin.
They have no desmosomes, no keratin filaments and no melanosomes (to be differentiated from other cell types).
The most characteristic and unique feature of Langerhans cells are their membrane bound tennis paddle-shaped granules (Birbeck granules). They may contain hydrolytic enzymes, however, their exact function is not yet known
Their nuclei are polymorphic and irregular.
Lysosomes, multivesicular bodies, Golgi apparatus and little endoplasmic reticulum,.
Their long slender processes extend between keratinocytes in the intercellular spaces (Fig. 2).
They display acidophilic cytoplasm and dense nuclei.
Using supravital stains or gold chloride, these cells are identified as star shaped cells.
Langerhans cells cannot be well identified with H&E.
They are mesodermal in origin and distributed between the prickle cells.
Merkel's cells.
It is suggested to be one of the APUD cells.
Touch sensation (mechanoreceptors).
Their nuclei are deep and indented. (Fig. 2).
The cytoplasm contains perinuclear small dense cored granules (of unknown function).
It extends its processes between the adjacent keratinocytes to which they are attached by desmosomes.
Found as single cells parallel to the basal lamina.
Present all over the body, particularly numerous in the tips of the fingers, oral mucosa and bases of the hair follicles.
Sensory or un-myelinated nerve fibers form disc-shaped expansions at the base of Merkel cells.
Present in the stratum germinativum layer near areas of well-vascularized, richly innervated connective tissue.
These cells are derived from the ectodermal neural crest.
Melanocytes
Melanophores are mesodermal in origin and present in the dermis. They are CT phagocytic cells that phagocytose melanin pigments.
Color of the skin is due to the following pigments; endogenous pigment (melanin and hemoglobin), exogenous pigment (carotene).
Both Negros and white people have the same number of melanocytes. So, skin color is dependent mainly on the amount of released melanin.
Determines skin color.
Synthesis of melanin pigments which is essential to protect the skin against ultraviolet rays in sunlight.
No desmosomes are present between melanocytes and keratinocytes.
Their nuclei are pale (euchromatic).
These granules are transferred from one melanocyte to a number of adjacent keratinocytes (melanin carrying cells) to which it is associated, forming “epidermal melanin unit”.
Abundantغزير RER, mitochondria, prominent Golgi apparatus and membrane bound granules (melanosomes).
protein synthesizing cells
In H&E stained sections they are not well demonstrated.
Rounded cell bodies with central nuclei and long cytoplasmic processes passing between the neighboring keratinocytes (Fig. 4).
They are located between the cells of stratum germinativum and also in hair matrices.
They are ectodermal in origin (derived from the neural crest).
It is an avascular layer, which is highly innervated by free nerve endings.
It is ectodermal in origin
It is formed of keratinized stratified squamous epithelium.
Skin pathology
Characteristics of skin
Hypodermis (subcutaneous tissue) is a layer of loose connective beneath the dermis that contains varying amount of fat (NOT a part of the skin) but it represents the superficial fascia that binds the skin to the underlying deep fascia. Its thickness varies according to the nutritional state, activity body region and gender.
The junction between the dermis and epidermis (the dermo-epidermal junction) is formed of dermal projections (dermal papillae) which interdigitate with invaginations of the epidermis called epidermal ridges.
The surfaces of the body are covered either by thin skin or thick skin.
The terms “thick skin” and “thin skin” refer only to the thickness of the epidermis and do not include the layers below it, which can vary in thickness, depending on the location in the body.
It consists of two layers (Fig. 1):
Dermis
Epidermis
The free surface of the skin shows grooves and ridges that form the dermatoglyphics (fingerprints) in the finger pad surfaces.
In humans, skin derivatives include nails, hair and several types of sweat and sebaceous glands.
Its derivatives and appendages form the integumentary system.
The skin is the largest organ in the body (about 16% of the body weight).
autonomic drugs
Parasympatholytics
parasympathomimetics
/Sympathoplegic
Sympathetic depressants are drugs which decrease the activity of the sympathetic nervous system through one or more of the following mechanisms:
Adrenergic neuron blocking agents:
Beta Adrenoceptor Antagonists
Alpha Adrenoceptor Antagonists
Classification of α-drenoceptor antagonists:
α- & β-blockers
Carvedilol
Labetalol
Selective α2 blockers
Yohimbine
Selective α1 blockers
Tamsulosin
Doxazosin
Terazosin
Prazosin
Non-selective αblockers (block α1 & α2)
Phentolamine & Tolazoline
N.B.: Phentolamine should be used with particular caution in patients with ischemic heart diseases or a history of peptic ulcer
They release of histamine from mast cells →→ stimulate GIT motility and enhance gastric acid secretion.
Adverse effect: Gastrointestinal stimulation may result in abdominal pain, nausea, and exacerbation of peptic ulcer.
Block 5-HT receptors.
Competitive non-selective α-blockers.
Adverse effect:tachycardia
و اللتى قد تعتبر
Adverse effect: arrhythmia
Adverse effect: ischemic heart diseases
e.g. myocardial infarction).
Therapeutic uses
Tolazoline
Treatment of pulmonary hypertension of the newborn. To visualize distal peripheral vessels during arteriography.
Phentolamine
To inhibit tissue necrosis caused by extravasation of α-agonist drugs
Due to
Releasing histamine from mast cells that may lead to periphral vasodilation to avoid schemia and also should be limited to avoid anaphlactic shock
Blocking alpha receptors that cause severe hypertention that may lead to ischemic necrosis
Short-term control of hypertensive crises due to:
Ingestion of tyramine-containing foods during the use of nonselective MAO inhibitors.
Abrupt withdrawal of clonidine.
Phenoxybenzamine
The only way the body can overcome this block is to synthesize new adrenoceptors, which requires a day or longer. Therefore, its actions last about 24 hours.
Mechanism:Phenoxybenzamine blocks α1- and α2-adrenergic receptors irreversibly.
Therapeutic use:Inhibition of ejaculation because of impaired smooth muscle contraction in the vas deferens and ejaculatory ducts.
Theraputic use :Treatment of pheochromocytoma either for:
OR: 2) Life-long management of the disease in patients with inoperable cases.
Preoperative preparation of the patient for surgery
Pharmacological effect :Blockade of histamine, serotonin and muscarinic receptors.
Pharmacological effect:Tachycardia due to
enhanced release of norepinephrine (because of α2-blockade) that stimulates β1-receptors in the heart
و الذى يؤدى أيضا الى
Therapeutic use: nasal stuffiness treatment
reflex sympathetic nerve stimulation
Pharmacological effect: Vasodilatation causing a decrease in peripheral resistance
Ergot alkaloids
Contraindications to use of ergot derivatives:
During pregnancy (Except for bromocriptine)?? [oxytoxic effect]
Therapeutic uses of ergot derivatives:
Parkinsonism
To suppress prolactin & growth hormone secretion
Postpartum hemorrhage
Senile dementia
Migraine headache
The vasoconstrictor effect of the above mentioned compounds is induced by partial agonist activity on both α adrenergic and 5-HT2 receptors.
Compounds isolated from the ergot extract:
Ergotoxine
marked α-blocking effect with moderate vasoconstrictor & uterine stimulant effects.
Ergometrine
potent uterine stimulant effect together with moderate vasoconstrictor and α-blocking effects.
Ergotamine
vasoconstrictor with moderate α-blocking effect and uterine stimulant effect.
Pharmacological properties:
Dopaminergic stimulant effect
anti-parkinsonian effect).
inhibition of
prolactin
growth hormone
vomiting
nausea
Uterine stimulant (oxytocic) effect.
Direct vasoconstrictor effect.
Ergot alkaloids are the hydroalcoholic extract of the fungus.
Ergot is a fungus "Claviceps purpurea” that grows parasitically on rye grains.
Pharmacological Properties:
Other actions: block of α1-receptors in the base of the bladder and the prostate decreases resistance to the flow of urine.
Selective α2 antagonists such as yohimbine can increase sympathetic outflow and release of NE from nerve endings →→ rise in blood pressure.
In case of agonists with both α and β2 effects (e.g. epinephrine), α-blockers convert a pressor to a depressor response. This change in response is called epinephrine reversal.
Alpha blockers prevent the pressor effects of α agonists (e.g. Phenylephrine).
Alpha1 blockers inhibit vasoconstriction induced by endogenous catecholamines →→ decrease in peripheral resistance and lowering of blood pressure.
Effect of α-Adrenoceptor Stimulation:
Stimulation of α2 adrenoceptor → suppressing sympathetic outflow.
inhibiting the release of norepinephrine and acetylcholine from nerve endings.
facilitating platelet aggregation.
Stimulation of α1-adrenoceptor → Contraction of arterial and venous smooth muscle.
Guanethidine
The use of guanethidine is restricted to topical application as eye drops for treatment of false
The drug doesn’t pass the blood-brain barrier and have no CNS effects.
Guanethidine depletes يستنزف the stores of NE with impairmentتدهور of the function of the adrenergic neurons.
Both reserpine and guanethidine are no longer used, as they are poorly tolerated.
Reserpine irreversibly inhibits vesicular reuptake of monoamines [reuptake III].
Failure of vesicular uptake of dopamine, NE and 5-HT exposes these monoamines to be metabolized by MAO enzyme →→ depletion of their stores both in the central and peripheral tissues.
Alpha-methyltyrosine (metyrosine)
Crystalluria (due deposition of the drug crystals in the kidney)
this could be avoided by increasing water intake.
psychogenic depression.
, extrapyramidal symptoms
Sedation
It is the only drug which could inhibit biosynthesis of catechalamines in patients with pheochromocytoma
colic and diarrhea due to the unopposed parasympathetic tone.
Increased gastric HCl secretion
Bradycardia and hypotension.
CNS:
Deficiency of dopamine →→ extrapyramidal symptoms (Parkinsonism).
Sedation which may progress to depression.
The site of action of metyrosine includes;
the peripheral adrenergic neurons
adrenal medulla
Metyrosine is a competitive inhibitor of tyrosine hydroxylase; the enzyme responsible for conversion of tyrosine into DOPA (the rate limiting step in biosynthesis of catecholamines).
Adrenergic receptor blocking agents: α- and β-blockers.
These drugs prevent normal physiologic synthesis, storage or release of norepinephrine (NE) from postganglionic sympathetic neurons.
Centrally-acting sympathoplegic drugs:
α-Methyldopa
Contraindicated in patients with:
(apparent) ظاهرى exophthalmos جحوظ العينin case of thyrotoxicosis.التسمم بالثيروكسين اى زيادة نسبته عن الطبيعي
ورم الغدة القظرية.
ورم الغدة الكظرية (can precipitate يسببa hypertensive crisis)
Clonidine
Sudden withdrawal of clonidine is associated with rebound hypertensive overshoot due to sympathetic overactivity, thus, the drug should be stopped gradually.
Sedation, dry mouth and constipation occur frequently.
In alleviating opiate and alcohol withdrawal symptoms.
Prophylaxis of migraine headache and postmenopausal flushing.
Treatment of hypertension, especially if rapid effect is needed (hypertensive urgency).
Site and mechanism of action:
Summation of both effects results in fall in blood pressure and heart rate.
Peripheral α2-adrenoceptors stimulation causes a reduction in release of NE from the adrenergic neurons.
Central α2-adrenoceptor stimulation causes a decrease in sympathetic outflow.
Depression
Active liver disease.
Type B adverse reactions:
Interaction of the drug with the patient’s immune system with the formation of auto-antibodies which may cause hemolytic anemia, aplastic anemia, leucopenia, thrombocytopenic purpura, hepatitis, lupus-like syndrome.. etc.
Type A adverse reactions:
Dry mouth & nasal stuffiness
Hypotension, bradycardia & salt and water retention
Extrapyramidal symptoms
Sedation & depression
Pharmacological action:
Stimulation of presynaptic alpha2 on the cholinergic nerve terminals →→ inhibits acetylcholine (ACh) release →→ decreases GIT secretion & motility.
CVS cardiovascular system
↓↓ sympathetic outflow →→ drop in the blood pressure and the heart rate.
Deficiency of dopamine →→ extrapyramidal symptoms.
Marked sedation, which may progress to psychogenic depression.
Stimulation of central α2-adrenoceptors with subsequentتالى inhibition of sympathetic outflow.
These agents reduce sympathetic outflow from vasomotor center (VMC) in the brain stem.
Sympathomimetics
According to action period
Short acting
Long acting
According to Synthesability
Synthetic
Synthetic مصنعة Sympathomimetics
Indirect-acting Sympathomimetics
Catecholamine reuptake inhibitors:
Cocaine
It penetrates CNS and produces amphetamine-like psychological effects.
It is a local anesthetic with a peripheral sympathomimetic action due to inhibition of both neuronal uptake (uptake-1) of catecholamines and monoamineoxidase (MAO).
Atomoxetine
It is used in the treatment of ADHD.
It is a selective inhibitor of the norepinephrine reuptake transporter.
Drugs that release the stored catecholamine transmitters:
Tyramine
In patients treated with non-selective MAO inhibitors, effect of tyramine is exaggerated, leading to severe hypertension (cheese reaction).
It is inactivated by MAO in the liver and intestine when taken orally. If administered parenterally, it produces an indirect sympathomimetic action.
It is a normal byproduct of tyrosine metabolism in the body and is also found in high concentrations in some fermented foods (such as cheese), chicken liver, chocolate, and smoked fish.
Amphetamine
Amphetamine derivatives
Fenfluramine and dexfenfluramine:
In large doses can cause arrhythmia.
Anorexiogenic drugs acts on 5-HT receptors centrally.
Modafinil
Methylphenidate
Phenmetrazine and diphenmetrazine
Methamphetamine
Contraindications
As epinephrine plus:
With MAOIs.
Prostatic enlargement.
Insomnia
Psychosis and coma.
Dependence
Anxiety, anorexia, insomnia, hallucination and convulsions.
CVS: Palpitations, hypertension, arrhythmias.
Attention-deficit hyperkinetic disorder (ADHD)
Obesity
Narcolepsy
Addiction (dependence): on prolonged use.
Tolerance: occurs to anorexiogenic and psychic effects.
It produces sympathomimetic action like ephedrine with little effect on bronchi.
It decreases appetite (anorexiogenic).
Also it has analeptic and anti-fatigue actions.
It stimulates cerebral cortex, reticular activating system, midbrain and spinal cord. – These effects are manifested as euphoria, increased mental activity, alertness and wakefulness.
Pharmacokinetics: Absorbed and excreted as ephedrine.
Mixed-acting sympathomimetics
Ephedrine
Tolerance and tachyphylaxis.
Urine retention (in old age with senile enlargement of prostate).
CVS: tachycardia, palpitation, angina, arrhythmia, hypertension.
CNS stimulation: insomnia, tremors, anxiety, convulsions and vomiting (CTZ).
Myasthenia gravis (adjuvant with neostigmine).
Nocturnal enuresis
For reversal of hypotension from spinal or epidural anaesthesia (by I.V ephedrine
Attention-Deficit Hyperkinetic Disorder (ADHD).
. Attention-Deficit Hyperkinetic Disorder (ADHD).
Analepticمنشط in toxicity with CNS depressants.
Ephedrine activates α1, β1 and β2-adrenoceptors.
It is decongestant to nasal mucosa; however, it causes rebound congestion.
In the eye, it produces active mydriasis.
Produces VC of blood vessels.
Systemic actions
Skeletal muscles: Stimulant more than epinephrine.
GIT & urinary bladder: contraction of sphincters (α1) and relaxation of walls (β2).
Bronchi: Bronchodilatation (β2), and VC of mucous membrane Bl.Vs.
Blood vessels: ▪ VC of skin and mucous membrane Bl.Vs. → increases systolic & diastolic BP [α- blockers can abolish the hypertensive effect of ephedrine].
Heart: Stimulates all cardiac properties.
It stimulates spinal reflexes.
It stimulates medullary centers and vasomotor center and chemoreceptor trigger zone.
In contrast, it causes sedation in attention deficit hyperkinetic children.
Stimulates cerebral cortex → insomnia, anxiety, tremors and convulsions.
Excreted in urine. Acidification of urine by ammonium chloride increases its excretion.
Metapolism
It is poor substrate to MAO and COMT, so it has long duration of action.
Distribution
Distributed all over the body and passes BBB.
It is absorbed orally and can be given parenterally.
Direct-acting synthetic Sympathomimetics
D1-selective agonists Fenoldopam
Used by IV infusion in hypertensive emergencies.
Its t1/2 is 5 min.
D1-receptor agonist causes VD of arterioles → ↓↓ TPR→ ↓↓ BP.
Headache and flushing.
Beta agonists
Non-elective beta agonists
Non- selective β-agonists Isoproterenol (Isoprenaline)
Tremors
Angina and myocardial infarction.
Tachycardia, palpitation, and arrhythmia.
Heart block.
Bronchial asthma
Metabolic: hyperglycemia.
Uterus: relaxation (β2).
Bronchi: bronchodilatation (β2).
BP: diastolic BP is decreased but the systolic BP may increase slightly.
Blood vessels: VD of skeletal muscle and coronary BV (β2) → ↓↓ diastolic BP → reflex tachycardia.
Heart: stimulates β1→ increase all cardiac properties.
A catecholamine in its chemical structure.
Isoproterenol (Isoprenaline)
Selective beta agonists
Beta 2 selective agonists
Non-Catecholamines beta 2 selective agonists
Long acting nonCatecholamines beta 2 selective agonists
Salmeterol
Formeterol
Short acting nonCatecholamines beta 2 selective agonists
Ritodrine
Sulbutamol and terbutaline
Catecholamines beta 2 selective agonists
Isoetharine
β1-Selective agonists Dobutamine
Prenalterol
Like dobutamine but non-catecholamine and can be used orally.
dobutamine
Headache
Nausea
Tachycardia, palpitation, angina and arrhythmia
Cardiogenic shock
Acute heart failure
Dobutamine is given by IV infusion 2.5-10 ug/kg min.
Increases cardiac output and does not significantly elevates oxygen demands of the heart.
Increasing contractility with minimal increase in hear rate.
Has a major advantage over other sympathomimetic drugs (??)
Catecholamine, directly acting sympathomimetic.
Alpha1-selective agonists
Xylometazoline and oxymetazoline:
used as topical decongestants.
Midodrine
used in treatment of orthostatic hypotension.
Methoxamine
like phenylephrine.
Phenylephrine
Treatment of hypotension
Decongestant
Mydriatic
Non-catecholamine (not inactivated by COMT →→ long duration)
Endogenous
Endogenous Catecholamines
Norepinephrine (Noradrenaline)
Epinephrine (Adrenaline)
Pharmacodynamics
Adrenergic receptors:
Systemic actions:
Other actions: anxiety, tremors and facilitates neuromuscular transmission.
Anti-allergic action: it is a physiologic antidote to histamine.
Metabolic actions:
Hypokalemia: potassium uptake by skeletal muscle cells.
Increased fatty acids concentration (β3).
Hyperglycemia: due to enhanced liver glycogenolysis (β2)
Sweat glands: sweat secretion from apocrine sweat glands of the palm of the hand (non-thermoregulatory sweat).
Uterus: variable with species. It causes relaxation of the pregnant uterus.
Urinary bladder: relaxes wall (β2) and contracts sphincter (α1)
GIT: inhibits tone and motility (β2) and contracts sphincters (α1).
Respiration: bronchodilatation (β2) and decongestion (α1).
Cardiovascular system (CVS) {β1 receptors}:
Blood pressure:
α1-adrenoceptor blockers reverse the hypertensive effect of epinephrine.
↓ Diastolic BP in therapeutic doses (β2 stimulation) and increases it in large doses (α1-receptor stimulation).
↑ Systolic انقباضي blood pressure as a result of COP.
Blood vessels
In the kidney, it stimulates renin release (an enzyme involved in the production of angiotensin II, a potent vasoconstrictor) through β1 stimulation.
VD of skeletal muscle, and coronary blood vessels.
VC of skin and mucous membrane blood vessels and splanchnic area.
Heart: epinephrine increases all cardiac properties.
o Increases force of cardiac contraction (positive inotropic effect) & heart rate (positive chronotropic effect). Therefore, cardiac output (COP) increases. These effects increase oxygen demands of the myocardium. o Increases conduction velocity of the heart (positive dromotropic). o Increases automaticity.
Local actions
Since epinephrine causes VC of ciliary blood vessels with associated decrease in aqueous humor formation, thus can be used in treatment of open angle glaucoma.
Note: In cases of supersensitive a-adrenoceptors [e.g. in thyrotoxicosis, diabetic ketoacidosis, and acute hemorrhagic pancreatitis], epinephrine causes mydriasis.
Eye: decongestion [VC of conjunctival blood vessels], but no effect on pupil size, because it is destroyed by alkalinity of tears.
By inhalation → Bronchodilatation, so can be used in bronchial asthma.
Decongestion and hemostasis because of its intensive VC of skin and mucous membrane blood vessels. Delay absorption of local anesthetics and prolong their duration.
It may be given
endotracheal tube
by inhalation
subcutaneously
The preferred route is intramuscular route.
Epinephrine has a rapid onset but a brief duration of action (due to rapid degradation by MAO and COMT).
Direct agonist acts on α1, α2, β1, β2, β3 adrenoceptors.
According to selectivity
Non selective
Selective
According to their chemical structure:
Non-catecholamines:
According to the mechanism of action:
Both direct and indirect actions e.g. ephedrine.
Indirect-acting either by:
Inhibit reuptake of catecholamines already released e.g. cocaine and tricyclic antidepressants "TCAs".
Release of stored catecholamines from the adrenergic nerve endings e.g. amphetamine.
Direct-acting agonists:
e.g. norepinephrine (NE) and epinephrine.
Autonomic Nervous System (ANS)
Definition: it is the part of the peripheral nervous system (PNS) that controls the involuntary functions of the body e.g. cardiac contractility.
Skeleton
TUMORS OF BONE
secondary
Unknown
Ewing's sarcoma
Prognosis: Aggressive with early metastases, but responsive to chemotherapy.
-X-ray: “Onion skin” periosteal reaction in bone.
Differential Diagnosis: Differentiate from conditions with similar morphology (eg, lymphoma, chronic osteomyelitis) by testing for t(11;22) (fusion protein EWS-FLI1).
Characteristics: Anaplastic small blue cells of neuro-ectodermal origin (resemble lymphocytes).
Location: Diaphysis of long bones (especially femur), pelvic flat bones.
Epidemiology: Most common in Caucasians. Generally boys < 15 years old.
Giant cell tumor
Although most cases are true benign, the tumor can be divided into three grades
Grade III (Malignant type)
Grade II (Locally malignant type)
Grade I (Benign type)
-X-ray : “Soap bubble” appearance
Characteristics: Locally aggressive benign tumor. Neoplastic mononuclear cells that express RANKL and reactive multinucleated giant (osteoclast-like) cells. “Osteoclastoma.”
Location: Epiphysis of long bones (often in knee region).
Epidemiology: 20–40 years old.
Vestigial
Ameloblastoma
Chordoma
Malignant Schwannoma
Liposarcoma
Hematogenic
Plasmacytoma
Lymphoma
Angiosarcoma
Malignant fibrous histiocytoma
Fibrosarcoma
Mesenchymal chondrosarcoma
Chondrosarcoma
Characteristics: lobules of malignant chondrocytes in a background of myxomatous material.
Location: Medulla of pelvis, proximal femur and humerus.
Paraosteal osteosarcoma
Osteosarcoma
Prognosis: Aggressive Primary usually responsive to treatment (surgery, chemotherapy), poor prognosis for secondary.
- X-ray: Codman triangle (from elevation of periosteum) or sunburst pattern
Presents as painful enlarging mass or pathologic fractures.
Pleomorphic osteoid-producing cells (malignant osteo-blasts).
Location: Metaphysis of long bones (often in knee region)
Epidemiology: Accounts for 20% of 1° bone cancers.
Less common in elderly; usually secondary to predisposing factors, such as Paget disease of bone, bone infarcts, radiation, familial retinoblastoma, Li-Fraumeni syndrome.
Peak incidence of primary tumor in males < 20 years.
Either primary or secondary
Mesenchymal
Schwannoma
Fibroma
Lipoma
Vascular
Hemangioma
Fibrohistiocytic
Benign fibrous histiocytoma
Fibrogenic
fibroma
Chondrogenic
Chondromyxoid
Chondroblastoma
Osteochondroma
Characteristics: Lateral bony projection of growth plate (continuous with marrow space) covered by cartilaginous cap. Rarely transforms to chondrosarcoma
Location: Metaphysis of long bones.
Epidemiology: Most common benign bone tumor. Males < 25 years old.
Chondroma
Characteristics: Benign tumor of cartilage.
Location: Medulla of small bones of hand and feet.
Epidemiology: no specific age or sex
Osteogenic
Osteoid osteoma
Characteristics: Similar histology to osteoid osteoma. Larger size (> 2 cm), pain unresponsive to NSAID.
Location: Vertebrae.
Diagnosis: Bony mass ( females.
Characteristics: Presents as bone pain (worse at night) that is relieved by NSAIDs.
Location: Cortex of long bones.
Epidemiology: Adults females.
Osteoma
Microscopic examination: revealed bony mass composed of cortical & trabecular bone architecture.Osteoblasts rimming bone are few & small .Inflammatory infiltrates are typically absent
Characteristics: Associated with Gardner syndrome
Location: Surface of facial bones.
Epidemiology: Middle age.
Bone Infections (Osteomyelitis)
Chronic osteomyelitis:
Syphilis of bones: (See general pathology)
Tuberculous osteomyelitis: (See General Pathology).
Brodie's abscess:
It is a gradual, mild infection occurring in the metaphysis of long bones of children and adults. The com-monest site is the upper end of the tibia. There is a focus of chronic suppuration with a small cavity filled with serous fluid or pus and surrounded by dense sclerotic bone.
Chronic suppurative osteomyelitis: Usually occurs an end result of acute osteomyelitis when the affected bone becomes deformed, with involucrum and multiple cloacae.
Complication of chronic osteomyelitis:
Squamous cell carcinoma from the epithelium lining the sinuses
Pathological fracture.
Acute suppurative osteomyelitis:
Pathological lesions:
The disease may end in chronic osteomyelitis.
Sympathetic effusion in the near-by joints but suppurative arthritis is very rare.
Pathological fracture due to bone destruction and weakening.
Pyaemia from septic emboli due to septic thrombophlebitis.
Septicaemia and acute bacterial endocarditis.
Acute toxaemia with all its effects.
New bone formation (takes placeيحدث)
and this is known as
involucrum
It is usually perforatedتُثقب
By
Multiple openings
Called
Cloacae
Through which pusالصديد may passيعبر
From The medullary cavity
To the outside
and may open through the skin
by multiple sinuses
especially subperiosteally,
by the
irritated osteoblasts,
Thrombosis of the vessels occurs. The thrombosed arteries lead to cut of blood supply leading to necrosis of small and large parts of bone, known as sequestrum
The sequestrum, particularly if small, will be gradually separated from the surrounding living bone by osteoclastic activity.
At the site of infection there is hyperaemia, oedema, leucocytic infiltration with suppuration and pus formation.
The pus spreads along the medullary cavity to be mixed with the fatty tissue of the bone marrow
Pus spreads also along the Haversian canals outwards to accumulate under the periosteum forming what is called a subperiosteal abscess.
The near-by joint is rarely affected due to the firm attachment of the periosteum to the epiphyseal line and because the epiphyseal cartilage resists the extension of infection.
In non haematogenous osteomyelitis, any part of bone may be affected.
Haematogenous osteomyelitis mostly starts in metaphysis of long bones such as femur, tibia and humerus because this area is more liable to trauma and has a rich blood supply.
Trauma: applied to a growing long bone, leads to hematoma formation which is a good media for growth of bacteria.
Sex: It occurs more in boys who are more exposed to trauma.
Age: The commonest age is 2-10 years, which is the period of active growth, but may occur in adults.
Non haematogenous: particularly in adults where the organisms reach the bone directly after trauma, compound fracture, as a complication to infected tooth (osteomyelitis of the mandible) or suppurative otitis media (osteomyelitis of the mastoid bone).
Haematogenous: following septicemia which is the commonest way particularly in children. The organisms usually come from subcutaneous suppurations as boils or abscesses or from the upper respiratory tract as tonsillitis.
Definition: Acute suppurative inflammation of bone with its soft tissues i.e. bone marrow, Haversian canals and periosteum. Causative organisms: The commonest is Staph. aureus. Rarely, especially in chronic cases, it may be due to staphylococcus albus, streptococci, pneumococci and typhoid bacilli. H. influenza in neonates, Salmonella in sickle cell anemia
Routes of infection
Hematogenous route, direct spread from nearby infection or by inoculation through an opened wound, an open fracture or following surgery.
SEPTIC ARTHRITIS
Implant associated infection: Infections associated with artificial implants, where bacteria are introduced during surgery and persist on the surface of the implant in biofilms.
The most common pathogen is coagulase negative staphylococci (CoNS) e.g. S. epidermidis.
Bacteria in biofilms are up to 1000 times more resistant to antibiotics due to their slow replication.
Caused by Staphylococcus aureus, Neisseria gonorrhoeae and Staphylococcus epidermidis in those with a prosthetic joint.
Septic arthritis (SA) is an infection of the joints, to be distinguished from immune-mediated arthritis.
Less commonly caused by fungi.
Caused mainly by bacteria as Staphylococcus aureus, Streptococcus pyogenes and Staphylococcus epidermidis in patients with prosthesis.
Osteomyelitis (OM) is an infection of the bone. It could be acute or chronic.
Diseases of the joints
OSTEOARTHRITIS:
RHEUMATOID ARTHRITIS
Drugs Used in Rheumatoid Arthritis
Selective COX-2 inhibitors
Drugs used in rheumatic diseases:
Counterirritant: methyl salicylate (oil of winter green).
Disease modifying anti-rheumatic drugs (DMARDs).
Non-Steroidal Anti-inflammatory Drugs (NSAIDs) NonNarcotic Analgesics = Antipyretic Analgesics
Mechanism of Action of NSAIDs:
Paracetamol → Selective inhibits COX-3 in CNS.
Classification of Antipyretic Analgesics:
Selective COX-ΙΙ Inhibitors:
Non-Selective COX-Inhibitors:
Pyrazolones: Phenylbutazone, dipyrone & aminopyrine
Anilines: Paracetamol (no anti-inflammatory action).
Salicylates: Aspirin, Na+-Salicylate, Salicylamide, Diflunisal.
Types of Cyclo-Oxygenase Enzymes (COX):
COX-3: present only in CNS → pain & fever.
COX-2: Inducible by inflammation → Pathological:
Infection → toxins → IL-1 & TNF-α → stimulates COX-2 → ↑↑PGs.
Periphery → Inflammation.
CNS
Thalamus → pain.
Hypothalamus [Heat Regulating Center (HRC)] → Fever.
COX-1: Constitutive → Physiological:
Kidney → Renal VD.
Stomach: ↓ gastric acid secretion, and stimulate synthesis of protective mucus (Prevent peptic ulcer).
Aspirin → Acetylation → Irreversible inhibition of COX.
All NSAIDs inhibit Cyclo-oxogenase (COX) enzyme reversibly (except Aspirin) → decrease synthesis of prostaglandins (PGs), prostacyclin (PGI2) & thrmboxane A2 (TXA2).
General characteristics
Most of them (except Paracetamol) have anti-inflammatory and antirheumatic effects = Non-Steroidal Anti-Inflammatory Drugs (NSAIDs).
Relieve pain centrally without narcosis, lower elevated body temperature to normal.
Steroid anti-inflammatory drugs (during flare-ups).
Bone Disorders
Osteomalacia/rickets
rickets
Children with rickets have pathologic bow legs (genu varum), bead-like costochondral junctions (rachitic rosary), craniotabes (soft skull). Skull may remain boxy(cubical) evenحتى after cure and growth
X-rays in rickets
show epiphyseal widening and metaphyseal cupping/fraying in rickets.
cartilaginous growth plates ( only in children).
Osteomalacia
X-rays in osteomalacia:
show osteopenia and “Looser zones” (pseudofractures)
Most commonly due to vitamin D deficiency.
Defective mineralization of osteoid
Paget disease of bone
Constitutive
Hearing loss is common due to auditory foramen narrowing.
Hat size can be increased due to skull thickening.
Increased risk of osteosarcoma.
-Increased blood flow from increased arteriovenous shunts may cause high-output heart failure
long bone chalk-stick fracture.
Stages of Paget disease:
Quiescent—minimal osteoclast/osteoblast activity
Sclerotic phase—excessive collagen formation
Mixed phase —bone destruction by osteoclasts & new bone formation by osteoblasts
Lytic(osteoclastic phase)— destruction of bone trabeculae by osteoclasts
Mosaic pattern of woven and lamellar bone (osteocytes within lacunae in chaotic juxtapositions)
Serum Ca2+, phosphorus, and PTH levels are normal with increased ALP.
Definition: Common, localized disorder of bone remodeling caused by increased osteoclastic activity followed by increased osteoblastic activity that forms poor-quality bone.
Osteopetrosis
Treatment: Bone marrow transplant is potentially curative as osteoclasts are derived from monocytes.
Diagnosis: X-rays show diffuse symmetric sclerosis (bone-in-bone, “stone bone” ).
Complications: Overgrowth of cortical bone fills marrow space→ pancytopenia, extramedullary hematopoiesis. -Can result in cranial nerve impingement and palsies due to narrowed foramina.
Etiology: Mutations (eg, carbonic anhydrase II) impair the ability of osteoclast to generate the acidic environment necessary for bone resorption.
Definition: Failure of normal bone resorption due to defective osteoclasts, with formation of thickened, dense bones that are prone to fracture.
Osteoporosis
Prophylaxis: regular weight-bearing exercise and adequate Ca2+ and vitamin D intake throughout adulthood.
Complication: Can lead to vertebral compression fractures A—acute back pain, loss of height, kyphosis. Also can present with fractures of femoral neck, distal radius (Colles fracture).
Diagnosis: Diagnosed by bone mineral density measurement by DEXA (dual-energy X-ray absorptiometry) at the lumbar spine, total hip, and femoral neck.
One time screening is recommended in women ≥ 65 years old.
Etiology: Most commonly due to increased bone resorption related to decreased estrogen levels and old age(primary type). Can be secondary to
Other medical conditions (eg, hyperparathyroidism, hyperthyroidism, multiple myeloma, malabsorption syndromes).
Drugs (eg, steroids, alcohol, anticonvulsants, anticoagulants, thyroid replacement therapy)
Definition: Trabecular (spongy) and cortical bone lose mass and interconnections despite normal bone mineralization and lab values (serum Ca2+ and PO43−).
Achondroplasia
Etiology: Constitutive activation of fibroblast growth factor receptor (FGFR3) actually inhibits chondrocyte proliferation. > 85% of mutations occur sporadically; autosomal dominant with full penetrance (homozygosity is lethal). Associated with increased paternal age.
Clinically : Membranous ossification is not affected→ large head relative to limbs. Most common cause of short-limbed dwarfism
Definition: Failure of longitudinal bone growth (endochondral ossification) → short limbs.
BONE HISTOLOGY
Bone is a specialized dense hard vascular connective tissue.
CLASSIFICATIONS OF BONE
Histological Classification:
According to bone lamellar arrangement, secondary bone is classified into two types:
Spongy (Cancellous) Bone:
General Organization
There are no complete Haversian systems steum and enclose bone i.e. the osteocytes are located in the branched bone trabeculae with many bone marrow cavities of irregular size inside (Figs. 9 &10) . 111
It appears as branching bone trabeculae and spicules projecting from the inner surface of compact bone, they are covered by endo marrow cavities.
Sites
The center of irregular and flat bones e.g. the skull, scapula, and pelvic bones.
The ends of the long bones (epiphyses) and around its ● central bone cavity.
Compact Bone:
General Organization
Figure 7 Structure of compact bone represents osteon of dried or center of osteon is the darkstaining ground central compact bone. Haversian canal Located in the surrounded by the concentric the lamellae lacunae . The dark, almondshaped structures between the lamellae are that house osteocytes in living bone. Tiny canaliculi radiate from individual lacuna to adjacent lacunae and form a system of communicating canaliculi throughout the bony matrix and within the central canal. 110
Between perioseum and endosteum there are 4 lamellar systems:
Inner circumferential lamellae.
These are several lamellae present parallel to the endosteum.
Interstitial lamellae.
Found between Haversian systems
Haversian systems (osteons):
The outer boundary of each osteon is a more collagen- rich layer called cement line.
Between successive lamellae there are lacunae, each with one osteocyte, interconnected by canaliculi containing the cells' dendritic processes, for receiving nutrients and oxygen from the vessels in the central canal.
In each lamella, the fibers are parallel to each other and follow a helical course.
Each Haversian canal is surrounded by 4–20 bone lamellae
Haversian canal contains blood vessels, nerves and the adjacent canals are connected to each other and to periosteum by Volkmann's canals running perpendicular or oblique to Haversian canals.
Each Haversian canal lined by endosteum.
Lamellar bone arranged in concentric cylinders around a central canal called Haversian canal.
It is formed of a long cylinder parallel to the long axis of bone to form the main bulk the diaphyses.
Outer circumferential lamellae.
It lies immediately beneath the periosteum.
Formed by lamellae running parallel to the surface.
The lamellar bone is formed of osteocytes inside lacunae and canaliculi embedded in calcified collagen fibers.
The bone marrow cavity of the shaft of the long bone is lined by endosteum.
The external surface is covered by periosteum.
It is a mature hard-organized bone tissue.
Sites: It is present where support and strength are needed such as
Inner and outer tables of flat bones e.g. the skull (outer and inner tables of compact bones enclosing a thin layer of spongy bone called diploe).
Shafts of long bones.
Classification according to maturity :
Secondary (mature or lamellar) bone:
Osteocytes are arranged in these concentric lamellae at regular intervals
It is characterized by concentric regular parallel arrangement of collagen fibers.
The matrix is more abundant and more calcified.
It is the mature and permanent form of bone.
Primary (immature or woven) bone:
It can be also found where there is need for rapid bone formation e.g. following fracture.
Later on, it is replaced by mature bone except in certain areas e.g. tooth alveoli and insertion of some tendons.
The mineral content is much less than mature form.
It has irregular or random arrangement of collagen fibers with abundant bone cells.
The first bone tissue to appear in the fetus.
STRUCTURES OF BONE
Histologically, bone tissue is formed of:
Bone cells
Bone contains four types of cells (Fig. 1):
Osteoclasts
The lysosomal enzymes cause lysis of the organic matrix (collagenases, acid phosphatases and proteolytic enzymes)
They secrete excess H decalcification of the bone ions which produce an acidic medium causing (Fig. 4)
Osteoclasts are bone eaters.
bone eater cell)
EM: Active osteoclasts (in bone resorption) are subdivided into four morphological zones:
Basal zone: ● Farthest away from the bone surface is the basal region of the cell it contains it s nuclei, numerous mitochondria, and multiple Golgi stalks.
Vesicular zone: Membrane bounded ve sicles of various shapes and sizes are found between the basal and clear zones. They may extend deeply into the cytoplasm between the ruffled border processes
Clear zone: Peripheral to the ruffled border, it is a ringshaped region. It lacks organelles but contains many actin filaments. The plasma membrane of this region is so closely applied to the bone that it forms the sealing zone
Ruffled border zone: The portion of the cell that is directly involved in bone resorption. Its finger like processes that project into the matrix surface
The surface of osteoclasts adjacent to the bone shows striations that were interpreted as a brush border.
Cytoplasm: acidophilic and strongly positive for acid phosphatase (many lysosomes).
Nucleus: multinucleated (up to 50 nuclei).
They are large cells (up to150 µm)
Site: Motile cells present in shallow cavities known as Howship's lacunae on bone surface at sites of active bone resorption (
Origin: They arise from monocytes as other phagocytic cells.
Non dividing motile cells.
Osteocytes
Osteocytes are involved in the maintenance of bone matrix.
It is the principal cell of mature bone.
bone maintenance cell)
Cell processes of neighboring osteocytes are in contact at their ends to form gap junction to allow flow of ions and molecules from cell to cell.
The cytoplasm is poor in organelles, the nucleus has more condensed peripheral chromatin.
Cytoplasm: pale basophilic.
Nucleus: oval.
Cell bodies send many thin processes that pass through corresponding channels or canliculi in the matrix
Each cell is imprisoned inside one lacuna (not divide).
Appear smaller, branched and paler than osteoblast.
Site: Present singly in bone lacunae.
Origin: Arise from osteoblasts.
Osteoblasts
They have receptors for parathyroid hormone by which it secretes osteoclast stimulating factor that activates osteoclasts to resorb bone.
When osteoblasts are housed in bone lacunae, they become osteocytes.
Deposition of inorganic components of bone matrix.
Responsible for synthesis of the organic components of bone matrix (collagen type I, proteoglycan and glycoprotein).
bone builder cell
EM: Protein secreting cells; contain extensive rER (which account intense basophilia), mitochondria, well developed Golgi apparatus and numerous secretory vesicles.
Cytoplasm
PAS positive granules which are rich in alkaline phosphatase.
Deeply basophilic.
Nucleus: oval and eccentric.
They are large ovoid or polygonal cells
They are non dividing cells.
Site: Located at the surface of bone tissues surrounded by matrix, side by side; in a way resembling simple epithelium.
Origin: Osteoprogenitor cells.
Osteogenic (Osteoprogenitor) cells
Functions: In bone growing and fractures, osteogenic cells are stimulated, divide and differentiate to give rise to osteoblasts.
EM: Scanty cytoplasm contains free ribosomes, small Golgi apparatus and profiles of RER
LM: They are small spindle shaped cells with oval nuclei and pale basophilic cytoplasm.
Site: In the deep layer of the periosteum and endosteum
Origin: Undifferentiated mesenchymal cells and have the ability to divide.
Bone matrix
The extracellular substance of bone which is responsible for its rigidity is formed of two major components:
Inorganic components: Inorganic elements form about 65% of its dry weight. It is composed mainly of calcium and phosphorus. Bicarbonate, citrate, magnesium, potassium and sodium are also present.
Organic component (osteoid): Represents about 35% of the bone formed of:
Ground substance: Form 10% of the organic component and includes:
Bone matrix proteins: osteocalcin and osteopontin.
Glycosaminoglycan: chondrotin and keratan sulphate. hyaluronic acid is also present.
Collagen fibers type I: Form 90% of the organic component and is arranged in lamellae.
Endosteum
Function: Helps bone growth and repair.
Endosteum lines the internal cavities of the bone (bone marrow cavities). It is composed of a single layer of flattened osteogenic cells and osteoblasts.
Periosteum
Shares appositional growth and helps repair after fracture.
Its blood vessels penetrate the matrix to carry oxygen and nutrition.
Provides attachment to tendons, ligaments and muscles. Coarse collagen fiber bundles (Sharpey’s fibers) extend from the outer fibrous layer and penetrate the bone tissue where they are continuous with the collagen fibers of the extracellular matrix.
Periosteum covers the outer surface of bone. It consists of two layers:
Inner cellular layer: It is a cellular layer containing fibroblast-like cells called osteogenic cells. When these cells are stimulated, they divide and give rise to osteoblasts.
Outer fibrous layer: This layer contains dense collagen fibers, fibroblasts and blood vessels.
General characters:
NB. Similar to cartilage, bone is also a special form of connective tissue. In contrast to cartilage, minerals accumulate and are deposited in the cartilage matrix causing calcification of the developing bones. Consequently, bones become hard and can bear more weight, serve as a rigid skeleton for the body, and provide attachment sites for muscles, tendons and ligaments.
It is a dynamic tissue being continuously formed and remodeled under control of varying physiological environmental and hormonal activities.
The bone is a highly vascular tissue.
Its matrix is hard because it is calcified with mineral salts (mainly calcium and phosphorus).
Like all connective tissues, it consists of cells, fibers and ground substances.
Biochemical background
Phosphorus
Excretion
Urine: 60 % of phosphorus is excreted in urine.
Stool: about 40 % of phosphorus eliminated from the body is excreted in feces.
Manifestation
Phosphorus retention is a prominent cause of acidosis in renal disease.
Nausea, vomiting and abdominal cramps.
Tachycardia
Hypocalcemic symptoms:
tetany
Neuromuscular irretability
Hyperphosphatemia
It occurs in the following conditions:
Neoplasm
after chemotherapy
lymphoma
leukemia
Excessive intake.
Endocrinopathies
thyrotoxicosis
hyperparathyroidism
Increase tissue catabolism
hemolysis
shoch
Acute and chronic renal failure.
In DM (diabetes mellitus) there is low concentration of organic phosphorus with higher concentration of inorganic phosphate.
The metabolism of phosphorus is largely related to calcium.
Normal levels:
Plasma
Elevated serum phosphorus levels (hyperphosphatemia) can occur in patients with renal failure due to a poor ability to excrete phosphorus in the urine.
Children: 4 – 7 mg/dl (1.29 – 2.25 mmol/l).
Adults: 2.5 – 5 mg/dl.
10 % is widely distributed in various chemical compounds:
Creatine~P
Coenzymes: TPP, NAD, NADP, FAD, FMN.
Nucleotides: ATP, GTP, CTP, UTP, TTP.
10 % is a combination with:
Carbohydrates (sugar-P).
Lipids (phospholipids).
Proteins (phosphoproteins).
80 % of phosphorus share in bone and teeth formation.
Daily Requirements: ▪ Similar to that of calcium.
Sources and absorption:
Aluminum hydroxide used as antacid interferes with absorption of phosphate due to formation of insoluble aluminum phosphate
The recommended ratio of Ca/P is 1:1 in adults, whereas in infants the ratio starts at 2:1. Such ratios allow the best absorption for dietary phosphate
Sources of phosphorus are similar to calcium
Distribution: ▪ About 80 % of phosphorus is present in bone and teeth. The rest is present in ICF and other tissues.
Proteins
proteins:
The colored prosthetic group does not contain metal
proteins
Non-metallochromo
Chlorophyl
contains magnesium.
Hemocyanin
(oxygen carriers of invertebrate) contains copper.
Haemoglobin
respiratory proteins in which the prosthetic group is the ironcontaining heme.
The colored prosthetic group contains metal
Classification of Proteins
Proteins can be classified according to:
Chemical composition and properties.
Classification according to chemical composition and properties:
Each of these main groups is sub-divided into a number of classes.
Conjugated or Complex Proteins
Chromoprotein
The chromoproteins are composed of simple proteins united with a colored prosthetic group. Many proteins of important biological functions belong to this group. There are two classes of chromoproteins:
Metallochromo
Glycoproteins and proteoglycans.
Nucleoproteins
Conjugated or complex proteins are composed of simple proteins combined with some non-protein substance. The non-protein group is referred to as the prosthetic (addition) group.
Simple Proteins
Eg
Albuminoids or Scleroproteins
Protamins
Histones
Prolamins or Alcohol Soluble Proteins
The prolamins are soluble in 70 to 80% alcohol , but they are insoluble in water, neutral solvents, or absolute alcohol. The prolamins are plant proteins found principally in seeds. Gliadin is acidic protein as it contains high content of glutamic acid and glutamine while
Glutelins
The glutelins are soluble in very dilute acids and alkali but they are insoluble in neutral solvents. They are plant proteins which include gluten of wheat and oryzenin of rice.
Albumin and globulin
Simple proteins are defined as those proteins, which on hydrolysis yield only amino acids or their derivatives.
Derived proteins.
Conjugated proteins.
Simple proteins
Nutritional value.
Classification according to nutritional value:
Low biological value proteins:
Deficient in essential amino acids and not easily digested e.g. collagen and plant proteins
High biological value proteins:
liver
fish
poultry
milk
meat
Contain high amounts of essential amino acids and easily digested
Shape
Classification according to shape:
According to their overall conformation 2 types of proteins can be distinguished:
Fibrous proteins:
e.g.
Collagen in hair
α-keratin
Which have axial ratio of more than 10
globular proteins
e.g
insulin
globulins
albumin
Which have axial ratio (length/width) of less than 10
Calcium metabolism
BioDynamics
Function:
7-Intracellular signaling: Ca described as second messenger to various stimuli including hormones. It binds to intracellular proteins (calmodulin), which mediates the activities of many enzymes and proteins
6-Some hormones like insulin need calcium ions for their secretion and activity.
5-Calcium is important for the activity of some enzymes as α-amylase and glycogen phosphorylase.
4-Blood clotting as well as milk clotting
3- Decreases neuromuscular excitability
2-It is essential for conduction of nerve impulses and normal muscular contraction
1-Calcium is essential element in bone and teeth formation
BioKinetics
Calcium toxicity: Excess calcium supplementation has been associated with formation of "stones" in the body, especially in Gall Bladder and the kidneys.
Excretion: .
Urine: a small amount of calcium is excreted in urine
Stool: Most of the calcium eliminated from the body is excreted in feces (70 – 90 %).
Distribution: .
calcium level:
Hypercalcemia: Increased blood calcium level.
Causes:
Drug induced hypercalcemia
e.g. diuretics
Malignancy due to erosion of bone by tumor
Excess intake of vitamin D
Hyperparathyroidism
Calcium deficiency:
chronic dietary deficiency
Hypoparathyroidism results in:
Very low urinary calcium and phosphorus
Increased alkaline phosphatase activity
Increased plasma phosphate (phosphorus)
Hypocalcemia
Adult→
increased risk of hypertension
depression
teeth decay,
osteoporosis (a deterioration of the bones),
osteomalacia
Children→ rickets
Acute deficiency: Tetany.
Factors affecting blood calcium level:
Plasma proteins:Hypoproteinimia leads to decrease in Ca++ bounds to plasma proteins (albumin & globin) leading to decrease in plasma total calcium
Solubility product (Ca:P ratio and Ca X P product) Normally Ca/ P ratio in blood must be kept constant in children (40) and in adult (50). If plasma phosphate increases, as in renal failure, so the plasma Ca will decrease in it is diffusible ( ionizable form) so the tetany may occur.
Effect of calcitonin: They are secreted by parafollicular cells of thyroid gland "C cells". They lower plasma calcium by:
Increasing deposition of calcium in bone
Inhibition of mobilization from bone.
Increasing Ca++ excretion in urine
Effect of calcitriol (active Vit.D3):
Mobilization of calcium from bone in large doses of vitamin D
Increasing calcium absorption from intestine and renal tubular reabsorption of calcium through increasing the synthesis of mRNA of calcium binding proteins in mucosal cells and renal tubules so it increases plasma calcium.
Effect of parathyroid hormone (PTH): .
▪ PTH increase blood calcium by increasing calcium absorption from intestine and by increasing mobilization of calcium from bone
▪ PTH activates 1-α-hydroxylase in renal tubular cells, thus it is important for activation of vitamin D3.
Ca++Homeostasis
Hormonal regulation of Ca++:
Insulin : stimulate bone formation .
Estrogen → ↑ Ca++ deposition in bone
Glucocorticoids → ↓ Ca ++.
Calcitonin → ↓ Ca++
Thyroid hormone → ↑ Ca++
Growth hormone → ↑ Ca++
Parathormone → ↑ Ca++
Vit. D → ↑ Ca++
Normal levels: - :
Plasma: 9 – 10.5mg/dl
Plasma calcium is present in two forms:
Non-diffusible calcium: 45 %, this is the bound form. It is bound to albumin and is physiologically inactive.
Serum :calcium varies with albumin concentration
Diffusible calcium: 55 %, this is the unbound form, which is either:
Non-ionizable: 5 %, this is inactive form, usually present as calcium citrate.
Ionizable: 50 %, this is the active form which usually present as calcium chloride.
Serum ionized calcium: 4. 5 – 5.6 mg/dl.
Small amounts of calcium are also present in
nerves
muscles
CSFالسائل المحيط بالمخ والحبل الشوكي
plasma
هام جدا
Almost all calcium is present in bone and teeth.
Absorption
Daily Requirements: - Adult males and females: 800 mg/day. - Pregnancy and lactation: 1200 – 1300 mg/day. - Infants under 1 year: 400 – 600 mg/day. - Growing children: 700 – 1400 mg/day
Factors affecting absorption: 1. Proteins and amino acids help absorption. 2. Phytic acid (in cereal grains) and oxalates (tomatoes, tea, Chocolate) hinder calcium absorption. These acids forms insoluble salts with calcium e.g. calcium phytate and calcium oxalate. 3. Fatty acids: impaired absorption of fat due to formation of insoluble Ca-soap. 4. Decreased pH helps solubility and increases absorption. Whereas in alkaline medium (elevated pH), calcium is less soluble and its absorption is low. 5. Phosphate and Ca/P ratio: If Ca/P ratio is high much Ca3 (PO4)2 will be formed (insoluble) and Ca absorption is diminished. 6. Vitamin D: active vitamin D promotes absorption of calcium from intestines. 7. Magnesium level in diet: As magnesium competes with calcium, excess magnesium leads to diminished calcium absorption.
Sources of absorption: ▪ Calcium is present in milk, cheese, egg yolk, beans, nuts, cabbage, cauliflower and green vegetables. ▪ Only 15 % of dietary calcium is absorbed in high protein diet. ▪ In low protein diet, only 5 % is absorbed.
Vitamins
Vitamin C
Requirements: The RDA 70 mg seems adequate to the adult, for children 40 to 45 mg. A lactating woman should receive an additional 30 to 35 mg/day.Excessive vitamin C produces hyperoxaluria (excessive oxalate in urine) as it is converted to oxalic acid in the animal body. 23
Deficiency
Scurvy
It is a disease characterized by:
Anemia due to decreased iron absorption and bleeding
Impaired collagen synthesis that produces:
Defective formation of bone and teeth.
Delayed healing of wounds.
Swollen, spongy and easily bleeding gums.
Increases capillary fragility causing petechial hemorrhages.
Hydroxylation of steroids during the biosynthesis of adrenocortical hormones from cholesterol. 4. Important for synthesis of catecholamines (adrenaline and noradrenaline). 5. Enhances absorption of iron by reducing it from the ferric (Fe+++) to ferrous (Fe++) state. 6. Decreases capillary fragility.
Essential for bone, teeth and blood cells formation.
Formation and maintenance of collagen as it is needed for hydroxylation of proline and lysine, amino acids residues in collagen synthesis
In the body, is catabolized to calcium oxalate which is excreted in urine.
Destroyed by heat , light and storage.
All fresh fruits and vegetables contain some amount of vitamin C.
Vegetables that are the highest sources of vitamin C include: Broccoli, cauliflower, green and red peppers.
Fruits that are the highest sources of vitamin C include:
Citrus fruits such as orange and grapefruit, pineapple, and strawberries.
Chemistry
L-ascorbic acid is a sugar acid presented in two forms:
Oxidized form(dehydro- L-ascorbic acid)
Reduced form (L-ascorbic acid)
Another names
"L-ascorbic acid, Antiscurvy vitamin"
Vitamin d
Hypervitaminosis D
It is due to self medication which leads to
Nausea and vomiting
Stone formation
Increase blood calcium and phosphate
Requirements
800 IU / day for pregnant and lactating female. 128
400 IU / day for children
Vitamin D and diseases
Diabetes mellitus :
Vitamin D levels were closely linked to type 1 and type 2 diabetes. Vitamin D improves insulin sensitivity, insulin secretion and reduces diabetic complications
Autoimmune disease
Vitamin D may protect against autoimmune disease e.g. multiple sclerosis, systemic lupus and rheumatoid arthritis
Infectious disease
In general, vitamin D functions to activate the immune systems . Deficiency has been linked to increased risk of viral infections, including HIV , tuberculosis and influenza
Cancer
Vitamin D supplements can be used to prevent or treatment of cancer. Higher intake or blood levels of vitamin D reduce the risk of colorectal cancer
Nonclassical functions :
Improve insulin resistance.
Hypoglycemic effect.
Anti-hypertensive.
Antiinflammatory. 126
Anti cancer
Classical functions
It is essential for normal bone calcification. It promotes bone calcification by stimulating Ca mineralization and providing calcium and phosphate; in hypocalcemia (belownormal blood calcium) it mobilizes calcium from bone when PTH is also present. All these actions help bring blood calcium levels back within the normal range
Calcitriol helps renal tubular reabsorption of calcium and phosphate.
It increases the absorption follows
Phosphate absorption occur secondary to the absorption of calcium.
The calcium (Ca) binding protein located at the brush border of the intestinal mucosa helps Ca upt ake from the GIT
Calcitriol (active vitamin D can bind calcium
Deficiency of vitaminD:
Renal rickets " renal osteodystrophy":
Who is at Risk of vitamin Ddeficiency
These populations may require extra vitamin D in the form of supplements or fortified foods:
Disease: Fat malabsorption syndromes.
Covered and protected skin.
Elderly: Because the skin of older individuals is less efficient in producing vitamin D3 after exposure to UV.
Dark Skin
Exclusively breast-fed infants.
When renal parenchyma is lost or diseased → Deficiency of 1α hydroxylase enzyme → 1,25 (OH)2 D3 is not formed → Hypocalcaemia →↑ secretion of parathyroid hormone →↑ demineralization of bone → clinical manifestations like that in rickets. Patients must be given1, 25 (OH) or a drug analog that does not require metabolism in the kidney.
Osteomalacia "in adults"
The bone becomes soft → liable to fracture mainly pelvis
It occurs in women with repeated pregnancy and lactation.
Rickets: "in young children"
Decrease active form of vitamin D3→ hypocalcaemia → stimulate secretion of parathyroid hormone from parathyroid gland → increase mobilization of calcium and phosphate from bone "demineralization" → soft bone which lead to:
Increase alkaline phosphatase level in blood.
Low blood calcium and phosphate.
Legs: knock knee and "bow legs".
Pelvis: contracted.
Chest: pigeon chest, rosary beads.
Skull: boxy skull, delay closure of fontanels.
Delayed teething, standing or walking.
Parathormone
This hormone is essential to life .
It a polypeptide hormone
parathormone (PTH) secreted from Chief cells of the four parathyroid glands embedded in the posterior surface of thyroid gland .
Role of PTH
On kidney
PTH stimulates Ca++ reabsorption in so, ↑ blood Ca++ level .
On bone :
Vit. D3 is essential for PTH action on bone.
PTH stimulates bone resorption by increasing activity of osteoclasts ( bone eating cells ) causing demineralization of bone (release of Ca++ from bone to the blood ) so ↑ blood Ca++ level
In calcium homeostasis :
The main function of parathormone is to ↑ Ca++ level and ↓ Po4--- level so as to maintain the solubility product constant .
Normally plasma Po4--- is inversely related to Ca++ and the product of Ca++ Po4--- is constant and called solubility product .
PTH is a major regulating factor for both calcium and phosphate concentrations in extracellular fluids .
Calcitonin
Function : Lowering of blood Ca++ and phosphate levels through:
kidney: increase urinary Ca++ , Na+ , Po4--- excretion . Calcitonin is weak in adult, it is more active in young . Mechanism of action: by increasing cyclic AMP .
Decrease osteoclastic activity → ↓ transfer of Ca++ to blood
decrease formation of new osteoclasts.
It is a polypeptide hormone secreted by parafollicular cells of thyroid gland .
VDR are present in intestinal mucosa, proximal and distal convoluted tubules of the kidney, osteoclast, osteoblast and other tissues.
This complex enters the nucleus and bind with specific site in DNA to stimulate the transcription of specific gene into mRNA.
Calcitriol binds with specific receptors in the cytoplasm called vitamin D receptors (VDR) to form calcitriol receptor complex.
Manifestations
Osteomalacia in adult
Rickets in children .
Actions of 1,25 DHCC :
↓ vit. D → ↓ plasma Ca++ → demineralization of bone
This decreases Ca++ absorption from the intestine which leads to hypocalcaemia so the new bone cannot mineralize.
Stimulate immune system development . Vit. D deficiency
Help development of bone and teeth .
Facilitate Ca++ reabsorption in the kidney .
Increase absorption of Ca++ and Po4--- from intestine . ( main action )
Activation of vitamin D3:
Humans can synthesize calcitriol from 7-dehydrocholesterol derived from cholesterol in the liver.
Three steps are involved, each occurring in a different tissue:
In the kidney: 25-hydroxycholecalciferol is converted into 1, 25-dihydroxy-cholecalciferol "1, 25 (OH)2 D3" by 1α hydroxylase enzyme in the proximal renal tubule cells in response to Para Thyroid Hormone (PTH). (Genetic deficiencies or patients with end-stage renal disease develop renal osteodystrophy because of insufficiency of 1, 25-(OH)2 D3). N.B: 1,25-dihydroxycholecalciferol "calcitriol" is active form of vitamin D3 and is considered as a hormone.
In the liver: Cholecalciferol is converted into 25-hydroxycholecalciferol "25 (OH) D3" by 25hydroxylase enzyme. (Deficient in patients with severe liver disease).
Mode of action of calcitriol:
In the skin: Activation of 7-dehydrocholesterol by UV light in the skin produces cholecalciferol (Vitamin D3). (This step is insufficient in many people in cold, cloudy climates, and vitamin D3 supplementation is necessary.)
Provitamins
Ergosterol "plant sterol" is a precursor of vitamin D2. It is not important as its intestinal absorption is poor.
7-dehydrocholesterol "animal sterol" is a precursor of vitamin D3.
Sources
Milk and butter are poor sources. Vitamin D3, prepared from animal products and then irradiated with UV light, is added to milk and some fortified cereals.
Fish oil, cod liver oil and shark oil are used for drug preparation of vitamin D.
Vitamin D3 is found in saltwater fish (salmon) and egg yolks.
Dietary source required if insufficient exposure to UV light.
Chemistry:
There are many types of vit. D , the commonest of which :
Cholecalciferol "D3"
Ergocalciferol "D2"
It is steroid in nature
"Anti-rachitic Vitamine"
Glycolysis (Anaerobic oxidation of glucose)
Steps: The steps can be summarized as follow:
In aerobic glycolysis
Clinical aspects of glycolysis: There are many diseases associated with impaired glycolysis. They include
Hexokinase deficiency: It leads to hemolytic anemia due to decrease ATP production. In vitro inhibition of glycolysis
Fluoride: Inhibits enolase enzyme. Fluoride-containing tubes are used to reduce glycolysis, in blood samples used for estimation of blood glucose especially when very accurate glucose results are required.
Iodoacetate: By inhibiting glyceraldhyde-3-P dehydrogenase.
Arsenate: By competing with inorganic phosphate in the reaction: Glyceraldhyde-3-P →1,3 bisphosphoglycerate
Pyruvate kinase (PK) deficiency:
Treated with transfusions and/or splenectomies
This leads to excessive hemolysis of RBCs → leading to hemolytic anemia.
ATP is required for Na+ -K+- ATPase which is important for stability of RBCs.
Regulation of glycolysis: By controlling of the three irreversible enzymes (key enzymes). These enzymes are glucokinase (hexokinase), phosphofructokinase (PFK-1) and pyruvate kinase.
Substrate regulation:
Fructose 1,6 bisphosphate stimulates pyruvate kinase.
Citrate inhibits phosphofructokinase-l.
Fructose 2,6 bisphosphate stimulates phosphofructokinase-1.
Glucose-6-phosphate inhibits hexokinase (and not glucokinase).
Energy regulation:
High level of ADP and AMP stimulate PFK-1.
High level of ATP inhibits PFK-1 and pyruvate kinase.
Hormonal regulation;
Glucagon: Inhibits the activity of all key enzymes of glycolysis. It is secreted in response to low blood glucose level (starvation).
Insulin: Stimulates synthesis of all key enzymes of glycolysis. It is secreted after meal (in response to high blood glucose level).
Substrate level phosphorylation in glycolysis: This means phosphorylation of ADP to ATP at the reaction itself. In glycolysis there are 2 examples:
Phospho-enolpyruvate + ADP
1, 3 Bisphosphoglycerate + ADP --> 3 Phosphoglycerate + ATP
Glycolysis Is Irreversible
Three enzymes in the pathway catalyze reactions that are irreversible. When the liver produces glucose, different reactions and therefore different enzymes must be used at these three points:
Pyruvate kinase
PFK-1 phosphofructo kinase-1
Glucokinase/ hexokinase
Differences between glucokinase and hexokinase:
Generally, glycolysis can be divided
Net gain of energy 2 ATP.
2nd phase: (Energy producing) phase: It includes second set of 5 reactions. Each glyceraldehyde 3-phosphate is converted to pyruvate (aerobic) or lactate (anaerobic). It releases 4 ATP molecules.
1st phase: “Priming” (Energy requiring) phase: It includes the first 5 reactions. Glucose is converted into two molecules of glyceraldehydes 3- phosphates. It uses two molecules of ATP.
In the presence of oxygen, NADH+H+ is oxidized in the electron transport chain in the mitochondria to produce ATP .
In anaerobic glycolysis
In muscle tissue under hypoxic conditions, the energy needs of the tissue may be partially supplied by anaerobic glycolysis
LACTIC ACIDOSIS
Convulsions, shock, uncontrolled hemorrhage, or conditions that interfere with circulatory function can cause lactic acidosis
Conditions that cause decreased oxygenation of tissues force on anaerobic glycolysis for energy production, with excessive lactic acid buildup dependence in tissues and spillover into the blood. 6
Decreased pH interferes with function of the contractile machinery of the muscle d. E . levated muscle lactate accounts for fatigue and pain induced by strenuous exercise.
Accumulation of lactic acid causes a decrease in muscle cell pH
Lactate buildup during anaerobic glycolysis limits the extent to which muscle can obtain energy by this means
In cells that are unable to transfer electrons to oxygen due to lack of mitochondria, e.g., RBCs, or in vigorously exercising muscle cells ( anaerobic conditions is regenerated by giving its hydrogen to pyruvic acid to form lactic acid.
Site: Cytoplasm of each cell, if a cell has mitochondria and oxygen, glycolysis is aerobic. If either mitochondria or oxygen is lacking, glycolysis may occur anaerobically so it is of high physiological importance in mature RBCs, cornea and lens due to absence of mitochondria and in muscle due to lack of oxygen during muscular exercise.
Glycogen
Storage Diseases
Metabolism
CONNECTIVE TISSUE
GROUND SUBSTANCE (MATRIX)
Glycosaminoglycans (GAGs): of two types;
Glycoproteins: formed of protein and monosaccharides e.g. fibronectin, chondronectin and osteonectin.
Proteoglycans: formed of protein core and glycosaminoglycans.
None sulfated e.g. hyaluronic acid.
Sulfated e.g. heparin, keratan, chondroitin and dermatan sulfate.
General Characters:
Additional Functions
The hematopoietic tissue is specialized for haemopoiesis (blood cell formation).
The adipose tissue serves as energy storage and thermal insulator.
Repair Function
In response to tissue injury, the fibroblasts migrate, proliferate and deposit abundant new collagen fibers resulting in the formation of fibrous scar tissue
Defensive Functions:
Physical barrier against microorganisms.
Local response to infection (acute inflammation).
Formation of antibodies.
Phagocytic function.
Metabolic function
It provides pathway for diffusion of nutrients, oxygen and waste metabolites between blood and other tissues.
Structural support:
it either :
or connects different types of tissues together (tendon)
Or acts to fill the spaces (packing) between organs or tissues (loose type),
maintains the anatomical form of the organs and systems (capsules)
Special types of connective tissue:
Bone
Cartilage
Connective tissue proper.
The connective tissue consists of
extracellular material called matrix
The matrix consists of
ground substance within which these fibers are embedded
The ground substance may be:
Hard as in bone.
Rubbery as in cartilage.
Gelatinous as in areolar tissue.
Liquid as in blood.
GROUND SUBSTANCE (MATRIX) general characteristics
Connective tissue proper can be classified according to the proportion of connective tissue components (cells, fibers and matrix)
Types of connective tissue proper
Dense Connective Tissue
Dense Irregular Connective Tissue
it is composed of:
Few cells mainly the fibroblasts
Mainly collagen fibers arranged in different directions (may be elastic fibers)
The orientation of the fibers in different make this type withstand stresses on various directions
Dense Regular Elastic Connective Tissue
Dense Regular Collagenous Connective Tissue
It is resistant to stress in one direction.
This type has abundantوفير fibers and few cells embedded within the little matrixDense regular connective tissue
Loose Connective Tissue
It has the following types:
Adipose Connective Tissue
Mesenchymal Connective Tissue
Mucous Connective Tissue
Reticular Connective Tissue
Loose Areolar Connective Tissue
This is cellular connective tissue with thin sparse fibers and abundant matrix.
Connective tissue proper is characterized by cells and fibers embedded in a soft ground substance.
protein fibers
CONNECTIVE TISSUE FIBERS
Elastic Fibers.
Reticular Fibers.
Collagen Fibers.
different cell types
CONNECTIVE TISSUE CELLS
Free or transient (wandering or immigrant cells).
Leucocytes
Free macrophages
Plasma cells
Mast cell
Fixed (resident) cells.
Fixed macrophages
Pericytes
Reticular cells
Adipose cells
Multilocular Adipose Cell.
Unilocular Adipose Cell
Endothelial cells
Fibrocytes
Fibroblasts
Undifferentiated Mesenchymal cells
It originates from embryonic mesoderm (mesenchyme).
Connective tissue is one of the four basic body tissues.
Lower limb
Upper Limb
Responsible nerves
The brachial Plexus
Cords
The posterior divisions of the three trunks unite to form the posterior cord.
Branches from the posterior cord:
A: axillary nerve (C5,6).
N: nerve to latissmus dorsi (C5,6,7).
L: lower subscapular nerve (C5,6).
U: upper subscapular nerve (C5,6).
The anterior division of the lower trunk alone forms the medial cord.
Branches from the medial cord:
Ulnar nerve (C7, 8 & T1).
Medial root of median nerve (C8, T1).
Medial cutaneous nerve of the forearm (C8, T1).
Medial cutaneous nerve of the arm (C8, T1).
Medial pectoral nerve (C8, T1).
The anterior divisions of the upper and middle trunks unite to form the lateral cord.
Branches from the lateral cord:
Musculo-cutaneous nerve (C5,6,7).
Lateral root of median nerve (C5,6).
Lateral pectoral nerve (C5,6).
Trunks
Divisions: each trunk divides into anterior and posterior divisions.
The ventral rami of C8 and T1 unite to form the lower trunk.
The ventral ramus of C7 alone forms the middle trunk.
The ventral rami of C5 and C6 unite to form the upper trunk.
Branches from the upper trunk:
Suprascapular nerve (C5,6).
Nerve to subclavius (C5,6).
Roots: the ventral rami of 5th - 8th cervical nerves and part of 1st thoracic nerve. Sometimes fibers from C4 join the brachial plexus (prefixed). Also, fibers from T2 may join the plexus (postfixed).
Branches from the roots:
Branches to the scalene muscles.
Branches to the longus coli muscle.
Root to phrenic nerve C5.
Long thoracic nerve to serratus anterior muscle from C5, 6, 7.
Dorsal scapular nerve C5.
The roots are present in the root of the neck and the trunks are present in the posterior triangle of the neck. The divisions are present in the cervico-axillary canal. The cords are present in the axilla.
It has four stages: roots, trunks, divisions, and cords. (fig.1)
It is the nerve plexus of the upper limb. It provides the sensory and motor supply to the upper limb except one muscle (trapezius) and an area of skin (medial side of the upper arm)
The Hand
The Forearm
Posterior compartment of the forearm
Deep group
Extensor indicis
Extensor pollicis longus
Extensor pollicis brevis
Upductor pollicis longus
Supinator
Superficial group (
مجموعة ٣
Anconeus
مجموعة ٢
Ext. carpi ulnaris
Ext. digiti minimi
Ext. digitorum
Ext. carpi radialis brevis
مجموعة ١
Ext. carpi radialis longus
Brachioradialis
The anterior compartment:
Deep Flexors group:
Pronator Quadratus
Flexor Pollicis Longus
Flexor Digitorum Profundus
Superficial group
Flexor carpi ulnaris.
Flexor digitorum superficialis.
Palmaris longus.
Flexor carpi radialis.
Pronator teres.
The Arm
Cubital fossa
Contents of the cubital fossa: from medial to lateral (Fig.2):
The biceps tendon
The end of the brachial artery and the beginning of the ulnar and the radial arteries.
Median nerve on the medial side of the brachial artery.
Boundaries (Fig.1):
Roof: formed by the skin, superficial fascia, the deep fascia and the bicipital aponeurosis.
The superficial fascia of the cubital fossa contains the following:
Lateral and medial cutaneous nerves of the forearm.
Basilic and cephalic veins, and the median cubital vein connecting them.
Floor: formed by two muscles; the brachialis medially and the supinator laterally.
Laterally: the medial border of the brachioradialis muscle.
Medially: the lateral border of the pronator teres muscle.
Base: imaginary line between the two humeral epicondyles
It is a triangular depression lies in front of the elbow joint.
Posterior compartment
The triceps muscle
Anterior compartment
The brachialis muscle
The coracobrachialis
Biceps brachii
Shoulder region
Entermuscular spaces
Lower triangular space
The profunda brachii vessels.
The radial nerve.
Laterally: the shaft of the humerus.
Above: the teres major muscle.
Upper triangular space
Contents: Circumflex scapular vessels.
Laterally: the long head of triceps.
Above: the subscapularis (in front) and teres minor (behind), and the lateral border of the scapula in between.
Quadrangular space:
The posterior circumflex humeral vessels.
The axillary nerve.
Laterally: the surgical neck of the humerus.
Medially: the long head of triceps.
Below: the teres major.
Above: the subscapularis (in front) and the teres minor (behind), and the capsule of the shoulder joint in between.
Rotator cuff muscles
Teres minor.
Subscapularis
Infraspinatus
Supraspinatus
Teres major.
Deltoid
Pectoral region
Cavities
Axilla
Fascia
Clavipectoral fascia
Structures piercing the clavipectoral fascia:
Lymph vessels.
Lateral pectoral nerve.
Cephalic vein.
Characteristics
Below, the two layers enclose the pectoralis minor muscle, fuse to each other and become attached to the axillary fascia where they form the suspensory ligament of the axilla.
Above, the two layers enclose the subclavius muscle and become attached to the lower surface of the clavicle.
Double-layered sheet of fibrous tissue which extends between subclavius and the pectoralis minor muscles deep to the pectoralis major muscle.
Muscles and tendons
Serratus anterior muscle
Pectoralis minor muscle
Pectoralis major muscle
Blood supply
Nerves
Bones
Humerus
Sternum
Costal cartilages
Rib
Clavicle
Scapula
Superficial muscles of the back
Latissmus dorsi.
Trapezius
Deep muscles of the back
Rhomboidus major.
Rhomboidus minor.
Levator scapulae.
Muscles
Muscle contraction and relaxation
Changes accompanying muscle contraction
Mechanical changes:
Relation between muscle length and tension:
Within limits, the greater the initial muscle length (preload), the more will be the tension developed in isometric contraction”
حتى حد معين، كلما زاد طول العضلة الابتدائي ،كلما كان الشد أقرب الى انقباض ايزومتري(ثابت الطول)
Parasites affecting the musculoskeletal system
Sarcocystosis
Trypanosoma cruzi,
Toxoplasmosis
Helminthes
Trichinosis
Hydatid cyst,
Cysticercosis
Sparganosis
There are 2 types of contraction:
Isometricالطول ثابت
e.g. when the weight is too heavy to be moved.
Zero (no work done)
Great waste heat
Short
no work)
waste heat
SE stretched ● constant length.
Increased
Isotonicالشد ثابت
e.g. contraction of biceps to lift objects
Mechanical efficiency and work done
25-30%
Heat production
Less
O2 required G
Greater
Longer
Sliding
Great sliding
Energy
Great and used for work and waste heat
Contractile element (CE), and serial element (SE).
SE not stretched → shortening
CE shortens
Muscle tension
Constant
The muscle length
Decrease
But overstretching →↓ number of cross bridges →↓tension. This law is applied also in the cardiac and smooth muscles as it is myogenic law (depend on the muscle not on the nerve supply).
The increase in muscle length leads to increase number of cross bridges→ ↑tension.
Starling law
Muscle length:
Optimal length: is the length at which we get the best contraction.
Equilibrium length: is the length of relaxed and detached muscle from bony attachment
Resting length: is the length of unstimulated muscle
Muscle tension: Represented by the degree of stretch on elastic component.
Total tension = passive tension + active tension in isometric cont.
Active tension: is the increase in tension during contractio
Passive(rest) tension: is that exerted by unstimulated muscle.
In the skeletal muscle there are:
2 elastic elements:
Serial element-SE or tendon is in series with CE.
Parallel Element-PE or capsule which is parallel to the CE
Contractile element (C.E)
When the muscle is stimulated to elevate a load, the two types occur; isometric contraction at first to produce tension equal to the load then isotonic contraction to elevate the load.
Excitability and ionic changes:
Electrical changes:
Compare between muscle and nerve
Nerve
Muscle
Chronaxia
Rate of conduction
Duration of spike P.
Amplitude of A.P.
Overshoot to
Firing level
RMP
It is similar to the nerve with the following differences:
occurs before contraction:
Mechanism of muscle relaxation
So, ATP hydrolysis is required for contraction and relaxation and without ATP relaxation will not occur.
↓↓ intracellular Ca++ ions → the troponin-tropomyosin complex return to its original position→ separation of myosin head from actin sites → muscle relaxation.
The Ca++ is actively reuptaken back to the SR by active Ca++ pump to be stored in the cisterns (Ca++ pump need breakdown of ATP).
Mechanism of muscle contraction
Results of contraction
H-zone becomes narrow.
The width of A band is remained constant.
The width of I band is decreased.
The sarcomere becomes short.
Molecular basis of contraction (ratchet, walk along or sliding theory):
The more the cross bridges the stronger the contraction.
After tilting of the myosin head, ATP bind to myosin head → detachment of the myosin head from actin sites → moves back to its normal direction → attach to a new active site and repeat the cycle.
The head tilts towards the arm and drag the actin filament towards the center of the sarcomere (H zone). This tilt is called power stroke.
Once the actin filaments become activated by Ca++, the heads of the cross bridges attach to the active sites of actin.
Excitation - contraction coupling: It is the process by which depolarization of the muscle fiber initiate contraction. It passes with the following steps:
The interaction between actin and myosin heads leads to sliding of actin filaments between myosin filaments → muscle contraction.
The concentration of Ca++ increases and initiates contraction by binding to troponin-c leading to:
Movement of tropomyosin laterally into the groove between the thin filaments → uncovering the binding sites of actin for the myosin heads.
Weakness of the binding of troponin I to actin.
This action potential triggers the release of Ca++ ions from the terminal cisternae of sarcoplasmic reticulum.
When the EPP reaches the firing level → action potential that propagates along the muscle membrane and transmitted to all fibres via the T tubules.
Ach combines with the cholinergic receptors on the muscle membrane ↑↑ Na+ permeability → depolarization of the membrane (End plate potential).EPP
When a nerve impulse reach the MEP motor end plate, it leads to Ach release from the nerve terminals.
Neuromuscular Transmission
Synapse
Structure of the synapse:
Mechanism of chemical transmitter release at the chemical synapse:
It is known that stimulation of the post synaptic receptors may either cause excitation in the post synaptic neuron (EPSP) or may cause inhibition in the post synaptic neuron (IPSP). This depends mainly in the nature of the released chemical transmitter from the synaptic vesicles and its effect on ions permeability across post synaptic membrane.
A postsynaptic potential is then generated in the postsynaptic membrane.
The chemical transmitter moves by simple diffusion to the receptors on the postsynaptic membrane where it activates them.
The vesicles get attached to specific release sites at the presynaptic membrane, then, they rupture, and the chemical transmitter is released in the synaptic cleft.
Ca+ + binds with the wall of the synaptic vesicles.
Presynaptic membrane voltage-gated Ca2+ channels are opened allowing Ca2+ influx into the cytoplasm.
When the action potential reaches the synaptic knob, its membrane is depolarized.
These vesicles are of two types:-
Granular type (contains neuropeptides which are slowly acting, their actions extend for days or years)
Clear type (contain rapid acting chemical transmitter acts for seconds)
If these knobs end around the dendrites of the post synaptic neuron, the synapse is called axodeneretic synapse which is the most common, if it end, on soma we get the axosomatic or if it ends around axon we get the axo- axonic synapse (rare type).
The presynaptic nerve ending shows a swelling called the synaptic knob. The chemical transmitter is stored in the synaptic knob in small vesicles called the synaptic vesicles.
The neuron that transmits impulses towards the synapse is called presynaptic neuron (its membrane is termed presynaptic membrane) and the neuron that transmits impulses away from the synapse is called postsynaptic neuron (its membrane is termed postsynaptic membrane).
There are two types of synapses:
Electrical synapse
in this type there are direct protein channels between adjacent cells that permit ion passage with very low resistance from inside one cell to another, they are called gap junctions. They are found in heart and smooth muscles and very few in C.N.S.
The chemical synapse
i.e. impulse is transmitted from one neuron to the other through release of chemical substance called chemical transmitter. More than 40 types of transmitters are known but the most important are acetylcholine, catecholamines, histamine, serotonin, dopamine, gamma aminobutyeic acid GABA, and glycine. Most synapses in human are chemical synapses, e.g. synapse in autonomic nervous system
the nerve impulse may be:
Integrated with impulse from another neuron.
Changed from one impulse to repetitive stimuli.
Transmitted to the second neuron.
Inhibited
Definition: it is the junctional area [a cleft that is 30-50 nm (1 nm= 10-9 m) wide] between two neurons, or between a neuron and an effector organ (muscle or gland).
Properties of neuromuscular transmission:
Effect of ions
↑ Mg++→ ↓ release of Ach →↓ transmission.
↑ Ca++ ↑↑ release of Ach ↑↑ transmission.
Drugs affect the neuromuscular transmission:
Blockers (muscle relaxing)
Succinylcholine: depolarizing blocker.
Curare: competitive inhibitor.
Stimulators
Anticholinesterase drugs (Prostigmine)
Ach-like drugs (carbachol).
The 10 folds safety factor: i.e. the number of Ach molecules is 10 mes more than the number of Ach receptors.
Fatigue: after repeated stimulation due to exhaustion of Ach.
Synaptic delay: is the time needed for the release of Ach and its effect on the muscle (0.5 msec).
Unidirectional: the impulse passes from the nerve to the muscle only.
Structure of the motor end plate (MEP):
MEP is the area between a nerve fiber and muscle fiber.
Neuromuscular transmission (The end plate potential, EPP):
Miniature end-plate potential: Spontaneous rupture of some Ach vesicles → subthreshold depolarization in MEP without action potential in the muscle fibre.
Then repolarization occurs by ↑K+ permeability and Na+-K+ pump.
Ach is rapidly hydrolyzed by cholinesterase in the cleft to prevent reexcitation of the muscle.
The EPP spread along the muscle fibre in both directions.
Ach combines with specific receptors in the muscle membrane → ↑↑Na+permeability via Na+ gates → partial depolarization of MEP → reaches the firing level → action potential.
Ach passes into the synaptic cleft.
Stimulation of the nerve causes Ca+2 influx into nerve terminals → Ach vesicles binds to the dense bars in axon terminals and ↓↓ the viscosity of the intracellular fluid →fusion of Ach vesicles to the presynaptic membrane → rupture of Ach vesicles and release of Ach by exocytosis.
The muscle fiber
membrane has invagination called synaptic gutter and subneural clefts to increase surface area of Ach effect.
Synaptic cleft
is a distance (200-300 A°) between end of nerve (sole foot) and muscle fiber, in which Ach is released from the nerve to stimulate the muscle and contain cholinesterase enzyme which hydrolyze Ach
The motor nerve
Loses it myelin sheath and branches into many sole foots (to increase the surface area) which contain large number of mitochondria, acetylcholine vesicles and dense bars. These foots are covered by neurolemma which continue with the sarcolemma of muscle fibers.
Parasitology
Classifications
Physiological classification:
Cvs
كارديو متحدد
قائمة التحديدات
تحديدات••CVS••
●ANATOMY
Common is common
●BIO
Written
Cholesterol metabolism
Lipoprotein Metabolism
Mcq
Cholesterol metabolism
Lipoprotein Metabolism
Ketone bodies metabolism
●MICRO
Written
Hemorrhagic fever
Mcq
All topics
●PATHOLOGY
Rheumatic fever
Myocardial infarction
Aneurysm
مهم جدول المقارنه
Comparison Between
Acute bacterial endocarditis
Subacute bacterial endocarditis
Rheumatic fever
●PHARMA
Mcq
Heat failure
Arrhythmia
●PHYSIYO
Witten+MCQ
1-Regulation of blood pressure
2- Regulation of Cardiac output
3- Venous circulation
MCQ الباقى
●HISTO
*Written Questions topics:
1- Cardiac Muscle.
2- Purkinje Muscle Fibers.
3- Smooth Muscle.
4- General Structure of the Blood Vessels.
5- Arteries (Large Elastic, Medium Sized, Small Arteries).
6- Blood Capillaries.
7- Veins (Venules, Small, Medium Sized, Large Veins).
*MCQs and OSPE exams:
**Special Medium Sized Arteries, Lymphatic vascular system and A-V anastomosis (MCQs)
All the curriculum will be covered
Microbiology
Infectious
Mode of infection : infection of the myocardium most frequently occurs following hematogenous spread of the bacteria or virus to the heart muscle
Helminths: Echinococcus, Trichinella
Fungi: Aspergillus, Cryptococcus, Candida
Bacteria: Corynebacterium diphtheria, Salmonella, Borrelia, Mycobacterium tuberculosis
Corynebacterium diphtheria
The exotoxin diffuses to blood stream and can affect heart leading to myocarditis accompanied by arrythmias and circulatory failure and death may occur.
It is transmitted by droplet infection, the organism multiplies locally releasing the exotoxin causing inflammation of the throat, local necrosis and formation of pseudo-membrane.
Diphtheria is a serious infection caused by Corynebacterium diphtheria, which produce a powerful exotoxin. Nowadays diphtheria is extremely rare after mass world immunization.
MYCOPLASMA
Treatment: ▪ Tetracyclines, Macrolides (erythromycin or azithromycin)
Serology
Detection of cold agglutinin: anti-mycoplasma antibodies cross-react with type O RBCs and agglutinate them but only at low temperatures (4ºC) ( Heterophil antibody )
Detection of IgM or a rising titer of IgG by ELISA.
Direct detection of:
nucleic acid using PCR or DNA probes.
Antigens by immunofluorescence.
Important pathogens and Diseases:
U. urealyticum and M. genitalium: cause non-gonococcal urethritis.
M. hominis: causes postpartum fever.
M. pneumoniae: causes atypical pneumonia and also can cause myocarditis.
General characteristics: ▪ Mycoplasma are the smallest free-living bacteria in nature. ▪ They are unique in that they do not possess cell wall, therefore drugs that inhibit cell wall synthesis (penicillin, cephalosporins and vancomycin) are ineffective against mycoplasma. ▪ Mycoplasma also have a plasma membrane reinforced with cholesterol; a sterol usually found in eukaryotic cells. ▪ On culture, it give a fried-egg appearance after a few weeks of culture (the center of the whole colony is characteristically embedded beneath the surface). ▪ They spread by direct contact or respiratory droplets.
Borrelia burgdorferi (Lyme disease)
Ceftriaxone (IV) for later-stage disease
Doxycycline (oral) for primary-stage Lyme disease
Diagnosis: based on clinical finding and history of tick bite.
Other diagnostic tests include PCR.
Serology: detection of anti B. burgdorferi antibodies in serum by ELISA.
Skin biopsy may be cultured for B. burgdorferi.
If the patient presented with the skin lesion ECM, biopsy from leading edge is examined by dark field microscopy for motile spirochetes
Disease: Lyme disease
Late manifestations which may last for months or years: arthralgia, and migrating arthritis due to immune complex deposition.
Initial symptoms: erythema chronicum migrans (ECM) is annular skin lesion at site of bite with an erythematous leading edge and central clearing "bull's eye" associated with fever, chills, muscle pain and headache, figure (37).
B. burgdorferi invades skin and spreads via blood to involve primarily the heart, joints, and CNS.
Mode of transmission: transmitted to man by tick bite.
Borrelia burgdorferi is a large spiral shaped bacteria with wide irregular coils.
Chlamydia
Viruses: Coxsackie A and B, Influenza virus, Hepatitis viruses, Poliomyelitis, Cytomegalovirus, Human immunodeficiency virus, Epstein-Barr virus
Parvoviruses
Immunocompromised patients may require IV immunoglobulins.
Supportive care , blood transfusions may be needed
Diagnosis • Serology by ELISA • Detection of viral nucleic acid by PCR
Diseases: Human parvovirus B19 is the causative agent of many diseases:
myocarditis
Aplastic anemia (especially in patients with sickle cell anemia)
Immunocompromised individuals may develop a severe chronic anemia
erythema infectiosum,( slapped cheek syndrome): bright red rash mainly in cheeks and flu-like symptoms. Immune complex deposition is the cause of red rash and arthralgias.
It is ssDNA, naked virus with icosahedral capsid. ✔ It is also one of the five most common pediatric viral exanthems (diseases that cause a rash). ✔ Transmitted by the respiratory route, transplacental or by blood transfusion.
Adenoviruses
Lab. Diagnosis: Virus isolation, Antigen or antibody detection by ELISA or PCR
Diseases: Transmission occurs by respiratory droplets, fecal-oral, or direct contact. Most infections are mild and give long life immunity.
Gastrointestinal diseases: Gastroenteritis in infants
Eye diseases: swimming-pool conjunctivitis
Respiratory tract diseases: e.g. acute febrile pharyngitis
Adenovirus was first isolated from adenoid tissue, hence the name. Adenoviruses can infect several organs in the human body They are : ● Non-enveloped DNA virus. ● Icosahedral nucleocapsid. ● Has a unique fiber protruding from each of 12 vertices of its capsid, this fiber helps in the attachment of the virus to the host cell. ● Replicates in host cell causing cell lysis with viral release from the cell. ● There are about 52 serotypes.
Coxsackie viruses
Lab. diagnosis: Serological tests such as ELISA and genetic tests as PCR
Group B coxsackieviruses are responsible for cardiomyopathy (acute myocarditis and pericarditis), aseptic meningitis, and pleurodynia.
Group A coxsackieviruses are responsible for herpangina (fever and painful blisters in the mouth) and hand-foot-and- mouth disease.
The Coxsackie viruses are RNA viruses that have an icosahedral capsid. belong to the picornavirus family. Transmitted by fecal-oral route and also through droplets.
Hemorrhagic fever
Yellow Fever
Replicative cycles:
Urban yellow fever cycle (urban cycle)
Treatment: only symptomatic
A live attenuated vaccineprepared from an attenuated 17D strain (17D vaccine) in eggs , the vaccine is obligatory to travelers from and to endemic areas . Those having egg allergy should consult doctors before taking it.
Mosquito control
on airplanes going to or coming from these areas.
in endemic areas as in equatorial countries of Africa and South America
Disease severity:
3 rd stage (intoxication stage): about 15% of cases suffer from vomiting, diarrhea, bleeding and multi-organ dysfunction with liver and renal failure.
2 nd stage (remission stage): in which symptoms disappear and most patients recove r rmost patients recover from this stage
1 st stage: a mild one. The patient develops fever, headache, sore throat, malaise and myalgia.
The virus is transmitted from human to human by the domestic mosquito Aedes aegypti. This is called urban yellow fever. This may occur in epidemics
When infected persons return to urban areas
Jungle yellow fever cycle (sylvan cycle)
Humans become accidentally infected if they visit the forests.
The virus is transmitted from monkey to another by mosquito Aedes africanus in Africa and haemogogus in south America.
monkeys serve as the main reservoir
occurs in tropical forests
Mode of transmission: mosquito-borne illness
Natural reservoirs: tropical forests monkeys
Distribution: Africa and South America.
Dengue fever
Nonsteroidal analgesics are avoided as they affect the bleeding tendency of the patient.
symptomatic treatment
Supportive
Hematological tests:
Hematocrit value is lowered.
WBCs count is lowered
Detection of viral nucleic acid by PCR.
Detection of viral Antigen or of antiviral antibody by ELISA (IgM).
Viral isolation.
Mode of transmission: It is transmitted by the mosquito Aedes aegyptuii, since 1700 th till 2020 th many cases were reported in different locations in Egypt
Four serotypes are present. Infection by one serotype confers long life immunity to the same serotype but short-term immunity to the other serotypes.
Natural reservoirs: Humans
Clinical picture and severity
The initial picture is the same as classic dengue, but then shock and hemorrhage, especially in GIT and skin.
Hemorrhagic dengue fever :a sever form of dengue that is fatal). , usually affect children and Previously infected with a different serotype.
Classic dengue (Break Bone Fever):
Recovery occurs after few weeks.
Enlarged lymph nodes and maculopapular rash may occur.
Pain soon develops especially in the back, joints, muscles and eyeball.
flu-like symptoms (fever, chills, and malaise).
CAUSES OF VIRAL HEMORRHAGIC FEVERS: VHFs are caused by viruses of four distinct families
Arenaviruses (Lassa virus)
Flaviviruses
Arenavirus (Lassa fever virus)
Complications: Most common complication is deafness in ~1/3 of cases
Disease severity: sever hemorrhagic fever characterized by multiple organ involvement. Lassa virus is associated with high death rates in pregnant women in 3rd trimester and fetuses (~95% fetal mortality rate)
Mode of transmission: by contaminated food or water with animal urine.
Natural reservoirs: small rodent (multimammate rat), which inhabits rural homes and fields
Morphology : enveloped/ RNA.
Members: Dengue virus and Yellow fever virus
Morphology : enveloped/ Icosahedral/ (+) ss- RNA viruses.
Filoviruses (Marburg, and Ebola viruses)
Clinical presentation:
Treatment:and prevention: treatment is symptomatic and there is no available vaccine
Internal and external bleeding follows leading to shock and death.
This is followed by abdominal pain, vomiting, diarrhea, skin rash.
starts by fever, headache, sore throat and muscle pain.
Mode of transmission: Infections by contacts (direct contact with blood or body fluids) of a reservoir or patient
Natural reservoirs: Monkeys or Bats are the reservoir and humans become infected accidentally.
Disease severity: They are highly virulent viruses with infections usually ending in death (These viruses have the higher mortality rate among all viral hemorrhagic fevers).
Members: Marburg and Ebola
Morphology: enveloped/ Thread – like filamentous /non segmented negative sense ss-RNA.
Bunyaviruses
Rift Valley Fever
Prophylaxis
vector control.
Veterinary examination for imported sheep & cattles
Protective clothing is indicated for persons that have contact with animals to reduce the risk of exposure
A live attenuated vaccine is used for animal (not human) immunization.
sometimes the condition is complicated by:
Hemorrhagic fever.
Meningoencephalitis
Ocular complication (blindness)
Recovery is usually complete
Flu-like symptoms.
The incubation period is 2 to 6 days.
Mode of transmission to humans either by:
Bite of Aedes aegypti mosquito.
Contact with blood, fluids or organs of infected animals e.g., placenta of aborted animal (veterinarians/slaughterhouses workers are at high risk of infection).
Natural reservoirs: The disease affects primarily domestic livestock e.g., sheep and cattle.
Hantaviruses
Disease: Korean hemorrhagic fever (hemorrhagic fever with renal disease and cardiopulmonary syndrome )
Mode of transmission
There is no person to person transmission
(rodent-borne viruses) . It is transmitted by inhaled rodent urine/feces.
Natural reservoirs: rodent
Morphology : enveloped/ helical /non segmented negative sense ss-RNA.
MODE OF TRANSMISSION
contact
With animal blood and body fluids : rift valleys fever
With human blood and body fluids: Marburg/ Ebola
rodent born (robovirus): viruses that are transmitted directly from rodents to humans without an arthropod vector (by exposure to infected rodents or their excreta) e.g. Lassa virus and hantaviruses.
Arthropods born (Arbovirus): viruses that are transmitted from reservoir to humans or from human to human by an arthropod vector e.g. mosquitos transmit yellow & dengue fevers
N.B. there is only one bacterial cause for hemorrhagic fever: Leptospira icterohaemorrhagiae causing Leptospirosis (Weil's disease)
SEVERITY: Some infections of hemorrhagic fever viruses can cause relatively mild illnesses. While in others severe, life-threatening disease may occur e.g., Lassa fever virus (in Africa) and hantavirus infection (in Asia)..
A group of illnesses that are caused by several distinct families of viruses, Characterized by multisystem affection, overall vascular system damage and hemorrhage
Drug therapy of Hypertension
Drug therapy
Classification of antihypertensive drugs:
Vasodilators (DVDs).
Mixed dilators (Na+ nitroprusside):
Na Nitroprusside
Therapeutic uses of Nitroprusside:
Acute aortic dissecting aneurysm (with β-blockers).
Controlled hypotension during plastic & neurosurgery.
Emergency heart failure (acute left ventricular failure & pulmonary edema).
Emergency hypertension e.g. hypertensive encephalopathy.
Teratogenicity
In renal impairment accumulation of thiocyanate → delirium & psychosis.
Prolonged use especially in old age → accumulation of cyanide → acidosis & arrhythmia (avoided by adding Na+ thiosulfate).
Sudden stop → rebound hypertension.
Large dose → severe hypotension & shock.
COP is maintained due to ↓↓ TPR (it may ↑↑ in patients with HF).
Venodilator → ↓↓ VR → ↓↓ EDV → ↓↓ preload → ↓↓ BP.
Artiodilator → ↓↓ TPR → ↓↓ afterload → ↓↓ BP.
Mixed balanced (arteriolar = venular) VD.
↓↓ Platelet aggregation
Nitroprusside → RBCs & endothelium → nitric oxide → ↑↑ activity of guanylate cyclase → ↑↑ cGMP:
very powerful mixed vasodilator
By rhodanase enzyme, cyanide → thiocyanate to be excreted in urine.
Nitroprusside → RBCs & endothelium → nitric oxide + cyanide.
Used by IV Infusion. Onset: 1/2 min. Peak: 2 min. Duration: 3 min.
restricted to the use as IV infusion in some cases of hypertensive emergency.
Arterio-dilators (hydralazine):
Hydralazine
Therapeutic uses: Because of the above-mentioned adverse effects, hydralazine is restricted to IV or IM administration as the first drug of choice for management of hypertensive emergency associated with preeclampsia.
Peripheral neuritis (especially in slow acetylators): Treat by Vit B6.
Hypersensitivity reactions:
Skin rash & drug’s fever.
Reversible rheumatoid arthritis & lupus-like syndrome.
Orally → GIT upsets.
VD → headache, congestion & flush.
Hypotension → reflex sympathetic stimulation:
↑↑ Renin → edema (add diuretics).
Tachycardia → contraindicated in angina (add β-blockers).
Undergoes acetylation in liver (slow acetylators are more prone to adverse effects).
↓↓ BP (DBP > SBP), ↓↓ afterload & ↑↑ stroke volume & ↑↑ COP in HF.
Direct arteriolar dilator.
restricted to IV or IM administration as the first drug of choice for management of hypertensive emergency associated with preeclampsia.
Veno-dilators (nitrites & nitrates):
The role of this group in hypertension is restricted to the use of nitroglycerine IV infusion in some cases of hypertensive emergency.
Angiotensin-aldosterone system (RAAS) inhibitors:
Renin inhibitors:.
Renin antagonists: Enalkiren & Remikiren.
drugs which inhibit renin enzyme as aliskiren
Drugs ↓↓ release of renin: β-blockers and α2 agonists.
Angiotensin II (AT1) Receptor Blockers (ARBs)
Side Effects: Similar to ACEIs, BUT no dry cough.
Therapeutic uses: Similar to ACEIs.
Mechanism of action: they compete with angiotensin II for AT1-receptors leading to:
VD of renal vessels → ↓↓ intra-glomerular pressure (efferent renal VD).
Prevent hypertrophy & remodeling of the heart & blood vessels occurring with hypertension.
↓↓ Sympathetic outflow: block of presynaptic AT1-receptors on adrenergic neurons → ↓↓ noradrenaline release.
↓↓ Synthesis and release of aldosterone.
Mixed VD (They also release prostacyclin).
Losartan, valsartan, candesartan, telmisartan & irbesartan
Angiotensin converting enzyme inhibitors (ACEIs).
Classification of ACEIs:
Prodrugs (by metabolism → active metabolites):
Ramipril → ramiprilat.
Benazepril → benazeprilat.
Perindopril → perindoprilat.
Enalapril → enalaprilat.
Active compounds: captopril, lisinopril.
Drug interactions of ACEIs:
NASIDs inhibit the antihypertensive effect by inhibiting synthesis of PGs.
K+-retaining diuretics e.g. spironolactone augments the hyperkalemic effect.
Na+-depleting diuretics accentuates the initial hypotensive effect.
Contraindicated in 2nd - 3rd trimester of pregnancy → fetal hypotension, renal failure, oligohydramnios → malformation (teratogenicity) or death.
Side effects of ACEIs:
Allergic manifestations →may→ angioedema.
Altered taste (dysgeusia).
Neutropenia: frequent blood count is required.
Proteinuria: frequent urine analysis is required.
Contraindicated in bilateral renal artery stenosis → acute renal failure.
Hyperkalemia, especially if accompanied with K+-retaining diuretics e.g. spironolactone, beta blockers or NSAIDs.
Dry irritant Cough: due to ↑ bradykinin & ↑ PGs (Treatment: shift to ARBs).
First dose hypotension
Therapeutic uses of ACEIs:
Heart failure:
In acute myocardial infarction to decrease the infarct size & inhibit cardiac remodeling.
Mechanism in HF:
↓↓ Secondary hyperaldosteronism → natriuretic → ↓↓ edema.
↓↓ Both after- & pre-load → improve cardiac performance → ↑↑COP.
Hypertension, especially in:
Diabetic nephropathy (very important).
Captopril is the only member used in treatment of hypertensive urgency
High renin.
Advantages
No abnormality in glucose, lipid, cholesterol or uric acid metabolism (better than diuretics).
No reflex tachycardia (↓↓ baroreceptors reflex & ↓↓ sympathetic activity).
Less venodilatation: No postural hypotension
No ↓↓ in COP (it may increase in HF).
Pharmacological actions of ACEIs:
↑↑ Renal blood flow (RBF) (but ↓↓ GFR due to efferent VD → ↓↓ intraglomerular pressure).
COP is maintained or even ↑↑ in case of heart failure.
Venodilatation→ ↓VR → ↓↓ EDV → ↓↓ preload & ↓↓ BP.
Arterial dilatation → ↓↓ TPR → ↓↓ afterload & ↓↓ BP.
Mixed VD (arterial > venous).
Reflex ↑↑ renin & ↑↑ angiotensin I.
Mechanism of Action: inhibit angiotensin converting enzyme:
↓↓ Inactivation of bradykinin → ↑↑ bradykinin → VD (directly & by ↑ PGs & ↑NO).
↓↓ synthesis of angiotensin II:
Inhibit hypertrophy & remodeling of the heart & blood vessels.
VD, ↓↓ aldosterone & ↓↓ sympathetic activity.
Calcium channel blockers (CCBs).
After one year, verapamil should be substituted by a 1st line antihypertensive drug.
its use in hypertension is limited by its hepatotoxicity when used for more than one year.
The control of hypertension in this year also could be achieved by verapamil alone or addition of another drug
The use of slow-release tablets could cure headache.
Thus, verapamil is restricted to hypertension associated with migraine or cluster headache.
Amlodipine
is the most commonly used DHP Dihydropyridine اسم لاحد العائلات الدوائية, in both hypertension and angina pectoris
This is because
Amlodipine produces both peripheral arterial vasodilation and coronary dilation, with less reflex tachycardia; possibly because of the long t1/2 it produces minimal peaks and troughs in plasma concentrations.
not expensive
its renal elimination is only 10% (could be used in renal impairment)
its "t1/2" is 39 hours
(given 5-10 mg once daily)
it has 74% oral bioavailability
Use of diuretics in hypertension:
Potassium-retaining diuretics:
Spironolactone & eplerenone in cases of hyperaldosteronism.
In combination with other diuretics to correct hypokalemia.
Thiazides: In Mild and moderate hypertension, as monotherapy or in combinations.
Mechanism of antihypertensive action of diuretics:
Indapamide: A thiazide analogue when used in a small dose it has a vasodilator activity (Ca2+-channel blocking effect), with some diuretic effect.
Thiazide diuretics in addition have a direct vasodilator action by:
Release of vasodilator PGs.
Activates ATP-dependent K+ channels → hyperpolarization → VD.
Deplete Na+ from the arterial wall.
Diuretic action → ↓↓ blood volume → ↓↓ cardiac output → ↓↓ blood pressure.
Diuretics used in treatment of hypertension are:
Potassium-sparing diuretics:
spironolactone (the only approved member because it has cardio-protective effect).
Loop diuretics:
torsemide (used only when diuretics are needed in hypertensive patients associated with renal impairment).
bumetanide
frusemide
Thiazide diuretics & their analogues:
indapamide
clorthalidone
hydrochiorothiazide (the most commonly used agent)
Sympatholytic drugs = Sympathetic depressants.
Adrenergic receptor blockers:
α-adrenoceptor blockers (prazosin & doxazosin)
β-adrenoceptor blockers (bisoprolol & atenolol)
Adrenergic neuron blockers: reserpine & guanethidine (not used).
Centrally-acting sympathetic depressants:
Imidazoline receptor agonists (rilmendine).
α2 agonists (α-methyldopa & clonidine).
First line groups of drugs used in treatment of essential hypertension:
For mono-, double or triple therapy:
D. Diuretics (thiazide).
C. Ca2+-channel blockers.
B. β. Blockers.**
** β-adrenoceptor blockers were considered previously to be in (B). Recently, worldwide studies demonstrated 50% increase in the incidence of developing type-2 diabetes. As a result, their use in hypertension is restricted to نستخدمه فقط معthe presence of other associated disease (angina, arrhythmia or thyrotoxicosis).
A. Angiotensin-converting enzyme inhibitors (ACEIs).*
* If the patient could not tolerate ACEIs, it is substituted by angiotensin-receptor blockers (ARBs).
Stages of Hypertension: hypertension is classified according to systolic and diastolic blood pressure into the following 3 stages:
Hypertensive Emergency: blood pressure 220/140 mmHg associated with target organ damage as hypertensive encephalopathy, heart failure and renal failure.
Hypertensive Urgency: blood pressure > 180/110 mmHg not associated with target organ damage.
Types of Hypertension:
Secondary hypertension is caused by underlying disease e.g. renal, SLE, Cushing syndrome, thyrotoxicosis, pregnancy, etc.
Essential (primary) hypertension: Of unknown cause.
Defined as persistent elevation of blood pressure above 140/90 mmHg in at least three measurements on at least three separate occasions.
Anti-arrhythmic Drugs
Classification of anti-arrhythmic drugs
Miscellaneous e.g. adenosine, digitalis and magnesium
Used in:
Prevent paradoxical tachycardia induced by quinidine.
In atrial flutter and AF to ↓↓ AV conduction → protect ventricle from high rate of atria.
Magnesium
Some patients with torsades de pointes even if serum magnesium is normal.
Digitalis-induced arrhythmias if hypomagnesaemia is present.
Adenosine
Interactions
Dipyridamole by adenosine uptake inhibition → Potentiation.
Theophylline or caffeine blocks its receptor → antagonism.
flushing, hypotension, chest pain
May cause shortness of breath related to bronchospasm due to activation of adenosine receptors in the lung.
Uses: adenosine is the drug of 1st choice for prompt conversion of PSVT to sinus rhythm because of its high efficacy and very short duration of action [half-life 10 seconds].
Adenosine inhibits AV nodal conduction and increases the AV nodal refractory period but has lesser effects on the SA node.
Stimulates adenosine receptor “Gi-coupled receptor”,
The results of these actions are marked hyperpolarization and suppression of calcium-dependent action potentials.
this produces:
Activation of K+-channels lead to K+ efflux → hyperpolarization.
Inhibition of adenylyl cyclase → ↓↓ cAMP-induced calcium influx.
IV: Ca2+ channel blockers Slow conduction in calcium dependent regions [SA and AV nodes]
Verapamil
Drug interactions:
Co administration of verapamil with antihypertensive drugs may produce marked hypotension.
Combination of verapamil with β-adrenoceptor blockers may cause heart block, heart failure.
Contraindications: Heart failure, heart block and sick sinus syndrome.
Extracardiac: minor adverse effects include headache, flushing, constipation, lassitude, nervousness, and peripheral edema.
Cardiac: The side effects of verapamil are dose-related and usually avoidable, this includes:
In patients with sinus node disease, verapamil can precipitate sinus arrest.
Verapamil can lead to atrioventricular block when used in large doses or in patients with partial AV block. This could be treated with atropine, βadrenoceptor stimulants, or calcium.
Negative inotropic effect, which may precipitate heart failure in susceptible patients.
Therapeutic uses:
Verapamil can also reduce the ventricular rate in atrial fibrillation and flutter. It may convert atrial flutter and fibrillation to sinus rhythm.
It is not used from the start because if ventricular tachycardia is misdiagnosed as PSVT it will be converted to VF by verapamil.
"PSVT": verapamil is used to inhibit recurrence of PSVT after conversion to sinus rhythm by adenosine unless there is a contraindication to the drug.
Much smaller doses are required when the drug is administered intravenously.
Its t1/2 is approximately 7 hours. Therefore, verapamil must be administered with great caution in patients with hepatic dysfunction.
It is extensively metabolized by the liver with only 20% bioavailability.
It is well-absorbed from the GIT.
Extracardiac effects: ▪ Vasodilatation (includes systemic and coronary blood vessels).
Cardiac effects:
Verapamil decreases the impulse conduction in the AV-node, thereby, decreases the response of the ventricles to supraventricular arrhythmia.
It decreases sinus arrhythmias and stops AV-nodal or junctional arrhythmia (paroxysmal supraventricular tachycardia “PSVT”).
Verapamil blocks Ca+2-channels. Thus, its effect is more marked on tissues that that their activation depends on Ca+2, such as the SAN and AVN and the junctional tissues.
III: K+ channel blockers Prolong APD and RP
The most important adverse effect of sotalol, dofetilide and ibutilide is excessive QT interval prolongation and Torsades de pointes.
Ibutilide: like dofetilide but administered intravenously.
Dofetilide
Used orally for treatment of AF.
Blocks K+ channels→ ↑APD& RP.
Sotalol
Supraventricular & ventricular arrhythmias in children.
AF
Blocks β-receptors.
Blocks K+-channels → ↑↑ APD action potential duration & RP refractory period.
Dronedarone
Used in Atrial F.
No thyroid or pulmonary toxicity.
The half-life: 24hrs
Structural analog of amiodarone and lacks iodine atoms so no effect on thyroxin metabolism.
Amiodarone
Hypotension
Hepatitis: Abnormal liver function tests should be monitored regularly.
Pulmonary interstitial fibrosis: Dose-related toxicity& fatal in 1% of patients.
Thyroid dysfunction, hypo- or hyperthyroidism as it contains iodine.
Corneal microdeposits.
Photosensitivity and grayish blue discoloration of the skin.
Amiodarone is broad spectrum (Atrial fibrillation, atrial flutter; ventricular tachycardia) anti-arrhythmic drug. However, it is not the first drug of choice due to its multiple adverse effects.
Mild β-blocking effect.
Blocks Ca2+channels.
Blocks Na+ channels.
Prolongs the APD & RP by blocking K+-channels.
The half-life is long up to several weeks.
It undergoes hepatic metabolism to active metabolite.
Oral bioavailability of 35–65%.
II: β-blockers Blockade of sympathetic effects in the heart
Propranolol can exacerbate vasospasm in vasospastic angina.
Metoprolol can cause dyslipidemia.
May mask the signs of hypoglycemia
CNS effects (sedation, sleep alterations).
Cardiovascular effects (bradycardia, AV block, HF).
Impotence, exacerbation of COPD and asthma.
Esmolol
is a short-acting β-blocker used for intra-operative and other acute arrhythmias.
Propranolol
inhibits conversion T4 to T3 so control dysrhythmia of thyrotoxicosis. Propranolol and similar drugs have β-receptor-blocking action and direct membrane stabilizing effects.
Non-selective β-blockers inhibit hypokalemia induced by excessive circulating adrenaline. Thus, they can control arrhythmias caused by:
Myocardial infarction.
Exercise or stress.
Pheochromocytoma
AV node particularly sensitive→↑PR interval.
The major anti-arrhythmic effects of these drugs are due to blocking of βadrenoceptors in the heart → ↓↓ cAMP → ↓↓ all cardiac properties; automaticity, excitability& conduction.
I: Na+ channel blockers Reduce Na+ current → slow depolarization
IC Dissociate from the channel with slow kinetics with minimal effect on APD
Class IC [Flecainide and Propafenone]
Class IC is contraindicated in structural and ischemic heart disease.
Proarrhythmic, especially post-MI
Exacerbation of preexisting ventricular arrhythmias
Heart block, heart failure and bronchospasm.
Uses: Supraventricular arrhythmias including atrial fibrillation.
Propafenone has calcium channel & β-blocking-activity.
Not affect K+ channels → not affect APD.
Delay AV conduction → prolong PR interval.
Marked Na+ channel block → ↓ excitability and conduction.
IB Dissociate from the channel with rapid kinetics and shorten APD
Class IB [Lidocaine, Phenytoin and Mexiletine]
Members
Mexiletine
like lidocaine but can be given orally.
Phenytoin
Used in ventricular arrhythmia after myocardial infarction and digitalis toxicity.
Antiepileptic and antiarrhythmic drug that can be administered IV route and orally.
Lidocaine
Not used orally due to extensive first pass metabolism by the liver with formation toxic metabolites → convulsions.
Used by intravenous infusion mainly in ventricular arrhythmia after myocardial infarction or cardiac surgery.
They have the following actions:
No block to other channels or autonomic receptors.
Rapid dissociation from Na channel.
Shorten APD.
IA Dissociate from the channel with intermediate kinetics and prolong APD
Disopyramide
Used mainly for supraventricular arrhythmia.
May precipitate heart failure
Differs from quinidine in: Marked atropine-like action → dry mouth & blurring of vision and contraindicated in senile enlargement of prostate and glaucoma.
Procainamide
Used mainly for ventricular arrhythmia.
Differs from quinidine in:
Metabolized by acetylation: in slow acetylators → systemic lupus-like syndrome.
Weak atropine like action & No α-blocking effect.
Quinidine
Adverse effects:
Idiosyncratic: Hepatitis, thrombocytopenia and angioneurotic edema
Cinchonism: Headache, tinnitus, vertigo and blurring of vision → only in toxicity.
Allergy: give test dose.
GIT: Diarrhea, nausea and vomiting→ Common.
CVS
Embolism with old AF.
Long QT interval [due to K+ channel block] → Torsades de pointes.
Paradoxical tachycardia in AF.
Pharmacological actions:
Other actions: antipyreticخافض لحرارة, muscle relaxant, oxytocic and antimalarial.
Hypotension: due to vasodilating and α-blocking effects.
Moderate atropine-like action → Paradoxical tachycardia
K+ channel block → ↑↑APD and RP.
Na+ channel block → ↓↓ excitability and conduction.
Excreted in urine and acidification of urine enhance its excretion.
Partially metabolized in the liver.
Bind to plasma proteins.
Absorbed orally and parenterally.
Why we treat arrhythmia? Because it can reduce the cardiac output.
Arrhythmia = Abnormal heart rate and/or rhythm.
Infective
Others: TB, Syphilis, Fungal.
Prognosis: Without treatment, the disease is fatal in few months to years due to heart failure, renal failure or embolic complications.
Diagnosis: Confirmed by blood culture.
Toxemia: Degeneration in parenchymatous organs, clubbing of fingers and bone marrow depression.
Clubbing
Osler nodules: Raised red lesions in the finger tips due to capillary damage and perivascular infiltration.
Focal embolic glomerulonephritis with hemorrhagic spots on the surface of the kidney (flea-bitten kidney).
Embolic manifestations with infarctions in various organs as spleen, brain and kidney.
Healing by granulation tissue and fibrosis.
The valves are infiltrated by lymphocytes, macrophages, PNL's.
The vegetations are formed of fibrin, platelets, bacterial colonies and few neutrophils.
The vegetations cover the valve cusps and spread on mural endocardium.
The site of vegetations depends on the site of the predisposing valvular lesion.
The vegetations are large, polypoidal and friable.
The affected predisposed valve has low vitality and rough surface. This favors bacterial deposition and multiplication.
Infection by streptococcus viridans usually results from septic dental focus or throat infection.
5- States of immunosuppression
4- Intravenous drug abusers.
3- Prostheticصناعية valves, catheters
2- Chronic rheumatic valvulitis.
1- Congenital heart disease.
Causative agents:
Fungal in immunosuppressed patients.
Streptococcus viridans and influenza bacilli.
Acute bacterial endocarditis.
Prognosis: Even with treatment the disease is usually fatal within few days to weeks due to valve perforation and heart failure (malignant course).
Toxic manifestations (toxemia and septicemia)
Spread of infection to aorta or heart wall with abscess formation
Detached vegetations lead to circulation of septic emboli (empyema) with subsequent formation of pyemic abscesses.
Microscopic picture: Vegetations contain fibrin, platelets, bacteria and neutrophils
Gross picture: Bulky, polypoid, detachable, septic vegetations on the cusps. These vegetations spread on mural endocardium and chordae tendinea
States of immune deficiency.
Causative agents: - Hemolytic streptococci - Staphylococci - Gonococci
Definition: Acute suppurative inflammation of healthy cardiac valves caused by highly virulent pyogenic organisms.
VENOUS CIRCULATION
Effects of gravity on the venous system:
Mechanisms that aid the venous return in standing position against gravity:
N.B. :In prolonged standing without movements a condition called "varicose veins",is resulted as the valves of the veins of the lower limbs become incompetent. The blood flow toward the heart is decreased. The veins of the lower limbs dilate and become filled with blood. The pressure in the veins rises, capillary pressure is increased and, ankle edema is produced.
N.B.: Muller’s maneuver: opposite to occur in Valsalva as it starts by deep inspiration with closed glottis.
Valsalva maneuver:
Forced expiration against a closed glottis (as in delivery and lifting heavy objects) increase intrathoracic pressure to about +40 mmHg, if continue to 10 seconds
At the end of this maneuver deep inspiration occurs
The increase in aortic pressure compensatory baroreceptor reflexes (Mary’s low) decrease bl. pressure towards normal.
The –ve intrathoracic pr. -->increase VR increase Co increase Aorta P.
Suction of the lung vessels increase bl. return to left sides of the heart decrease Co decrease aortic pressure.
The decrease in aortic pr. compensatory baroreceptor reflexes -> vaso- & veno-constriction increase aortic pressure towards normal.
The +ve intrathoracic pr. decrease VR decrease COP decrease aortic pressure.
Squeezing of lung vessels increase bl. return to left atrium & ventricle increase Co increase aortic pressure.
Cardiac suction:
Ventricular suction during rapid filling phase expansion of the ventricle decrease intra ventricular pressure suction of the blood from atria --> increase VR.
Atrial suction: during rapid ejection phase, the A-V valve moves downward expansion of atria --> decrease intra-atrial pressure -->increase VR.
Thoracic pump:
Expiration causes the reverse.
Inspiration causes increase -ve intrathoracic and +ve intra abdominal pressure increase VR
Muscle pump:
During relaxation, the valves close and prevent backflow of the blood to lower limbs.
During skeletal muscle contraction squeezing the veins increase VR.
Venomotor tone:
There is sympathetic venomotor tone to prevent stagnation of bl. in lower limb veins.
Hydrostatic indifferent point (HIP):
Hypervolemia, VC & capacitance of lower limbs (during swimming) shift HIP upwards to level of right atrium constant CVP constant VR, CO and ABP inspite of change the position during swimming. So, orthostatic hypotension doesn’t occur during swimming.
Hypovolemia, VD and increase the capacitance of lower limbs veins as in varicosity shift (HIP) down.
The pressure at which 10-11 mmHg.
It is a transitional zone (5-7 cm below the diaphragm) in which the venous pressure remains constant and independent of body posture.
Venous pressure gradient:
The pressure in superior sagittal sinus is –10 mmHg thus if the sinus is opened during neurosurgical operation it sucks air air embolism.
Above the right atrium the venous pressure becomes subatmospheric, however thoracic veins don’t collapse because it is surrounded by the negative intrathoracic pressure. In neck veins, they are partially collapsed by the atmospheric pressure.
In prolonged standing, the high pressure in lower limbs varicose veins & odema.
The change in position from recumbent to standing position associated with some difference in venous pressure.
Orthostatic hypotension:
When the person changes his position from the lying to the erect position bl. shifts to lower limb --> decrease VR -->decreaseCVP --decraese Co --> hypotension --> dizzy sensation, diminish vision even fainting may occur (but compensatory mechanisms correct the hypotension).
Venous pressures
Peripheral venous pressure:
The increase in CVP will lead to opening of these compressions before elevation of the peripheral venous pressure.
It is about 4 to 7 mmHg greater than the CVP this occurs because there are many points at which resistance to bl. flow present as:
Collapsed neck veins by the atmospheric pr.
Angulation of arm veins on the 1st rib.
Intraabdominal pressure on abdominal veins.
Central venous pressure:
It’s functions are:
It is the force which fills the ventricle.
It is the determining force of venous return as the transmural pressure (the filling pressure for the heart) = CVP – intrathoracic pressure.
It is regulated by a balance between the venous return and the cardiac output.
It is increased by:
But the lower limit is –3 to –5 mmHg.
Decreased VR as in decreased blood volume in severe haemorrhage.
It is decreased by:
It may reach 20-30 mmHg
Decrease COP as in congestive heart failure.
Increased venous return as in increase blood volume, venoconstriction and vasodilatation.
It is normally from zero - 4 mmHg.
It is the pressure in right atrium and large veins opening into it.
Functions of the veins :
They are capable of actually propelling blood by means of a so-called "venous pump".
They are capable even of regulation of C.O.P.
They are capable of constricting and enlarging.
Storage of the blood (capacitance vessels): They accommodate about 65% of the circulating blood. This allow the venous circulation to act as blood reservoir and to hold the major portion of the blood volume at low pressure.
Drainage of blood from all tissues to the heart.
Veins are the blood vessels in which the blood flow is directed towards the heart.
Cardiac cycle
during cardiac cycle:
Fourth
In Atrialsystole
Third
In Maximum(rapid ) filling
Second
In Isometric relaxation
First
I n Maximumejection
In Isometriccontraction
ECG changes during cardiac cycle:
T wave: ventricular systole ends just after top of T wave. Heart Sounds
QRS complex: start before ventricular systole by 0.02 sec.
P wave: starts before atrial systole by 0.02 sec.
Importance of cardiac diastole:
Time of ventricular rest (to prevent Fatigue).
Time of main coronary blood Flow.
Time of ventricular Filling (mainly in early diastole).
Ventricular cycle
Ventricular diastole 0.5 sec
Reduced filling phase:
Ventricular pressure Rises the to 4 stroke mmHg.
Events 10% of the stroke volume flow slowly to the ventricle
Duration. - 0.2 sec.
Maximal (rapid) filling phase:
Duration. - 0.1 sec.
Heart sounds - The third heart sound due to rushing of blood into theventricles and vibration of the ventricular wall.
Ventricular volume - Increased.
Ventricular pressure - Around zero. - Aortic pressure decreases due to escape of bloodto peripheral vessels.
Atrial pressure - Around zero.
Events - It begins by opening of A.V. valve due to the increased atrial pressure above the ventricular pressure (60% of stroke volume is rushed to the ventricle).
Isometric relaxation phase:
ECG - end of T wave.
Valves - -The semilunar valves (aortic, pulmonary) close at thebeginning of this phase - -The A.V. valves open at the end of this phase.
Heart sounds - The second heart sound due to closure of the aortic valveand pulmonary valve (semilunar valves).
Ventricularpressure - Falls rapidly from 90 to 0 mmHg. - Aortic pressure: due to elastic recoil of the aorta itspressure increased leading to upward (dicrotic) wave.
Atrial pressure - Increased above the ventricular pressure due to accumulation of venous return, this pressure can open the - A.V. valve at the end of this phase.
Events - It begins by closure of the aortic valve and the ventricles relax isometrically without change in the ventricular volume.
Duration. - 0.06 sec
Protodiastolic phase:
ECG - down slope of the (T) wave
Valves - The closure of semilunar valves occurs as a result of fall of ventricular pressure below that of aortic and pulmonary arteries. The closure of the aortic valve and the change of potential energy to kinetic energy leads to sharp momentary fall in the aortic pressure called the dicrotic (incisura) notch.
Ventricular volume - Constant.
Ventricularpressure - The ventricle begins to relax but still contracted and its pressure decreases about 20 mmHg and the aortic pressuredecreases also (due to escape of blood to peripheral circulation). But still above ventricular pressure. This causesthe blood in the aorta to regurgitate to the ventricles leading - to closure of the aortic valve at the end of this phase.
Events - The period between the end of ventricular systole and theclosure of the aortic valve.
Duration. - 0.04 sec
Ventricular systole 0.3 sec
Reduced (minimum) ejection phase:
Ventricular volume - Decreases to reach the end systolic volume (ESV = 70ml).
Ventricular pressure - The ventricular and aortic pressures: reach their maximum and begin to decrease (due to escape of blood to peripheral circulation is more than the amount of blood ejected from the ventricle.
Atrial pressure - Increased due to venous return.
Events - The remaining 30% of stroke volume is ejected to the aorta.
Duration. - 0.1 Sec
Rapid (maximum) ejection phase:
ECG - Beginning of T wave of ECG (repolarization of the ventricles).
Valves - The semilunar valves are opened. - The A.V. valve is closed
Heart sounds - The second component of the first heart sound due to rushing ofblood into the aorta and vibration of the aortic wall.
Ventricularvolume - decreases greatly due to change of the isometric contraction to isotonic contraction and ejection of the blood ( blood is notcompressible).
Ventricularpressure - The ventricular and aortic pressures rise from 80 to120 mmHg. - Because the amount of blood ejected through the
Atrial pressure - Decreases due to down of the A.V. valve during displacement shortening of ventricular muscles.
Events - It begins by opening of the aortic valve and rushing of blood intothe aorta where 70% of stroke volume ejected in this phase.
Duration. - 0.15 sec
Isometric (iso-volumetric) contraction phase:
ECG - QRS complex starts before the ventricular contraction by 0.02 seconds to ventricular depolarization
Valves - are closed (A-V and semilunar valves)
Heart sounds - the first components of the first heart sound due to closure of the A.V. valves
V. volume - Constant (isometric), because blood is not compressible.
V. pressure - Rise from 4 mmHg to 80 mmHg in the left ventricle.
Atrial pressure - Rise due to bulging of the A.V. valves into the atria and also due to regurgitation of some blood into the atria before closure of the A.V. valves.
Events - It begins by closure of A.V. valve and the ventricles begin to contract isometrically (without change in muscle fiber length). - Thus the ventricles are closed chambers filled with blood
Duration. - 0.05 sec
Duration
Atrial cycle
Atrial diastole 0.7 sec
Atrial systole 0.1 sec.
Atrial contraction phase (late diastole):
ECG - P wave of ECG starts before atrial contraction by 0.02 sec due - to the atrial depolarization.
Valves - -The semilunar valves are closed. - -The A.V. valve is opened
Heart sounds - 4th heart sound (weak and inaudible), due to vibration of atrial - muscle during contraction and blood rushing to ventricles.
Ventricular volume - Increased by 20 ml to reach end diastolic volume (140ml).
Ventricular pressure - Rise from 4 mmHg to 8 mmHg and return to 4 mmHg at end of - this phase as the ventricles dilate to accommodate blood passingto it.
Atrial pressure Rise from 4 mmHg to 8 mmHg and return to 4 mmHg at end of - this phase due to the atrial evacuation.
Events - Atria contract and pump 30% of the ventricular filling intoventricles.
Duration. 0.1 Sec
When heart rate increases, the cycle shortens, especially the diastole.
Complete cardiac cycle = 0.8 sec., if the heart rate is 75 beats/minute
Electrical events: The cycle is initiated by SAN, and then the action potential travels rapidly through both atria then reach AVN with a delayed period of 1/10 seconds (to allow both atria to contract before ventricular contraction), then through the AV bundle into the ventricles.
It starts by systole of both atria followed by systole of both ventricles and then diastole of the whole heart.
It is the period from the end of one heart contraction to the end of the next (=Events that occur in the heart during one beat).
Capillary Hemodynamics
General features of capillary circulation:
Safety factors against edema:
Total safety factors against edema is 17mmHg i.e. 5+7+5.
This means that capillary hydrostatic pressure must rise about 17mmHg or the capillary oncotic pressure decreases about 17 mmHg before edema begins to appear.
Washout of protein from the interstitial spaces: increased lymph flow also washes out most of the proteins from the tissue spaces decreasing the colloid osmotic pressure of the interstitial fluid. It gives 5 mmHg safety factor.
Flow of lymph from the tissues: when interstitial free fluid pressure rises above the normal value, the lymph flow increases markedly removing the greater portion of the extra fluid. It gives 7 mmHg safety factor.
Normal negative interstitial hydrostatic pressure: the interstitial free fluid pressure must rise from the normal value negative pressure to above 0 mmHg, before edema begins to appear. It gives 5 mmHg safety factor.
Factors determine transcapillary exchange and interstitial fluid formation (Starling forces):
Types of Starling forces: (4= 3+1)
Anti-filtering force (1): opposes movement of fluid out from the capillary.
At the venular end, the capillaries are more permeable (more branched, with more wide pores). So, most of filtration is reabsorbed and small amount removed from the interstitial fluid by the lymph vessels.
At arteriolar end, net filtration occurs by 13 mmHg, while, at venular end, net reabsorption force occurs by 7 mmHg.
Donnan effect it attracts Na+ and fluid to inside the cells. It is about 28 mmHg and exerted mainly by albumin.
Plasma proteins colloid osmotic (capillary oncotic) pressure: as the plasma proteins with high molecular weight do not penetrate the capillary membrane and by
Filtering forces (3): move fluid out from the capillary.
Interstitial fluid colloid osmotic (oncotic) pressure: some of plasma proteins leak into the tissue spaces and absorb fluids to outside the capillary. It is about 8 mmHg.
In the liver and spleen, interstitial hydrostatic pressure is positive.
Capillary hydrostatic pressure:
At venular end = 10-15 mmHg
At arteriolar end = 30-40 mmHg
Definition of starling forces: they include forces (factors) that determine filtration and interstitial fluid formation (trans-capillary exchange).
Active and inactive capillaries:
In resting tissues (alternation phenomenon):
In active tissues: the vasodilator metabolites formed in these tissues causes dilatation of precapillary sphincters which causes blood flow through the closed capillaries.
Only 10% of the capillaries are opened while, 90% of them are completely closed. After few seconds, the opened capillaries become closed spontaneously while a similar number of the previously closed capillaries are opened.
Mechanism: gradual decrease in O2 and increase in both CO2 and H+ around the closed capillaries succeed to open them. Then, blood flow in this area provides O2 and removes waste products (CO2 and H+) abolishing their vasodilator effect which causes the capillaries to be closed again.
Microcirculation unit:
On contraction of those sphincters, blood rapidly passed through the thoroughfare vessel to the venules, while when they are relaxed, blood passes out into the true capillaries
The precapillary sphincters have a rich sympathetic innervation causing continuous contraction (tone). The sympathetic tone may be increased or decreased reflexly.
The true capillaries open from the proximal end of thoroughfare vessel. The entrances of these capillaries are controlled by rings of smooth muscle (pre-capillary sphincters).
The blood does not flow directly from arterioles into venules, but rather into a thoroughfare vessel which connects the arterioles to the venules. This vessel, like arteriole and venule, has sparse smooth muscle layer mainly located at the arteriolar end.
Function of capillaries: site of gas, nutrient and waste product exchange i.e. O2 and nutrients enter the interstitial fluid while, CO2 and waste products enter the blood stream.
At any moment, only 5% of the circulating blood is in the capillaries (about 10 billion capillaries with a surface area of 500-700 m2).
Mcq
Lipoproteins
mcq
LYMPHATIC VASCULAR SYSTEM
● It's composed of:
Lymphatic Duct
Lymph is collected in the thoracic duct before entering the blood stream. It
is composed of:
Tunica adventitia is poorly developed.
Tunica media: thick mixed longitudinal and circular smooth muscle.
Tunica intima: endothelium, C.T. and elastic lamina.
Lymphatic Vessels:
its wall layers
Tunica adventitia: thick and consist of C.T., collagen and elastic
fibers.
Tunica media: thin circular smooth muscle fibers with some elastic
fibers.
Tunica intima: contain endothelial cells. Possesses valve to allow
unidirectional flow of lymph
o Lymph consists of blood proteins, antibodies, lymphocytes and fat
droplets which give milky color of the lymph.
Lymph enter lymphoid organ to be filtered where new lymphocytes are
added.
Lymph passes to larger vessels with very thin wall of endothelium, basal
lamina, collagen fibers and many valves.
Lymphatic Capillaries:
Lymphatic capillaries are absent in C.N.S, bone marrow and eye.
Anchoring filament extend between incomplete basal lamina and
perivascular collagen to maintain patency of the vessels during time of
increase tissue pressure.
Have one layer of endothelial cells with discontinuous basal lamina to
permit collection of extracellular fluid.
A network of blind- ended anastomosing tubes of 5- 10 µm in diameter.
Consist of vessels that collect lymph (excess fluid) and return back to the blood
stream.
A-V anastomosis
Types:
. Organized connections (glomus body):
Function: regulation of temperature and venous pressure.
It has thick richly- innervated muscle layer and small lumen.
It has connective tissue capsule that is penetrated by an arteriole
with no internal elastic lamina.
It is a small organ present in nail beds, tip of fingers and toes,
and auricle of the ear.
Simple connection: without structural changes in its wall, they are
either straight or tortuous.
Sites: skin, thyroid and digestive tract.
They are characterized by absence of elastic tissue in their walls and presence
of abundant muscle fibers.
They are direct connection between arterioles and venules (Fig. 11.8).
penile arteries
They are characterized by longitudinal ridge like thickening in the lumen
smooth muscle fibers
longitudinal connective tissue
renal arteries
they are modified to prevent sudden increase of pressure in the glomeruli
umbilical arteries
tunica media composed of
outer circular muscle layer
inner longitudinal muscle layer
they have no internal elastic lamina
coronary arteries
they have well developed three elastic laminae
middle
enternal
the sub endothelial Layer contains Longitudinal smooth muscle cells
they supply the heart they have thick wall
basilar arteries
they have
adventitia
tunica media
wide lumen and thin wall with well developed internal elastic lamina
they supply the brain
their wall is composed of
includes a connective tissue
rich in
collagen
Tunica media :
includes
external elastic lamina
few elastic fibers
smooth muscle cells
tunica intema :
thin subendothelial layer of CT
with
thick fenstrated internal elastic lamina
and
endothelium
they are the most numerous type
they are muscular arteries distributing blood to different organs of the body
so they are also called muscular or distributing arteries
written
Blood vessels
general structure of blood vessels except capillaries
innervation
blood supply
In medium and large vessels ,
whereas the outer layers of media and adventitia receive blood from the vasa vasorum
the layers near the lumen receive oxygen and nutrients from blood in their lumen by diffusion
small blood vessels (thin waked) recieve oxygen and nutrients from the blood passing their lumen by diffusion
functional significances
collagen fibers prevent over expantion and limit the shortenning of the vessel if it is cut
elastic fibers allow easy expansion and recoil durring cardiac systole and avoid occlusion during cardiac diastole
endothelium provides smooth surface for the blood flow to avoid clotting
The wall of blood vessels is composed of three main coats
in this layer , carge blood vessels contains vasa vasorum (vessels or the vessels) which is a network of small blood vessels to supply the walls of the major vessels with blood
it is composed of
elastic fibers
collagen fibers
it is the outermost layer
tunica media
it is composed of:
External elastic lamina that separates the media from the adventitia
connective tissue in between muscle fibers
circular smooth muscle fibers
it is the middle layer
tunica interna
It is composed of
internal elastic lamina formed of elastin
supendothelial layer of connective tissue
underlying basement membrane
endothelium(simple squamous epithelium
It is the inner most layer
are
A-V anastomosing
Comparison between medium sized artery and vein
Medium Sized Vein
Have valves
Thick adventitia
Thin media
No internal elastic lamina
Wide lumen
Thin wall
Medium Sized Artery
No valves
Thin adventitia
Thick media
Well developed internal elastic
lamina
Narrow lumen
Thick wall
veins
types of veins
NB. Some veins show exceptional variations in their structure
Umbilical vein is very muscular.
Cerebral, retinal and osseous veins have no valves or T. media.
Large Muscular Veins
Its wall is composed of:
Tunica adventitia
a thick layer of C.T. contains
longitudinal smooth muscle.
lymphatics
nerves,
vasa-vasorum,
Tunica media
a several layers of smooth muscle
and penetrated by
lymphatics
vasa vasorum
separated by collagenous C.T.
but longitudinal
in vena cava
which are often crcular
Tunica intima
and valves
are always present.
contains few elastic fibers
well developed,
They include renal vein, venae cavae, pulmonary vein and femoral vein.
Medium Sized Veins
Its wall is composed of:
Tunica adventitia is the thickest layer and composed of longitudinally
arranged collagen and elastic fibers.
Tunica media consists of 3-5 layers of smooth muscle cells
. Tunica intima
intimal valves are prominent
and are devoid of elastic fibers
contains
subendothelial connective
tissue
endothelial cells
It has a thin wall and wide lumen and more likely to contain blood in
histological sections.
The most common type of veins in the body.
Small Veins
Similar to venules but have a thicker tunica media and adventitia.
Venules
NB. Histamine increase the distance between the endothelial cells of venules to
allow passage of fluids and cells into surrounding connective tissue.
Exchange of tissue fluids occurs in capillaries and post capillary venules
Leukocytes attach and cross the basement membrane to enter the surrounding
connective tissue
Tunica adventitia contains C.T. thicker than tunica media.
Tunica media is absent in small venules but few smooth muscle fibers appear
in larger ones.
Valves may be present to prevent retrograde flow of blood.
They have an endothelial lining with numerous pericytes.
They are small vessels at terminal ends of capillaries (post- capillary venules)
● Valves:
They are present only in
veins of diameter more than 1 mm particularly in extremities to prevent back
flow of blood against gravity.
semilunar projections of tunica intima
and have two leaflets
lined by endothelium,
composed of fibro-elastic
tissue
Begins as venules then increase in size to continue with small medium to
continue with sized vein and finally large veins.
They return un-oxygenated blood from the organs to the heart.
capillaries
types
discontinous capillaries
function:
storage and passage of blood elements and filtration of blood by phagocytosis
The endothelium cells secrete
mitotic agents
vasodilator
vasoconstrictor
permiability for O2 , Co2 and metabolites
sites
red bone marrow
spleen
the basal lamina is incomplete or absent
The walls reveal small distinct gaps between adjacent cells
endothelial cells and phagocytic cells line them
they are large spaces with irregular thin easily collapsed wall
fenestrated capillaries
found in
endocrine glands
GIT
their morphology helps to exchange fluid and macromolecules
have pores (fenestrae) in the endothelial wall , sometimes covered by a diaphram
continous capillaries
They are found in
gonads
nervous tissue
CT
muscle
formed of
they contain pinocytic vesicles that permit transport in both direction
one layer of endothelium forming a tube
there are tight junction between endothelial cells which rest on basal lamina
general characteristics
they have single layer of endothelium on basal Camina and pericytes
endothelium permit exchanges
of
metabolites
fluid .
enzymes
gases
They are low pressure vessels that permit passive diffusion across their walls
very numerous delicate anastomosing tubes of 4-10 micrometer diameter
Arteries
clinical note
atherosclerosis
it is degenerating and metabolic lesions of large arteries in which tunica media is thickened by colesterole deposites and hardened by healing the thing which causes a disease
types
arterioles
tunica media : one or two layers of smooth muscle cells
tunica entima
thin sub endothelial layer of connective tissue
they are the major determinant to blood pressure
they regulate the flow of blood to the capillaries
they are the smallest arteries , with diameter less than 0.1 mm
they are the terminal branches of He arterial tree
medium sized muscular arteries
special sized medium arteries
small arteries
tunica adventitia
CT thiner than in tunica media
tunica media : 3-10 layers of smooth muscle cells
turnica entima
less smooth muscle
connective tissue
they distribute the blood flow to the arterioles
they are the smallest arteries , with a diameter Less than 1 mm
they are terminal branches of arterial tree
Large elastic arteries
their wall is composed of
tunica adventitia:
elastic connective is nourished by vasa vasororum
tunica media:
thick and elastic layer consists of fenestrated sheets of elastin separated by collagen fibers and many smooth muscle cells
tunica intima:
includes
with smooth muscle
thin layers of CT
endothelium
they are characterised by wide lumen and thick wall
they include aorta and its large branches
They are the largest arteries connected to the heart
conduct oxygenated blood from the heart to the tissues of the body
smooth muscle
they are present in
contraction of smooth
occurs more slowly and Lasts Longer than in skeletal and cardiac muscle because the rate of ATP hydrolysis is slower. Thus, smooth muscle contraction is not only prolonged but also requireleas energy
innervations of smooth muscle
sympathem noradrenergic nerves and parasympathetic cholinergic nerves
Em:
Glycogen granules
Gap junction
present between smooth muscle fibers to fascilitate the spread of excitation
smooth endoplasmic reticulum
Less developed and sparse but clossely associated with sarcolemmal vesicles
sarcolemmal vesicles (caveoli)
they are invagination of cell membrane (similar to t-tubules)
present along the periphery of the cell and termed caveoli
dense bodies
they may be similar to Zline in its function
located in both cacytoplan and sarcolemma
contractile filaments
they are
Intermediate filaments
dismin
vimentin
myosin
actin
they are involved in the synthesis of type III collagen, elastin, glycosaminglycin, the external lamina and growth factors
Ribosomes
Rough endoplasmic reticulum
golgi complex
mitocondria
LM:
they are arranged in layers, which may be
oplique
or
spiral
longtudinal
circular
Their cytoplasm appears hemogenous and acidophilic except for some dark patches called dense bodies
their Length varies from 30 micrometer in the wall of blood vessels to 500 micrometer in the wall of pregnant uterus
they have the smallest diameter of all muscle fibers (about 3 micrometer)
fusiform in shape with Central oval nucleus
the vescera of various systems (digestive , respiratory and genitourinary, etc)
the wall of blood vessels
they are non-stariated and involuntary
cardiac muscle
conducting system of the heart
it consists of
SA node (pacemaker)
AV bundle of Hiss
with its two branches
moderator band
Purkinje muscle fibers are different from other cardiac muscle fibers in:
they are richly supplied by nerves
they have no diad
they have fewer intercalated disks they have higher conductivity (5 times the other cardiac muscle fibers conductivity,
they are vaculated because they are rich With glycogen
they are paler in color with peripheral fewer myofibrils
they are larger in diameter
Each Purkinje fiber is formed of separate, short, thick elongated cylinderical cell
it is formed of special type of fiber called Purkinje fibers surrounded by connective tissue rich in blood capillaries
it is the right branch of AV bundle of Hiss
and their finer ramifications
cardiac muscle fiber
EM:
inclusions
present in either pole of the nucleus
atrial granules
ANF is a hormone that have an opposit action to aldosteron ie decreas sodium and water resorption in kidney
ANf is secrected in response to increased blood pressure and volume
ANf leads to reduction of blood fluid volume so the blood pressure decrease
are present in the atrial cardiac muscle cells and contain precursors of atrial natriuretic factor (ANF)
golgi complex present in association with the
mitocondria are more abundant than in skeletal muscles
Intercalated disks:
an intercalated disk is formed of
lateral portion
formed of
Gap junction
facilitatesion Coupling
Transverse portion
which is formed of:
2 Junction specializations
maculae adherens (desmosomes)
it prevents attachment of the cardiac muscle fibers from each other while contraction
fascia adherens
it serves as anchoring sites for the actin filaments of the terminal sarcrameres
step-like Junctions for mening and to end attachment between adjacent cardiac muscle cells.
sarcoplasmic reticulum (SR) and T-tubules system
In cardiac muscle, T-tubules occur at the Zline (instead of A-I junction as in skeletal muscle
Ttubules in cardiac muscle is wider than in skeletal muscle
SR is poorly defined and less organised than in skeletal muscles
Myofibrils and Myofilaments
I bands are biscected by z lines
they show dark A bands with H bands and z lines
thin actin and thick myosin a represent resulting in stariated appearance
their cross stariations are not regular as the skeletal muscles
cardiac myofibers are branching and anastomosing
LM: Cardiac muscle cells (fibers)have a similar structure to the skletal muscle with some differences
NB: No satellite cells ie.no stem cells are present
the cytoplasm is granular acidophilic and contains glucose granules, lipid droplets and some lipofusin pigments which increase with age
the fibers contain large oval nucleus (sometimes two nuclei are seen) The fibers exhibit a highly specialized end to end Junction known as intercalated disks which appear as dark transverse Line between the cardiac muscle fibers
the fibers branch and anastomose with each other
Each fiber is covered by a dilicate CT sheath rich in blood capillaries
The fibers are about 15 micrometers in diameter and about 80 micrometers long
cardiac muscle fibers are stariated and involuntary
The wall of the heart is formed of
Endocardium: the lining endothelium of the myocardium from inside
periecardium: the serous membrane covering the myocardium from outside
Myocardium: the cardiac muscle fibers
المنهج بدون تحديدات
Patho,micro,pharma
Ischemic Heart Diseases
Clinically: Cardiac ischemia may be manifested as:
Sudden death
Chronic ischaemic heart disease
MYOCARDIAL INFARCTION (M.I)
Ventricular aneurysm: This complication develops several weeks and months after the infarction. Typically it occurs at the site of large myocardial scars. The lumen of these aneurysms often contains mural thrombi.
Pericarditis: Sterile inflammation of the epicardium and exudation of fibrin. Healing --> fibrous adhesions.
Mural thrombosis: Overlying the infarction area.
Rupture of the enterventricular septum: Left to right shunt leading to right ventricular failure and pulmonary hypertension.
Rupture of papillary muscles --> mitral insufficiency.
Rupture of the myocardium: Occurs during the first week because the necrotic myocardium is very soft. Massive bleeding into the pericardial sac is called hemopericardium. The patient dies of cardiac tamponade.
Cardiogenic shock: Pump failure.
Sudden death: Most often due to arrhythmia.
Arrhythmia: The most common complication and the most common cause of death in the early infarction period.
Enzyme changes:
Leukocytosis زيادة عدد خلايا الدم البيضاءlasting not more than 1 week.
Lactic dehydrogenase (LDH): Peaks with SGOT and stays high for 7-10 days.
Serum glutamic oxaloacetic transaminase (SGOT): not specific for cardiac muscle. Peaks in 48-72 hr and falls over days.
Creatine kinase: 6 hours, peaks in 24 hr and falls in 72 hr. (MB isoenzyme useful for distinguishing myocardial from skeletal muscle diseases).
Myoglobin: 2 to 4 hours (very nonspecific; any muscle injury may cause elevation).
Creatine phosphokinase (CPK): Specific for cardiac muscles. Peaks in 24 hr and falls in 72 hr.
Troponin I: 4 hours (the most reliable test).
ECG changes: elevation of ST segment, inversion of T-wave and increased amplitude of Q-wave. Diagnostic ECG changes are found in 50% of cases during the first 2 days of onset of the infarction.
Clinical, Laboratory and ECG changes: - Chest pain, dyspnea, arrhythmia or sudden death.
Gross and microscopic features
The transmural infarct undergoes characteristic sequence of gross and microscopic changes. After 10 days the infarct heals by scar tissue.
10-14 days:
Increased collagen deposition, with decreased cellularity.
Gray-white scar, progressive from borders towards the center of the infarct.
2-8 weeks
Well-established granulation tissue with new blood vessels and collagen deposition.
The infarct is red-gray and depressed.
3-10 days:
Granulation tissue progressively replaces the necrotic area.
Phagocytosis of necrotic tissue by macrophages.
Macrophage infiltration with dying neutrophils.
Disintegration of dead myofibers.
The infarction area is yellow, soft depressed with red margin.
24-72h
PNLs polymorpho/nuclear lymphocytes infiltration.
Pyknosis of nuclei; myocyte hypereosinophilia.
The striations of muscle fibers are lost.
The area becomes pale yellow, soft.
By electron microscopy: Sarcolemmal disruption; mitochondrial amorphous densities.
None in first 6-12 hrs, although treatment with tri/phenyl/tetra/zolium chloride (TTC) can impart a red-brown color on non-infarcted myocardium (due to presence of dehydrogenase enzyme), thereby highlighting the infarction areas even at 3-6 hrs post infarction.
In the first 6-12 h:
Anatomic and morphologic types of MI:
Subendocardial: an area of ischemic necrosis that does not extend through the full thickness of myocardial wall segment(s) (limited to the endocardium or to the endocardium and myocardium)
Transmural: Ischemic necrosis of full thickness of the affected muscle segment(s), extending from the endocardium through the myocardium to the epicardium.
The extent of infarction depends on the site of occlusion of the affected vessel and the state of the collateral circulation.
If the superimposed thrombus undergoes lysis either spontaneously or by fibrinolytic treatment soon after occlusion, the injured myocardial cells restore their vitality within 1-2 days.
Thrombosis and vasoconstriction follow the acute plaque change leading to complete vascular occlusion.
If such an occlusion persists for more than 20 minutes, irreversible myocardial cell damage and cell death will occur.
The initial event is ulceration, fissuring and hemorrhagic ballooning of atheromatous plaque.
The major cause of myocardial infarction is coronary atherosclerosis. The noncomplicated atheroma usually occludes at least 75% of the cross diameter of the affected vessel. Loss of contractility occurs with 1-2 min of ischemia, ATP is 50% depleted at 10 min, irreversible injury occurs at 20-40 minutes.
Sites of coronary artery occlusion:
Circumflex branch of Lt. coronary --> infarction in the lateral wall of Lt. ventricle.
Rt. coronary artery --> infarction in the posterior wall of Lt. ventricle and posterior part of interventricular septum.
Proximal 2 cm of anterior descending branch of Lt.(left)coronary (commonest) --> infarction in anterior wall of Lt. ventricle and anterior part of interventricular septum.
Risk factors:
Minor risk factors:
Oral contraceptives. حبوب منع الحمل
High stress life, obesity.
Family history of atherosclerotic arterial disease.
Old age, more in males.
Major risk factors:
Hypertension
Incidence: The incidence of M.I increases with age however, the actual incidence is dependent on predisposing risk factors for atherosclerosis. In children, M.I may occur in cases of vasculitis.
Definition: Localized irreversible myocardial damage or death due to sudden occlusion of coronary blood supply. Myocardial infarction occurs when myocardial ischemia exceeds a critical threshold that overcomes the myocardial repair mechanisms, resulting in localized irreversible myocardial damage or death.
ANGINA PECTORIS
Clinically: 3 distinctive patterns:
UNSTABLE ANGINA:
The perfusion deficit is multifactorial including;
Fissuring, ulceration of atheroma.
Vasospasm
Atherosclerosis.
Usually of prolonged duration.
They may occur at rest or after minimal effort.
Anginal attacks occur in increasing frequency.
PRINZMETAL'S ANGINA:
ECG shows elevated ST segment because ischemia is transmural.
Occurs at rest (unrelated to physical activity) due to coronary artery spasm
TYPICAL (STABLE) ANGINA:
Electrocardiography (ECG) shows depressed ST segment because ischemia is most intense in the subendocardial region of the left ventricle.
Usually results from reduction of coronary perfusion as in cases of atherosclerosis
Precipitated by increased physical activity or emotionalstress.
Definition: Paroxysms of substernal or precordial pain or discomfort resulting from cardiac ischemia. The pain is described as constricting, choking or knife-like. The condition is usually reversible.
Causes of cardiac ischemia:
Increased myocardial demand: as in tachycardia.
Decreased O2 transport: as in lung fibrosis, congenital heart diseases and anemia.
Decreased coronary blood flow: Chronic ischemia results only after 70% reduction in cross sectional area of the affected artery.
Causes of coronary artery occlusion:
Emboli from the left side of the heart (e.g. vegetations in subacute bacterial endocarditis).
Arteritis superimposed by thrombosis.
The most common cause is atherosclerosis superimposed by thrombosis or vasospasm.
Definition: Sudden or gradual occlusion of coronary blood supply depending on the nature of coronary artery disease. The left ventricle is the main affected chamber.
STREPTOCOCCI and RHEUMATIC FEVER
classified according to:
Carbohydrate antigen (Lancefield classification):
The clinically most important groups are group A (Str. Pyogenes) and group B (Str. Agalactiae).
A polysaccharide present in the cell wall of streptococci, known as C- carbohydrate,
Hemolytic properties
Gamma hemolytic: non-hemolytic e.g. Str. bovis.
Alpha hemolytic: partial hemolysis with greenish discoloration e.g. Str. viridans and Str. pneumoniae.
Beta hemolytic: complete hemolysis with a clear zone around the colonies e.g. Str. pyogenes and Str. agalactiae.
Cardiovascular system diseases
RHEUMATIC FEVER
Prognosis of acute rheumatic fever:
Death from severe myocarditis.
Recurrence of acute attacks with development of chronic rheumatic heart disease.
Recovery after few weeks in most cases.
Clinical manifestations & Lab. findings of rheumatic fever:
N.B: The diagnosis of rheumatic fever requires at least 2 major John's criteria or one major criterion with 2 minor criteria.
Minor criteria
Elevated ESR erythrocyte sedentation rate, CRP c reactive protein and ASO antistreptolysin O titer.
Leukocytosis
Arthralgia
Previous attack of rheumatic fever.
Major John's criteria:
Sydenham's chorea.
Erythema marginatum.
Subcutaneous nodules.
Arthritis
Carditis
AFFECTED ORGANS:
SKIN
Subcutaneous nodules:
Microscopic picture: Granulomatous reaction formed of Aschoff’s nodules.
Gross picture: Circumscribed nodules about 2 cm in diameter, mobile and firm in consistency. The overlying skin is edematous but not ulcerated.
Sites: Over bony prominences, on extensor surfaces of limbs, skull and in relation to vertebral column.
JOINTS
Microscopic picture: Acute sero-fibrinous inflammation of the synovium with exudation in the joint cavity.
Leaves no deformity because the articular cartilage is not affected.
Migratory (fleeting): i.e. affecting one joint after the other.
Affect usually large joints as the knee and ankle.
HEART
Acute rheumatic heart disease characterized by Pan-carditis (myocarditis, endocarditis and pericarditis).
Fibrin results in adhesions between the parietal and visceral layers of pericardium and interfere with cardiac action.
Sero-fibrinous inflammation of the pericardium.
Endocarditis
Mural: Inflammation and edema of mural endocardiom. McCallum's patchs: represent Aschoff's nodules, usually seen in the posterior wall of the Lt. atrium.
Valvular
Vegetations: thrombi formed mainly of platelets and fibrin.
The affected valves show inflammation, edema and ulcerations
The valve surface reveals small (1-2 mm) whitish rubbery adherent platelet and fibrin thrombi called vegetations.
Vegetations are usually formed at the lines of valve closure i.e. the atrial surface of mitral valve and ventricular surface of the aortic valve. Affection of pulmonary & tricuspid valves are less common.
The most serious effect of rheumatic fever due to valvular affection.
Aschoff 's nodules in the interstitial fibrous tissue areas.
Cloudy swelling and fatty degeneration of myocardial fibers.
Small rounded grayish-white Aschoff`s nodules, called Ascoff bodies in the interstitial fibrous regions of the heart.
Mild cardiac dilatation and softening of myocardium.
Tissue reaction:
Healing phase: The lesions undergo fibrosis.
Proliferative tissue reaction: Granulomatous phase characterized by formation of Aschoff's nodules. It identified in the heart, joints and other tissues.
Aschoff’s nodule:
Microscopic picture: Central area of fibrinoid degeneration surrounded by lymphocytes, macrophages and plasma cells. With chronicity there is a palisade of histiocytes and multinucleated giant cells with multiple central nuclei and basophilic cytoplasm (Aschoff cells). The nodule is surrounded by fibroblasts.
Gross picture: Grayish-white nodule measuring about 1-2 mm usually found paravascular.
Exudative tissue reaction: Tissue edema and infiltration by PNLs polymorphonuclear lymphocytes, plasma cells and histiocytes. Collagen fibers undergo disintegration (fibrinoid degeneration). It mostly identified in serous sacs as pericardium, pleura and joint cavities.
Etiology and pathogenesis of rheumatic fever.
Two theories explain the immunological disorders in Rh. fever:
Another theory stated that streptococcal toxins produce alterations in the cardiac tissue which become considered by the immune system as foreign. This is followed by reaction between the altered cardiac tissue and anti-streptococcal antibodies.
One theory stated that, the cell wall of the organism contains M-protein which has antigenic similarity to cardiolipin of the cardiac tissues. Antibodies against streptococcal M-protein cross react with sarcolemma of cardiac muscle fibers and smooth muscle cells of arteries --> cytokine release and tissue destruction.
Rheumatic fever is an immune-mediated disease occurring 2-3 wks after infection by group A β-hemolytic streptococci. During a streptococcal infection the APC antigen presenting cells as macrophages present the bacterial antigen to helper T cells which activate B cells to produce antibodies against streptococcal antigens.
Bad ventilation. - Recurrent streptococcal infections. - Familial predisposition.
Sex and age: More common in female children and young girls from 5-15 years (school age).
Definition: Acute recurrent immune-mediated post-streptococcal disease characterized by wide-spread inflammatory & degenerative changes in a variety of tissues mainly heart and joints.
Heart Failure
Drugs Used in Treatment of Heart Failure
Vasodilators: The most beneficial
β-adrenoceptor blockers in small doses (usually started as 1/8 the dose used in other indications):
Nitrates:
IV infusion of nitroglycerine for acute pulmonary edema.
the oral preparations for CHF
ARBs (angiotensin receptor blockers) e.g. losartan: if contraindicated the following choice is:
ACEIs: e.g. captopril and lisinopril, are absolutely the best,
Diuretics: 1. ↓↓ Blood volume → ↓↓ VR → ↓↓ EDV → ↓↓ preload & ↓↓ pulmonary congestion.
Loop diuretics e.g. frusemide
Thiazides e.g. hydrochlorothiazide
Inotropic agents → ↑↑ contractility → ↑↑ COP
β1-Agonists: dopamine, dobutamine (in acute heart failure)
Bipyridines: amrinone & milrinone (in acute heart failure)
Digitalis (digitoxin & digoxin):
NYHA classification
Class IV Defined by symptoms at rest or with any physical activity
Class III Characterized by a marked limitation in normal physical activity
Class II When ordinary physic al activity results in fatigue, dyspnea, or other symptoms.
Class I Describes a patient who is not limited with normal physical activity by symptoms (diagnosis by investigations e.g. ECG, ECHO)
Ordinary classification
Chronic heart failure:
ACUTE HEART FAILURE
Effects: Generalized acute venous congestion (general pathology).
Causes: 1- Arrhythmias 2- Angina pectoris 3- Myocardial infarction. 4- Acute infections 5- Myocarditis. 6- Hypertension 7- Massive pulmonary embolism. 8- Rupture of cardiac aneurysm 9- Pericardial hemorrhage (cardiac tamponade)
Pathophysiology: Impaired pump function due to decreased myocardial contractility or increased cardiac demands due to pressure or volume overload. Compensatory mechanisms aim to maintain tissue prrfusion. These mechanisms include increased stroke volume and tachycardia. With time, chronic pressure or volume overload led to myocardial hypertrophy, ventricular dilatation and heart failure.
Definition: It is the inability of the heart to pump blood sufficiently to meet the body circulatory demands.
CONGENITAL HEART DISEASES
Classification of congenital heart diseases:
Other anomalies
abnormal origin of the carotid arteries.
Missing or supernumerary cusps
Malposition of the heart,
Dextro-cardia: the heart lies in the Rt. hemithorax
Ectopia cordis: The heart lies outside the chest wall, or may be in the abdomen.
Cyanotic group:
4. Tricuspid atresia with ASD.
3. Persistent truncus arteriosus.
2. Tetralogy of Fallot.
1. Transposition of great vessels.
Corrected form:
The common form:
Acyanotic group:
5. Isolated aortic or pulmonary valve stenosis.
4. Coarctation of aorta.
post-ductal coarctation (adult type):
pre-ductal coarctation (infantile type):
3. Patent ductus arteriosus (PDA).
2. Atrial septal defect (ASD).
Ostium secundum defect:
Ostium primum defect:
1. Ventricular septal defect (VSD).
The clinical picture varies according to the size of the defect:
Larger defect causes heart failure and cyanosis.
Small defect in the muscular part is clinically insignificant. This is called Roger's disease
Isolated cases represent only 30%.
It is usually associated with other cardiac anomalies as Fallot's tetralogy, patent ductus arteriosus, ASD.
The most common congenital cardiac anomaly.
Congenital cardiac defect associations
Turner syndrome: Bicuspid aortic valve, coarctation of aorta
Infant of diabetic mother: Transposition of great vessels, VSD
Down syndrome : AV septal defect
Congenital rubella: PDA, pulmonary artery stenosis, septal defects
Alcohol exposure in utero: VSD, PDA, ASD, tetralogy of Fallot
22q11 syndromes : Truncus arteriosus, tetralogy of Fallot
Williams syndrome : Supravalvular aortic stenosis
Prenatal lithium : Ebstein anomaly
Marfan syndrome: MVP, thoracic aortic aneurysm and dissection, aortic regurgitation
Manifestations of congenital heart diseases may be:
Manifested in adult life.
Manifested shortly after birth.
Incompatible with life.
Clinical manifestations of congenital heart diseases: - Failure to thrive. - Cyanosis. - Increased risk of infective endocarditis.
Causes: 1- Chromosomal disorders: Down's syndrome (trisomy 21). 2- Environmental factors: Rubella infection, radiation, drugs, alcohol intake, cigarette smoking in the first trimester of pregnancy.
VALVULAR DISEASES
PULMONARY STENOSIS (P.S):
Right-sided heart failure
Right ventricular hypertrophy
Carcinoid syndrome
Atherosclerotic changes.
Congenital stenosis
AORTIC STENOSIS (A.S):
Generalized ischemia.
Left ventricular failure.
Concentric hypertrophy of left ventricle.
Atherosclerotic changes (e.g. senile aortic stenosis).
Healed rheumatic valvulitis or subacute bacterial endocarditis.
Congenital stenosis.
AORTIC INCOMPETENCE (A.I):
Blood regurgitates from the aorta to the left ventricle during vevtricular diastole --> Left ventricular hypertrophy. - Relative mitral incompetence due left ventricular dilatation --> hypertrophy and dilatation of left atrium --> pulmonary hypertension --> Hypertrophy and dilatation of the right atrium and tight ventricle.All cardiac chambers become dilated (cor bovinum).
Syphilitic aortitis.
Healed rheumatic valvulitis
MITRAL VALVE PROLAPSE:
Rupture & sudden death.
Infective endocarditis.
Arrhythmia
It usually affects young ages (20-40 years).
One or the 2 cusps of the mitral valve become floppy and balloon back into the left atrium during systole.
MITRAL INCOMPETENCE (M.I)
Pulmonary congestion, hypertension --> Rt sided heart failure.
Hypertrophy of the left ventricle because it receives extra amount of blood during diastole --> Left ventricular failure
Hypertrophy and dilatation of the left atrium due to regurge of blood during ventricular systole
Relative M.I. due to dilatation of the left ventricle as in anemia And hypertension
Healed rheumatic valvulitis or subacute bacterial endocarditis
MITRAL STENOSIS (M.S):
Formation of thrombus in left atrium (ball thrombus)
Right-sided heart failure.
Hypertrophy & dilatation of the Rt. atrium and Rt. ventricle
Chronic venous congestion of the lung --> pulmonary hypertension.
Dilatation and hypertrophy of left atrium
Gross picture: The valve is fibrotic with thickened cusps. The valve orifice is narrow and slit-like (fish-mouth or Button-hole or funnel shaped).
Subacute bacterial endocarditis.
Healed rheumatic valvulitis.
MYOCARDITIS
Trichinosis: Encysted larvae. - Inflammatory cellular infiltrate. Later on: progressive fibrosis.
Bacterial (pyogenic) myocarditis: - Suppurative reaction, microabscesses. - Interstitial edema.
Viral myocarditis: - Isolated myofiber lysis. - Inflammatory lymphocytic infiltrate. - Interstitial edema.
Gross picture: - Normal-sized or enlarged heart. - Pale foci and minute hemorrhages. - Small foci of fibrosis. - Mural thrombi. The inflammatory process ending in fibrosis.
Clinically: - The condition may be asymptomatic and is suspected by ECG. - Arrhythmia, fatigue, dyspnea, palpitations, pericordial discomfort and mild fever. - Death due to cardiac failure. - Viral cases (years later) --> Congestive cardiomyopathy.
Non-infectious:
Physical agents: Radiation, trauma
Immune-Mediated Reactions: Post-viral, Post-streptococcal rheumatic fever, SLE, Transplant rejection, drug hypersensitivity
Definition: It is inflammation of the heart muscles that characterized by leukocytic infiltration, necrosis or degeneration of the myocytes.
ENDOCARDITIS
non-infective:
Libman-Sacks verrucous endocarditis of SLE.
Non-bacterial thrombotic: in debilitating diseases & malignancy.
Rheumatic
Definition: Inflammation of mural and valvular endocardium.
ACUTE BACTERIAL ENDOCARDITIS
Angina Pectoris
Types of angina pectoris:
Variant (Prinzmetal's, vasospastic angina) angina:
Due to reversible coronary vasospasm.
Occurs at rest, usually accompanied by arrhythmia.
Unstable angina (pre-infarction):
Treatment: Hospitalization + Coronary VDs + ↓ Cardiac work + Antiplatelets + LMW heparin, and statins.
Due to formation of labile non-occlusive thrombi at the site of a fissured or ulcerated atherosclerotic plaque.
Occur at rest with change in the frequency and duration of chest pain.
Angina of effort (exertional, stable or classic angina):
Treatment by ↓ cardiac work.
Due to coronary atherosclerosis
Occurs on exertion.
The most common type.
Angina is a type of chest pain due to transient myocardial ischemia; it is due to imbalance between oxygen demand and coronary oxygen supply.
Biochemistry
Cardiac Metabolism
Lipid Transport
Composition of lipoproteins: Lipoproteins= lipid part + protein part “apolipoproteins”.
Metabolism of lipoproteins
Metabolism of chylomicrons
LDL-cholesterol /HDL-cholesterol ratio and coronary artery disease:
Hyperlipoproteinemia
There is an inverse relationship between HDL concentration and coronary artery disease, making the LDL/HDL cholesterol ratio a good predictive parameter. The optimal ratio is 4. To avoid atherosclerosis and coronary heart disease, we must try to raise HDL-cholesterol and to lower LDL-cholesterol.
HDL high density lipoproteins
HDL contains two enzymes which inhibit the oxidation of LDL;
PAF-acetyl hydrolase
paraoxonase
Functions of HDL:
HDL is considered as anti-atherogenic particles.
Acts as reservoir of apo CII and apo E for other types of lipoproteins e.g. VLDL and chylomicrons.
Esterification of cholesterol by LCAT.
Carries cholesterol from tissues to the liver "Reverse cholesterol transport".
Metabolism of HDL:
Nascent HDL are disc-shaped containing phospholipids, cholesterol and apolipoproteins A, C and E. They are rapidly converted to spherical particles when lecithin-cholesterol acyl transferase (LCAT) binds to the surface of discoidal HDL converting free cholesterol to cholesterol ester and the HDL particles become spherical.
HDL is synthesized and secreted from both liver and intestine. However, apo C and apo E are synthesized in the liver and transferred from liver HDL to intestinal HDL.
Types of apolipoproteins: A, C, D, E.
Main lipid type: phospholipids and cholesterol.
Amount of proteins: 40 %.
Site of synthesis: liver: intestine.
LDL low density lipoproteins
Catabolism of LDL:
Oxidized (Ox-LDL)
Oxidized LDL are taken by macrophages and converting it into foam cells which play a central role in atherosclerosis.
Factors which increase LDL-oxidation:
Diet rich in trans fats.
Uncontrolled diabetes.
Metabolic syndrome.
The oxidation of LDL occurs when the LDL-cholesterol particles react with free radicals. The Ox-LDL itself then becomes more reactive with the surrounding tissue, resulting in tissues damage.
70% of LDL is degraded in the liver.
Any defect or absence of LDL-receptors →↓ uptake of LDL →↑ LDLcholesterol →familial hypercholesterolemia.
Estrogen “Female sex hormone” ↑ the number of LDL-receptors in the liver, so blood cholesterol in females is low during reproductive period. Also, PUFA ↑ the number of LDL-receptors.
30% of LDL is degraded in extrahepatic tissue.
LDL binds via ApoB100 and Apo E to LDL-receptors on both liver and extrahepatic tissues.
Function: Carries cholesterol to peripheral tissues.
Main lipid type: Cholesterol.
Formed in plasma from catabolism of VLDL
Formation of LDL “low density lipoproteins”
Apo D is called cholesterol ester transfer protein.
Phospholipids and triacylglycerols are transferred upon Apo D from IDL to HDL, while at the same time cholesterol ester is transferred from HDL to IDL converting it into LDL.
Formation of IDL “Intermediate density lipoproteins”
Lipoprotein lipase acts on triacylglycerols of VLDL hydrolysing it into glycerol and FA. After that VLDL is converted to IDL.
Metabolism of VLDL
Nascent VLDL is synthesized by the liver and contains Apo B100. In plasma, it receives Apo CII and Apo E from HDL and becomes VLDL.
The triacylglycerols carried by VLDL is endogenous synthesized from excess carbohydrates.
Main lipid type: Triacylglycerols.
Amount of proteins: 10%
Amount of lipids: 90%.
Function: Carries lipids from liver to the peripheral tissues.
Site of synthesis: Liver.
The post-prandial turbidity is cleared by lipoprotein lipase enzyme.
Lipoprotein lipase is secreted from vascular endothelium of capillaries of adipose tissues, cardiac, skeletal muscle and is activated by Apo CII. It hydrolyses triacylglycerol of chylomicrons into glycerol and FA.
Apo CII and Apo E return to HDL.
Deficiency of either lipoprotein lipase or Apo CII→ results in accumulation of triacylglycerol rich lipoprotein (Type I hyperlipoproteinaemia).
Apo CII returns to HDL and chylomicrons become shrinked and called chylomicron remnant which are removed by the liver receptor which recognize Apo B48 and Apo E.
So, this enzyme is called clearing factor
In plasma, chylomicrons take apo CII and apo E from HDL and becomes chylomicrons.
Chylomicrons pass through lymphatics→ thoracic duct → superior vena cava → heart → systemic circulation causing post prandial turbidity.
chylomicrons is formed in the intestinal mucosa after meal, but can’t pass through the portal circulation because of its large size. This chylomicron contains apo B48 and called nascent chylomicrons.
Main lipid type→ dietary triacylglycerol
Amount of proteins→ 2%
Amount of lipids→ 98%
Function: Carry dietary lipids from intestinal mucosa to peripheral tissues.
Time of biosynthesis→ after meal
Site of biosynthesis→ Intestinal mucosa
Structure of Lipoproteins:
Plasma lipoprotein particle consist of a core of triacylglycerol and cholesterol ester surrounded by a layer of phospholipids and cholesterol.
The apolipoproteins may be integral part “can,t be removed” such as apo A and B or peripheral part “can be removed” such as apo E and apo D.
Phospholipids are arranged in a manner that the polar groups are faced outside while the non polar groups are toward inside
These types of lipoproteins differ from each other in:
Main type of lipids.
Amount of lipids
Types of apolipoproteins
Amount of proteins
Site of biosynthesis
Types of lipoproteins:
High density lipoprotein (HDL).
Low density lipoproteins (LDL).
Very low density lipoproteins (VLDL).
Chylomicrons
Separation of lipoproteins:
Lipoproteins can be separated by two methods:
Electrophoresis
Ultracentrifugation
Apolipoproteins: They are synthesized in liver and intestine.
apo E
apo D
apo C (apo CI, apo CII, apo CIII)
apo B (apo B48, apo B100)
apo A (A1 , A2 )
Lipids are insoluble in water; to be carried in plasma it must be soluble in water. So, lipids combine with protein to form water soluble complex called lipoproteins.
Cholesterol
Causes of hypercholesterolemia:
Regulation of Cholesterol Synthesis
HMG - CoA reductase is the key enzyme for cholesterol synthesis.This enzyme is regulated by:
Drugs : Hypocholesterolemic drugs e.g.Lovastatin, Mevastatin inhibit HMGCoA reductase by competitive inhibition.
Feed-back regulation: HMGCoA reductase is inhibited by mevalonate and cholesterol.
Hormonal regulation:
HMG - CoA reductase is present in two forms active (dephosphorylated) and inactive (phosphor-ylated).
The activity of the enzyme is regulated by cAMP dependent enzyme system
decreased by fasting and by glucagon.
increased by carbohydrate feeding and by insulin
Sources of cholesterol:
Endogenous source: Each cell can synthesize its own cholesterol, but plasma cholesterol is formed by the liver ( 1 gm/day ).
Dietary Sources: Liver, kidney, brain, red meat and egg yolk are rich sources for cholesterol.
Excretion About 1g of cholesterol is excreted daily, 50% in the form of bile acids and 50% as cholesterol. Intestinal bacteria reduce cholesterol to coprostanol, which is the principal sterol in feces. Bile acids that are excreted in bile are partly reabsorbed into the portal blood to the liver and re-excreted in bile (Enterohepatic circulation). The main bile acid present in stool is lithocholic acid (the least soluble bile acid).
Functions of Cholesterol
Synthesis of bile acids and salts:
Synthesis of Vitamin D3
Formation of lipoproteins: Cholesterol and cholesteryl esters enter in the formation of plasma and cell membrane lipoproteins.
Synthesis of steroid hormones: Cholesterol is the precursor of androgens, estrogens, progesterone, and corticoids.
Blood cholesterol level:
Elevated LDL/HDL cholesterol ratio more than 4/1 (atherogenic index) predisposes to atherosclerosis and coronary heart disease
75% of cholesterol is carried on LDL.
LDLs act as carriers of cholesterol for extrahepatic tissues
25% of cholesterol is carried on HDL.
HDLs act as the main carrier of cholesterol from tissues to the liver (reverse cholesterol transport), where cholesterol is excreted into bile, converted to bile acids or reused in synthesis of lipoproteins.
In the blood, 70% of cholesterol is esterified with long chain fatty acids, while 30% is free.
Cholesterol ester is metabolized more rapidly than cholesterol and does not precipitate in vascular endothelium.
Esterification of cholesterol :
In tissue: By Acyl-Cholesterol Acyl transferase enzyme ACAT.
In plasma: by Lecithin-Cholesterol Acyl transferase enzyme LCAT present in HDL
Blood cholesterol level: 150 - 220 mg/dl
Distribution of cholesterol inside the body: Fig (43) Inside the body, cholesterol is present in high concentrations in: liver, brain, ovary, testis, and supra-renal cortex.
Biosynthesis of cholesterol
Sources: Acetyl CoA.
Site : Cytoplasm.
The enzymes responsible for synthesis of cholesterol are present in the microsomal and cytosolic fraction of cells.
Ketone bodies Metabolism
Ketone Bodies in Blood
Ketosis is a condition characterised by elevated levels of ketone bodies in blood (Ketonemia) and their excretion in urine (ketonuria).
Complication of Ketosis
Ketosis may be associated with electrolyte loss especially potassium in case of diabetics (as insulin stimulates intracellular accumulation of K+)
High levels of acetoacetate and β-hydroxybutyrate in ketosis are accompanied by acidosis, and if not treated this may proceed to acidemia, coma or even death.
Causes of Ketosis
Prolonged and severe muscular exercise.
Severe uncontrolled diabetes mellitus.
High fat and low carbohydrates in diet
Prolonged fasting or starvation.
Normally, there is a balance between the ketogenesis in the liver and ketolysis in extrahepatic tissues. As, the rate of ketogenesis increases, the rate of ketolysis proportionally increases till reaches a maximum, after that any increase in ketogenesis will produce increase in ketone bodies in blood.
They are present at very low concentration, about 1 mg/dl.
The main ketone bodies of blood are acetoacetate and 3 - hydroxybutyrate
ketolysis
Site: occurs in the mitochondria of extra hepatic tissues due to the presence of CoA transferase (Succinyl- CoA – acetoacetate – CoA transferase).
Ketolysis is breakdown of ketone bodies into acetyl CoA which is oxidized in Kreb,s cycle to H2O,CO2 and water.
Ketogenesis
Regulation of Ketogenesis
Factors that decrease ketogenesis:
Insulin in case of diabetes.
Feeding of glucose or carbohydrates.
Factors that increase ketogenesis
Besides substrate availability, enzyme induction is important for ketogenesis. The synthesis of β-HMG-CoA synthase – the rate limiting enzyme of ketogenesis from acetyl CoA- is stimulated powerfully by:
Diabetes mellitus due to impaired glucose oxidation and increased fatty acid oxidation.
Administration or hypersecretion of anti-insulin hormones.
High fats and low carbohydrates in diet.
Carbohydrate deficiency.
Fasting and starvation .
Site: It occurs in the mitochondria of liver cells due to the presence of two enzymes, HMG-CoA synthase and HMG-CoA lyase.
Definition: Ketogenesis is synthesis of ketone bodies from active acetate derived from β-oxidation of fatty acids.
FA oxidation --> active acetate --> ketone bodies
Oxidation of fats
The free fatty acids diffuse from adipose cells, combine with albumin in the blood, and are thereby transported to other tissues, where they passively diffuse into cells for oxidation and further pathways.
Fatty Acids Oxidation
There are 3 mechanisms for fatty acids oxidations:
ω--oxidation of fatty acids.
α-oxidation of fatty acids.
β-oxidation of fatty acids.
Site: ● Mitochondria of most cells prominent in liver, heart and skeletal muscle but, not in brain.
Carnitine deficiency: Occurs in prematures due to inadequate intake or in hemodialysis , liver diseases due to decrease biosynthesis, malnutrition and vegeterians. Carnitine defi ciency leads to muscle weakness during long-term exercise (when fatty acids are an important source of energy)
Inhibitors of carnitine shuttle: Malonyl CoA inhibits CPT-1. Therefore, when fatty acid synthesis is occurring in the cytoplasm , the newly made palmitate cannot be transferred into the mitochondria and degraded.
Carnitine palmitoyltransferase-2 (CPT-2) deficiency: affects skeletal muscle
Carnitine palmitoyltransferase-1 (CPT-1) deficiency: Affects only the liver, resulting in reduced fatty acid oxidation and ketogenesis, with hypoglycemia. Sulfonylurea drugs, used for treatment of type 2diabetes, reduce fatty acid oxidation by inhibiting CPT-1 therefore increasing glucose utilization.
Oxidation of odd number fatty acids
Definition : Oxidation of fatty acid at β-carbon to give acetylCoA which is then oxidized in Kreb,s cycle.
Triacylglycerols are hydrolysed into fatty acids and glycerols. The release of fatty acids is controlled by a complex series of lipolytic cascades that result in the activation of hormone-sensitive lipase enzyme.
Physio
Physio 2
Cardiac Output (COP)
Regulation of COP: [COP= SV x HR= (EDV-ESV) x HR]
Effect of anaemia on COP:
Causes of hyperdynamic circulation in anemia:
Diminished viscosity of the blood decreased peripheral resistance which causes a rapid shift of blood from the arterial to venous side.
O2 lack and CO2 excess have direct VD effects.
In anemia, there will be a rapid shift of blood from the arterial to venous side (hyperdynamic circulation) causing marked increase in VR and COP.
Effect of exercise on COP regulation:
Other effects of exercise:
Increased breathing rate in response to activation of chemoreceptors
Bronchodilatation mediated by β2 adrenoceptors.
Vasoconstriction of blood vessels supplying the inactive organs e.g. (the gut) through ἀ1 adrenoceptors
Vasodilatation of arteries that supply skeletal muscle through cholinergic fibers (partly mediated by the endothelium)
Mechanism of increasing COP during exercise: (COP= SV x HR)
Arteriolar dilatation, caused by O2 lack, CO2 excess, acidosis and other metabolites, increases VR and COP.
Direct impulses from the cerebral cortex to the cardiac centers increase HR and contractility.
Increased HR due to direct stimulation of the cardiac centers by O2 lack, CO2 excess, acidosis and release of metabolites.
Venoconstriction that occurs due to sympathetic stimulation increases MSFP, VR and COP.
Increased contractility (SV) and heart rate (HR) due to sympathetic stimulation.
According to the type of exercise i.e.
It is increased up to 700% (35 L/min) during severe exercise in well trained persons.
COP is increased during mild walking to 200% (10 L/min).
Effect of venous return (VR, preload, EDV) on COP regulation:
Factors affecting VR (and COP): [VR= (MSFP-RAP)/RVR] where VR, venous return; MSFP, mean systemic filling pressure; RAP, right atrial pressure; RVR, resistance to venous return
Other factors affecting VR
e.g. respiratory pump i.e. increased intrathoracic negativity (e.g. during inspiration) increases VR.
Resistance to venous return (RVR):
It is inversely related to VR.
Definition: it is the resistance which blood meets during its flow from the arterial side to the right atrium.
Right atrial pressure (RAP, central venous pressure, CVP):
Increase RAP (e.g. congestive heart failure) decreases VR (VR becomes equal 0 when the RAP becomes equal MSFP). [VR= (MSFP-RAP)/RVR]
Normal value: about 2 mmHg (with a range from 0 to 5 mmHg).
Definition: it is the mean pressure in the right atrium.
Mean systemic filling pressure (MSFP):
Factors that affect the MSFP (and VR):
Muscular activity: increases MSFP. This is due to compression of the vascular bed by the contracting muscles.
Increased sympathetic tone: constricts all the blood vessels decreasing the vascular capacity with marked elevation of the MSFP.
Capacity of vascular system: increased capacity of the vascular bed e.g. by vasodilation especially in the veins and capillaries as in anaphylactic or histamine shock leads to a marked decrease in MSFP.
Increased blood volume increases MSFP
Normal value of MSFP: 7 mmHg.
Definition: it is the pressure measured everywhere in the systemic circulation one minute after blood flow has been stopped by clamping large blood vessels at the heart. So, it is impossible to be measured in living animal.
Role of VR in regulation of COP: (SV= EDV-ESV)
So, increased VR increases both SV and HR which increase COP in order to maintain balance between VR and COP. (COP= SV x HR)
Increase in VR increases:
HR (Bainbridge effect).
EDV which increases SV (heterometric autoregulation).
It is the most important factor controlling COP as the heart adjusts itself in order to keep COP equal to VR (venus return).
Effect of mean arterial blood pressure (MABP, afterload) on COP regulation
Effect of increased MABP (mear arterial blood pressure): it causes the heart to pump less amount of blood than it receives for several beats resulting in accumulation of the blood in the ventricles increasing the size of the heart with subsequent increase in the initial length of the cardiac muscle. Thus, the heart contracts more forcefully resulting in increased COP to its normal level (Frank-Starling law).
Definition of afterload: it is the force against which the heart is contracting (aortic pressure).
Effect of changes in HR on COP regulation:
Marked increase or decrease in HR: decreases COP.
Mechanism of decrease in COP:
Marked decrease in heart rate (<60 beat/min): although it increases the time of diastole and the ventricular filling and SV, yet, the increased SV cannot compensate for marked decrease in HR. This occurs when the ventricle beats by its idioventricular rhythm (25 -40 heart/minute).
Marked increase in HR (>160 beat/min) causes marked shortening of the diastolic period leading to:
Decrease in the time of main coronary flow which causes decrease in the force of contraction and consequently decreases SV and COP i.e. the increase in the heart rate cannot compensate for the marked decrease in stroke volume.
Decrease in filling of the ventricle which decreases EDV resulting in decrease in SV and COP.
Mild and moderate changes in HR (60- 160 beat/ minute): do not affect the COP (i.e. compensated), provided that, venous return is kept constant.
Effect of cardiac contractility (and SV) on COP:
Extrinsic regulation of cardiac contractility, SV and COP:
Effect of hormones and chemicals on SV and COP (i.e. hormonal regulation of COP):
Hormones affecting COP:
Glucagon: has a positive inotropic effect through increasing cAMP.
Thyroxine: increases COP by exerting positive inotropic and chronotropic effects.
Catecholamines: have the same effects as sympathetic stimulation i.e. they increase COP.
Effect of autonomic nervous system on SV and COP (i.e. neural regulation of COP
Parasympathetic nervous system decreases COP through decreasing HR i.e. negative chronotropic effect.
Sympathetic nervous system increases COP through increasing:
Venous return and filling of the heart as it causes venoconstriction.
Cardiac contractility i.e. positive inotropic effect.
HR (heart rate) i.e. positive chronotropic effect.
Intrinsic regulation (autoregulation) of COP: [occurs also in transplanted or denervated heart]
In certain situation e.g. muscular exercise, the heterometric and homeometric autoregulations operate at the same time for a long time to maintain marked increase in SV although heterometric mechanism starts first.
Homeometric autoregulation:
This mechanism is lost in cardiac failure.
This mechanism occurs in prolonged exercise.
It starts 2-5 minutes after increase in the venous return after heterometric autoregulation; the EDV starts to return gradually to its normal level.
Definition: it is the increase the force of contraction without increase in EDV.
Heterometric autoregulation (Starling's law):
Physiological limitations: overstretch of the myocardial fibers leads to weakening of the contraction and decrease in SV and COP
It is the only mechanism controlling the COP in cardiac failure.
This mechanism starts about 30 seconds after increase in venous return i.e. at the beginning of exercise, there is an increase in venous return but the COP is not increased. So, the heart is dilated to accommodate excess venous return increasing EDV which increase force of contraction i.e. it increases SV and COP.
Definition: it is the ability of the cardiac muscle to increase its force of contraction secondary to increase in the EDV (preload) causing increase in SV and COP.
Measurement of COP:
Echocardiography
Clinical use of echocardiography:
It is also used to calculate:
Cardiac output, ejection fraction, and diastolic function
Flow velocity and volume of blood through valves.
It provides helpful information about:
Location and extent of any tissue damage.
Pumping capacity of the heart.
Size and shape of the heart (internal chamber size quantification).
Definition of echocardiogram: it is a sonogram of the heart, it uses standard twodimensional, three-dimensional, and doppler ultrasound to create images of the heart.
Variations in COP:
Conditions decrease COP:
All conditions that destroy the cardiac muscle fibers.
Marked arrhythmia: (COP= SV x HR)
In bradycardia: although the SV is increased (e.g. 100 ml), it cannot compensate for the decreased HR (e.g. 40 beat/min) i.e. COP in this case will be 4 L/min (100 x 40) i.e. decreased COP
In tachycardia: due to shortening of the diastolic period in which cardiac filling occurs
Sitting or standing from lying down: decreases COP by 20 - 30% (due to pooling of blood in lower limbs with decreased venous return and COP). However, under normal condition, immediate compensation occurs by constriction of veins which increases venous return.
Conditions increase COP:
Pregnancy: due to an increase in uterine blood flow and placental arterio-venous shunt
Eating: in the first few hours after eating due to increase gastrointestinal (GIT) blood flow.
Exercise: can increase COP up to 700% in trained athletes
Exposure to extremes of temperature:
In very low temperature due to increase muscle tone which increases venous return.
In high temperature due to skin vasodilatation.
Excitement: increase COP by about 50 -100% due to sympathetic stimulation.
Cardiac index (CI)
Normal range: increased COP)
Calculation: if we consider the surface area of adult male weighted 70 Kg = 1.73 m2. So, cardiac index= COP/m2= 5/1.73= 3.2 L/min/m2.
Definition: cardiac output per square meter (m2) of body surface area.
Cardiac output (minute volume, COP)
Normal value: 5 L/min
Calculation: COP = SV x HR = 70 x 70.
Definition: it is the amount of blood (in liters) pumped by each ventricle in one minute.
Ejection fraction
Factors affecting (importance):
It decreases with increased aortic resistance and in heart failure.
It increases with increased contractility.
Normal value: 50-65%.
Definition: stroke volume / end diastole volume x 100 i.e. SV/EDV x 100
Stroke volume (SV)
Normal value: 70 ml.
Calculation: SV= EDV- ESV= 140-70= 70 ml.
Definition: it is the amount of blood pumped out by each ventricle per beat.
Heart rate (HR)
Normal value: 70-75 beat/min.
Definition: it is the number of heart beats per minute.
End systolic volume (ESV)
Normal value: 65-70 ml.
Definition: it is the volume of blood in the ventricle at the end of systole.
End diastolic volume (EDV)
Normal value: 135-140 ml.
Definition: it is the volume of blood in the ventricle at the end of diastole.
Conducting System of the Heart
This consists of
SA node (the pace maker)
AV node
A-V bundle of Hiss
Moderator Band (right branch)
It is formed of special type of cardiac muscle fibers called Purkinje fibers, surrounded by CT rich with blood capillaries.
Purkinje muscle fibers differ from the cardiac muscle fibers in:
with its two branches and their finer ramification
Regulation of Diameter of Arterioles
Factors regulate arteriolar diameter:
Systemic (central) regulation of diameter of arterioles:
Circulating vasoactive substances that regulate arteriolar diameter:
Circulating vasodilator substances:
Atrial natriuretic peptide (ANP):
It decreases renin release causes decrease angiotensin II formation.
ANP causes relaxation of mesangial cells of the glomeruli which increases glomerular filtration rate and sodium loss in urine.
It decreases vasopressin hormone secretion.
It decreases aldosterone secretion.
Actions of ANP: are opposite to action of angiotensin II i.e.
It causes natriuresis i.e. loss of Na+ in urine.
It has a VD effect as it decreases the response of the blood vessels to vasoconstrictor substances. Thus, it decreases blood pressure.
It decreased in rising from supine to erect position due to decreased venous return).
It is secreted when:
venous return is increased e.g. with immersion in water up to the neck.
blood volume is increased.
NaCl intake is increased.
intraventricular pressure is increased.
right atrial pressure is increased.
It is secreted from the atria, ventricles and brain.
Kinins
Actions of kinins:
Stimulation of pain receptors.
Positive chemotaxis effect (attract WBCs).
Contraction of smooth muscles as in respiratory system.
Increase capillary permeability.
Act as mediators for VD in active salivary glands.
VD by release of endothelium derived relaxing factor (NO) causing marked decrease in blood pressure.
Circulating vasoconstrictor substances:
Vasopressin (antidiuretic hormone, ADH):
The normal amount in blood doesn't affect the arterial pressure, but if its level increases, it will cause marked VC and increases the blood pressure. Thus, it plays important role in acute hemorrhage.
It acts on V1 receptors in vascular smooth muscle to increase Ca+2 concentration in smooth muscle fibers causing VC and increased blood pressure.
It acts on V2 receptors in the nephrons increasing cAMP which increases the permeability of the cells to water, urea, and some other solutes. Thus, it increases the extracellular fluid volume and arterial blood pressure.
It secreted by the posterior pituitary gland.
Renin-angiotensin system:
Decreased blood pressure (e.g. dehydration, salt restriction, hemorrhage) causes a reduction in renal blood flow which results in renal ischemia that stimulates the juxtaglomerular apparatus to secrete renin which acts on alpha globulin in the plasma called angiotensinogen producing angiotensin I which is converted to angiotensin II by the angiotensin convertase enzyme in the lung.
Effects of angiotensin II:
Stimulates thirst sensation which increases water intake resulting in an increase in blood volume and blood pressure.
Stimulates salt and water retention by the kidney which increases blood volume and blood pressure.
Stimulates aldosterone release from the suprarenal cortex which causes salt and water retention that results in an increase in blood volume, cardiac output and blood pressure.
Stimulates antidiuretic hormone (ADH, vasopressin) secretion from the posterior pituitary causes water retention VC and increase blood pressure.
Stimulates noradrenaline release from postganglionic sympathetic fibers which causes VC increasing peripheral resistance and blood pressure.
Has a strong direct arteriolar VC (50 times as noradrenaline) leading to increased peripheral resistance and blood pressure.
Catecholamines
Sympathetic stimulation causes release of adrenaline and nor-adrenaline which circulate in the blood and cause the same effects of the sympathetic nervous system on the arterioles i.e.
Adrenaline: in small doses causes VD of blood vessels in skeletal muscles and liver by acting on 2 adrenergic receptors.
Noradrenaline: has a potent VC effect on the blood vessels by stimulating alpha (α) adrenergic receptors.
Neuronal regulatory mechanisms:
Vasodilator fibers:
Antidromic vasodilator impulses:
When they reach the arterioles, they cause a release of substance P which has a VD effect on the arterioles thus, the area of inflammation become red (flare).
It is a local axon reflex i.e. stimulation of pain receptors initiates impulses travel along sensory nerve fibers toward central nervous system (CNS) until they reach a branch, they travel a long it (antidromically) i.e. it doesn’t involve the CNS
When pain receptors are stimulated by a painful stimulus as scratching the skin with a pin, dilatation of the adjacent blood vessels occurs.
Parasympathetic vasodilator fibers:
The parasympathetic fibers in the facial and glossopharyngeal nerves (7th and 9th cranial nerves) which supply the salivary glands produce VD indirectly by increasing metabolic activity of these glands during active secretion.
The only parasympathetic fibers which are definitely vasodilator are those which supply the genital organs (sacral outflow).
Sympathetic vasodilator fibers to:
The splanchnic areas: as the blood vessels of these areas are rich in beta () adrenergic receptors that produce VD.
Sweat glands: they are sympathetic cholinergic VD fibers that supply blood vessels of the sweat glands. Their activity is controlled by the heat loss center in the anterior hypothalamus, independent from the VMC.
Skeletal muscle blood vessels:
This system can be activated by sudden strong emotions which causes a widespread VD resulting in severe hypotension, brain ischemia and syncope.
They start to operate and dilate the skeletal muscle blood vessels even before the start of the exercise and so help to increase the skeletal muscle blood flow during exercise.
These fibers are not under the control of the VMC.
This system originates in the cerebral cortex and relays in the hypothalamus, then it passes through the medulla oblongata to the lateral horn cells of the thoraco-lumbar segments of the spinal cord and activates the sympathetic vasodilator fibers to skeletal muscle blood vessels.
They are cholinergic sympathetic fibers i.e. they secrete acetylcholine.
Coronary vessels: VD occurs indirectly by increasing heart rate and the metabolic activity of the heart which decreases PO2, tension and causes accumulation of metabolites.
Vasoconstrictor fibers:
Parasympathetic vasoconstrictor fibers:
Parasympathetic stimulation to the heart causes coronary VC indirectly by decreasing the metabolic activity that causes elevation of PO2.
No vasoconstrictor parasympathetic fibers are known.
Sympathetic vasoconstrictor fibers:
Vasoconstriction or vasodilatation is produced by increasing or decreasing the sympathetic neural activity which is determined by activity of the VMC i.e. stimulation of VMC increases the vasoconstrictor tone increasing the peripheral resistance and the arterial blood pressure and vice versa.
They discharge continuously, due to descending tonic excitation from the vasomotor center (VMC) in the medulla oblongata, leading to generalized partial vasoconstriction which is called sympathetic vasoconstrictor tone.
The sympathetic noradrenergic fibers arise from the lateral horn cells of the thoracolumbar segments of the spinal cord.
Local regulation of diameter of arterioles:
Substances released by the endothelium:
Endothelins:
Endothelium-derived-relaxing factor (EDRF):
Normally, erection in male genital organs occurs by VD.
Its deficiency as in cases of endothelium injury causes loss of its vasodilator effect and the vasoconstrictors as thromboxane A2 becomes predominant causing vasoconstriction, atherosclerosis, hypertension and impotence (failure of erection).
It is released by endothelium under the effect of bradykinin, substance P, vasoactive intestinal peptide (VIP) as a mediator for their vasodilator effects.
It is inhibited by methylene blue.
It increases cGMP causing VD.
It is identified as nitric oxide (NO) and is synthesized from arginine amino acid.
Actions of endothelins:
Positive inotropic effect on cardiac muscle.
Decrease renal blood flow and increase renal vascular resistance (potent VC).
Stimulate aldosterone and catecholamine release.
VC of the coronaries
Strong contraction of the vascular smooth muscles especially veins (the most potent one).
They are released by stretching the vessels.
They are of four types and have two types of receptors in the vascular walls.
Prostacyclin and thromboxane A2:
Both are in balance with each other in control of vascular diameter and platelet plug formation.
Both are formed from arachidonic acid by cyclooxygenase enzyme.
Thromboxane A2: is released from platelets and causes VC and increase platelet aggregation.
Prostacyclin: is released from endothelium, causes VD and inhibition of platelets aggregation.
Local temperature: drop in the tissue temperature has a direct VC effect, while increase in its temperature causes VD.
Local vasoconstrictor substances: injured arteries and arterioles constrict powerfully due to serotonin release from blood platelets.
Intrinsic mechanism (autoregulation):
Metabolic theory: if the blood flow to an organ is decreased, vasodilator metabolites accumulate producing vasodilatation which will increase the blood flow to wash the metabolites and remove their effect.
Myogenic theory: when the blood flow increases to a tissue, it causes stretching the vascular smooth muscles resulting in their depolarization and vascular smooth muscle contraction that decreased the blood flow to normal.
Definition: it is the ability of a tissue to regulate its blood flow according to its need.
It is well developed in kidneys, liver, myocardium and brain.
Most of vascular beds have this capacity.
Metabolites
When the tissue becomes hyperactive, some metabolic changes occur as increased CO2 tension (PCO2), acidosis, osmolality, K+, and adenosine which in turn cause VD in systemic arterioles i.e. active hyperemia.
Reactive hyperemia: increase in blood flow of a tissue produced by accumulation of metabolites due to temporary occlusion of its blood supply.
Active hyperemia: increase in blood flow at the active tissues by vasodilation produced by accumulation of metabolites
O2 tension (PO2):
When the metabolic activity of a tissue decreases, PO2 is increased leading to VC. The opposite occurs with the increase in the tissue metabolic activity i.e. if the metabolic activity of a tissue is increased, PO2 is decreased leading to VD.
O2 lack is the most potent vasodilator in the heart, while CO2 excess is the most potent vasodilator inside the central nervous system
Decreased PO2 leads to a direct vasodilator effect on the arteriolar smooth muscles (except for the pulmonary vessels which constrict due to O2 lack).
The normal PO2 produces partial VC and this is maintained by the sympathetic vasoconstrictor tone.
PO2 is also known as the partial pressure of oxygen and it represents the activity of the molecules of oxygen dissolved in the plasma.
Functions of arterioles:
They control blood flow to the tissues: by changing their diameter through producing VD or VC, as they have a smooth muscle layer.
Determination of the peripheral resistance: they are called the resistance vessels because they control the peripheral resistance and the arterial blood vessels.
Characters of arterioles:
The only site at which arterioles can be seen is the retina.
The endothelium in their walls can synthesize chemical mediators that cause constriction or dilatation o their walls.
They are sensitive to chemicals of blood as the blood gases, hormones, metabolites and pH.
They have sympathetic vasoconstrictor (VC) fibers and some parasympathetic vasodilator (VD) fibers.
In comparison to arteries, arterioles:
have a greater resistance to blood flow (so the blood pressure drops from 80 to 30 mmHg) and act as sphincters between arterial and venous systems.
lost elastic elements, while a smooth muscle layer is present.
Definition: arterioles are the terminal branches of the arterial system.
Coronary Blood Flow
Regulation of coronary blood flow (CBF):
Mechanical factors controlling CBF:
the coronary blood flow is markedly affected by the mechanical events during the cardiac cycle.
The coronary blood flow is controlled by the MAP in aorta, so a decrease in aortic pressure (e.g. in shock or in aortic stenosis) leads to a decrease in the CBF
Blood flow in the coronary arteries occurs mainly during diastole, so any pathological condition which increases the HR markedly shortens the diastolic period of the ventricles and decreases the coronary flow e.g. paroxysmal tachycardia.
In the right coronary: there are similar changes also occur, but they are milder because the force of contraction is much weaker in the thinner right ventricle and the blood flow in the right coronary artery increases towards the end of systole, but maximum inflow is reached also in early diastole.
In left coronary artery: the coronary blood flow follows the aortic pressure i.e.
Then, the CBF gradually decreases as the aortic pressure is gradually decreased.
In the isometric relaxation phase, maximum CBF occurs as:
The cardiac muscle fibers relax.
The aortic pressure is relatively still high.
In reduced ejection phase, CBF is decreased again due to decrease of aortic pressure.
In the maximum ejection phase, CBF is gradually increased due to rise of the aortic pressure (which pushes some blood in the coronary artery in spite of the compressing effect of the contraction muscle).
In the isometric contraction phase, CBF is markedly decreased due to:
Low aortic pressure.
Mechanical compression of the coronary vessels.
Chemicals, hormones and drugs controlling CBF:
Coronary VC substances: antidiuretic hormone (ADH, vasopressin) and angiotensin II.
Coronary VD substances: thyroxine, adrenaline, ADP, caffeine, alcohol, nitrites and EDRF (NO).
Chemical factors controlling CBF (autoregulation, intrinsic mechanism):
When the cardiac work is decreased, there is coronary VC.
When the cardiac work increases, the blood flow is increased and vice versa.
The most effective vasodilator is hypoxia of the cardiac muscle which produces coronary vasodilatation through:
Release of chemical substances most probably adenosine (the greatest vasodilator substance).
Direct effect on the coronary blood vessels.
As the cardiac work increase e.g. during muscular exercise, there is hypoxia, increase CO2, H+, K+, lactate and other metabolites.
It is independent on neural control i.e. it can be observed in the denervated (transplanted) heart.
Neural factors controlling CBF:
Effect of parasympathetic (vagal) stimulation on CBF:
Direct effect: acetylcholine released at the vagal nerve ending produces slight VD on the coronary vessels.
Indirect effect: a decrease in HR, force of contraction and reduction of CBF which is secondary to a decrease in the cardiac work and metabolism.
Effect of sympathetic nervous system:
Indirect effect (dominant): an increase in HR, force of contractions and marked increase in myocardial work lead to accumulation of metabolites, that causes marked VD effect on the coronary blood vessels.
Stimulation of sympathetic nervous to the heart leads to:
Cardiac oxygen extraction:
In other body tissues, the venous blood contains 14 ml O2% i.e. only 5 ml O2 are extracted.
During rest: it is about 70-80% O2 in each unit of blood. The arterial blood contains 19 ml O2% and the coronary venous blood contains 5 ml O2% i.e. 14 ml O2 are extracted from every 100 ml blood. So, the cardiac O2 consumption can be increased significantly only by increasing the coronary blood flow.
Normal value for coronary blood flow:
During exercise: coronary blood flow is increased about 3-5 folds that of normal resting level and in athletic person may reach up to 600 ml /100 gm heart weight/min.
The right ventricle receives about 2/3 the blood flow to the left ventricle.
During rest: it is about 80 ml /100gm of the heart /min i.e. 250 ml/min i.e. 5% of cardiac output.
Physio 1
Cardiac Reserve
Mechanisms of cardiac reserve:
Hypertrophy of the cardiac muscle:
When the work done by the heart is increased for a long period of time as in arterial hypertension, hypertrophy of the cardiac muscle takes place which increases the force of ventricular contraction.
Limitations: hypertrophy of the cardiac muscle is not accompanied by a simultaneous increase in the number of the capillaries which supply the cardiac muscle fibre, resulting in hypoxia of the cardiac muscle. Thus, the force of ventricular contraction decreases.
Increased SV:
Limitation: above the physiological limit, increased EDV decreases the force of contraction which decreases the SV. Moreover marked dilatation of ventricle causes incompetent AV valves which decreases the COP.
It may be increased from 70 ml to a maximum of 200 ml (3 folds the normal).
Increased HR:
Limitation: marked increase in HR shortens the time for ventricular filling and for the main coronary flow which decreases the COP.
It may be increased from 70 to a maximum 160 - 200 beats/minutes. Thus, increasing the COP by 3 folds its normal provided that the VR is adequate
Variations in cardiac reserve:
In heart failure: there is no reserve at all i.e. zero.
In elderly asthenic person: it may be as low as 200%.
Normal value of cardiac reserve: it is expressed as percent of normal i.e.
In athletes trained person: 500 - 700%.
In normal young adult: 300 - 400%.
Definition: it is the difference between cardiac work during maximum exercise and cardiac work during rest.
Mechanical Efficiency (ME)
Variations in ME:
In hypertension and aortic stenosis, the work of heart is increased, the oxygen requirement are much increased. So, ME is decreased and early heart failure occurs.
In aortic regurge, SV is increased without much increase in O2 consumption and so ME is increased and so early heart failure is rare.
The increase of work by increasing the MAP (COP constant) is accompanied by increased O2 utilization in proportion to increased work. So, ME is not changed.
ME is increased by increasing the work done. So, it is increased by increasing either the COP (SV x HR) or MAP.
The rest of energy expenditure is lost as heat.
ME may be as low as 3% in heart failure and as high as 30% in well-trained athletes.
Calculation of normal ME:
So, ME = work done/total energy expenditure = 1/5 x100= 20%.
The heart consumes at rest one liter O2/hr which yeilds 5 calories (energy expenditure).
The useful work done by the heart = total work of the heart (kg-m/min) x 60= 7.14 x 60= 428.4 Kg-m/hr = 1 calory (calory = 426 kg-m/hr).
Normal value of ME: 20%.
Definition: it is the useful work done expressed as a percentage of the total energy expenditure.
MAP=mean atrial pressure
Circulatory Shock
Prognosis of shock:
Circulatory shock is classified according to its prognosis into:
Irreversible (refractory) shock: occurs in severe cases of shock and when the patients are not treated for about 3-5 hours causing progressive decrease in COP and ABP in a positive feedback mechanism
Mechanisms that lead to death in refractory shock:
Acute renal failure: due to;
Muscular tissue damage which causes accumulation of myoglobin that enhances the damage in the kidney tissue with decrease renal plasma flow and glomerular filtration rate. The renal functions are severely impaired with uremia and anuria.
Severe renal VC that causes renal ischemia and tubular necrosis.
Acute respiratory failure:
due to damage of capillary endothelium and alveolar epithelium in the lung with release of cytokines.
Metabolic acidosis:
decreased O2 supply causes lactic acid accumulation and also increased CO2 increases H2CO3. This acidosis leads to tissue damage and activation of intracellular proteolytic enzymes with auto-destruction.
Thrombosis of small vessels: .
due to sluggish circulation with activation of clotting factors and platelet aggregation. This leads to more tissue ischemia
Release of toxins by ischemic tissues:
Free radicals: decrease in COP causes tissue hypoxia that results in injury of vessels causing adherence of granulocytes to vessels releasing free radicals which causes more damage of vessels and more adherence of granulocytes and release of more free radicals and so on.
Endotoxin: released from intestinal bacteria under ischemia is absorbed to blood causing severe VD and cardiac depression causing severe shock.
Myocardial toxic factor: extreme pancreatic ischemia causes a release of trypsin enzyme from pancreas causing degeneration of pancreatic tissue with release of myocardial toxic factor that causes a direct depression of the heart contractility.
Dilatation of precapillary sphincter:
Mechanism: hemorrhage causes reflex sympathetic spasm of precapillary sphincters and venules especially in splanchnic area after that dilatation of precapillary sphincter occurs by metabolites or toxins but venules remaining constricted which results in:
an increase in capillary filtration increasing loss of plasma in tissue space decreasing blood volume that results in a decrease in VR decreasing COP and causes ischemia of the capillary wall and more filtration
a decrease in VR with more decrease in ABP and more spasm of venules causing more decrease in ABP.
Cerebral depression:
Mechanism: severe decrease in ABP decreases cerebral blood flow causing depression of vasomotor center with no correction of decreased ABP causing more decrease in ABP causing cerebral damage.
Cardiac depression:
Mechanism:
Myocardial toxic factor (or other bacterial toxins) released during shock.
Severe decrease in ABP causes a decrease in coronary blood flow resulting in myocardial ischemia which decreases cardiac contraction decreasing COP and ABP causing myocardial infarction.
Reversible (compensated) shock: immediate and delayed hemorrhage compensatory mechanisms gradually restore the normal ABP in a negative feedback control.
Severity of circulatory shock depends up on both degree and rate of the drop in the ABP.
Types and causes of circulatory shock:
Obstructive shock: due to obstruction of the blood flow at the center of circulation which hinders blood flow to tissue e.g.
In the heart: as in cardiac tamponade (massive pericardial effusion) with fibrosis which prevent cardiac filling and contraction.
In the lung: as in cases of the pulmonary embolism, thrombosis, and tension pneumothorax with marked elevation of the intrathoracic pressure.
Cardiogenic shock: as in infarction, heart failure or arrhythmia.
Treatment:
IV infusion of dobutamine
It does not stimulate dopaminergic receptors.
The drug increases cardiac output and does not significantly elevates oxygen demands of the heart, a major advantage over other sympathomimetic drugs. It is given by IV infusion 2.5-10 ug/kg min. (ug= micro gram = 0.000001 gram)
Dobutamine is a selective β1 agonist increasing cardiac contractility with minimal increase in heart rate.
treatment of the cause
Dysrhythmia
Myocarditis
Massive pulmonary embolism
Myocardial infarction
Hypovolemic (cold, secondary) shock
Dopamine 2-5uglkglmin → vasodilatation of renal blood vessels [++D1 receptors] → protect from renal hypoperfusion and renal failure. The rate of dopamine infusion can be increased according to patient hemodynamic state. But correction of hypovolemia must be done before dopamine infusion.
Volume replacement [blood, plasma or fluids].
dehydration
Loss of fluids as in severe vomiting and diarrhea.
trauma
Loss of plasma as in burn.
Hemorrhage
Types of hemorrhage:
According to prognosis of hemorrhage:
Compensated 20% loss hemorrhage
According to onset of bleeding:
chronic
Acute
According to site of bleeding:
interstitial
internal
External
Definition: it is the loss of blood from the cardiovascular system.
Characters: blood volume is decreased secondary to loss of blood or plasma or extracellular fluid.
Normovolemic (low-resistance, primary) shock:
Septic shock:
Monoclonal antibodies against bacterial endotoxins.
Dopamine by IV infusion.
Corticosteroids e.g. dexamethasone
In addition, by favoring sodium and water accumulation in blood vessels’ wall, corticosteroid will contribute to increase systemic vascular resistance.
Corticosteroids cause rise in blood pressure: • by enhancing the vasoconstrictor action of adrenergic stimuli on small vessels via increasing the sensitivity to alpha agonist leading to increase in mean arterial pressure and systemic vascular resistance.
Corticosteroids induce sodium retention via both mineralocorticoid and glucocorticoid receptors. Thereby, contribute to correct the hypovolemia that characterizes the early phase of sepsis.
Corticosteroids restore cardiovascular homeostasis, terminate systemic and tissue inflammation, restore organ function, and prevent death in sepsis.
Full doses of bactericidal specific antibiotics
Caused by gram-negative and sometimes gram-positive bacterial infection → release of endotoxins that mediate vasodilatation. In severe infection, bacterial endotoxins depress the vasomotor center causing VD of arterioles and capillaries increasing capillary permeability and decreasing ABP progressively causing shock.
Anaphylactic shock
Antihistaminic IV.
Antihistaminics act by reversible competitive antagonism to histamine on H1- receptors, producing:
Hydrocortisone or prednisolone IV.
Glucocorticoids can dramatically reduce the inflammatory response and to suppress immunity, through:
Glucocorticoids stabilize mast cells and basophile membranes thus, interfering with mast cell degranulation resulting in decreased histamine release and capillary permeability.
COX-2 synthesis in inflammatory cells is reduced, lowering the availability of prostaglandins.
Indirect inhibition of phospholipaseA2 (due to the steroid-mediated elevation of lipocortin), thus blocks the release of arachidonic acid, the precursor of the inflammatory mediators prostaglandins and leukotrienes from membrane- bound phospholipids.
Complete antagonism of histamine-induced contraction on GIT and bronchi. Partial antagonism of histamine on C.V.S.
Antiallergic effect.
Adrenaline IM.
Adrenaline which is life-saving in anaphylaxis is a Physiological antagonist to histamine (the main mediator in anaphylaxis) Physiological antagonism: Adrenaline induces bronchodilatation (β2) opposes Histamine induced bronchoconstriction (H1).
Definition : with release of histamine (or kinin) causing VD with drop in ABP
exaggerated antigen-antibody reaction (Hypersensitivity reaction to an antigen for example [penicillin]) → release of mediators [histamine (or kinin) , leukotrienes, PGs…] severe vasodilatation--> drop in ABP (arterial blood pressure) → shock
Neurogenic shock: .
In case of severe pain, morphine can be given [10mg i.v.]
Vasopressor Sympathomimetics as:
Ephedrine [25mg i.v.] or Dopamine by i.v. infusion [10 up to 50 μg/kg/min].
Pharmacological actions of dopamine:
High rate of infusion of dopamine [>10µg/kg/min] stimulates α1adrenoceptors causing vasoconstriction with increased in blood pressure.
Moderate rate of infusion [5-10µg/kg/min]: dopamine stimulates β1adrenoceptors causing positive inotropic and chronotropic effects lead to increase cardiac output.
Slow rate of infusion [2- 5µg/kg/min]: dopamine stimulates D1 receptors in renal, splanchnic, coronary and cerebral circulation → VD in the renal vasculature. D1 receptor activation increases renal blood flow and urine output.
Position of the patient: recumbent with elevation of the lower limbs to prevent pooling of blood into the lower half of the body and to attain good perfusion of vital of organs.
Pain or anxiety.
severe emotions cause vaso-vagal syncope i.e. VD of skeletal muscle blood vessels, bradycardia and decrease ABP progressively causing shock
Spinal anesthesia → decreased sympathetic activity → V.D. → drop of BP.
Characters: blood volume is normal, but there is marked VD.
Definition: it is inadequate tissue perfusion with blood due to the progressive decrease in COP and ABP.
Properties of Cardiac Muscle
Contractility
Factors affecting contractility :
Factors that increase the strength of contraction are called + ve inotropic factors, however that decrease the strength of contraction are called -ve inotropic factors:
Mechanical factors :
Force-frequency relationship:
Studied on the papillary muscles, show that the force of myocardial contractility is affected by the time interval between the cardiac impulses.
Beat loss:
Following an interval of constant frequency of beats if an impulse is absent ,the following contraction after this period of rest becomes more powerful.
Extrasystole: .
Following an interval of constant frequency, if an impulse comes early, it causes a weak contraction called extrasystole then followed by stronger contraction than normal (called post-extrasystole) then return to normal
Staircase (or treppe ) phenomenon
When the isolated heart is stimulated by successive maximal stimuli (constant). The first few contractions show gradual increase in magnitude.
Explanation
The increase in contractility is due to :
Increase in the warmth --> increases the rate of metabolic processes and chemical reactions.
Bring out of K+ from the cell producing optimal environment for contraction.
Increase the availability of Ca++ inside cytoplasm.
Force - velocity relationship :
However, as a rule, within limits an increase in either pre- or afterload will increase the force of contraction. e.g. The cardiac muscle contraction increases by increase in venous return (preload) and with hypertension (by increase afterload).
The velocity of contraction is inversely proportional يتناسب طردياto after load and directly proportional يتناسب عكسياwith preload.
After load: means the force which act on the muscle after its beginning of contraction and resist the contraction and decreases its velocity .In the heart the increase in the mean aortic pressure opposes the contraction power of the ventricle.
Pre-load: means the force which stretch the muscle fibers and increase its length before contraction and is lifted by contraction. In the heart the preload force is the amount of blood returns to the heart and fill the ventricle at end of diastole period (end diastolic volume).
Length - tension relationship (Starling law) :
Starling law states that “The force of contraction of the cardiac muscle is directly proportional to the initial length of the cardiac muscle fiber within limit” (i.e. the greater the initial length of the cardiac muscle fiber, the stronger will be the force of its contraction, however, over stretch decrease its power of contraction (as in heart failure).
Starling low can be explained by the finding that proper stretch of the cardiac muscles make more heads of myosin come in contact with active sites of actin.
Initial length of cardiac muscle fibers is determined by the degree of diastolic filling.
The cardiac muscle cannot be tetanized
N.B.: If tetany occurs in the cardiac muscle, the pumping action of the heart would stop leading to circulatory failure and death.
This is due to long absolute refractory period ARP in the cardiac muscle during which its excitability is completely lost.
ARP ends by the end of systole, and first part of diastole. So, the heart must be relaxed before it can be re-stimulated .
All or non rule (law) :
N.B. :
The tissues that obey the law are ( atria, ventricles , single muscle fiber , single nerve fiber and the motor unit).
This does not mean that the force of contraction of cardiac muscle is fixed, but it can be increased or decreased by neural, humoral or mechanical factors (i.e. If the conditions are changed the strength of contraction will be changed).
This property makes the heart an efficient pump.
This is because the cardiac muscle acts as a functional syncytium as one unit.
It states that “Stimuli causes the cardiac muscle contracts maximally or does not contract at all, provided that all factors affecting contraction are kept constant”.
Sever O2 lack and Co2 excess → decrease the force of contraction (-ve inotropic effect).
Effect of extracellular ions :
N.B. : Intravenous injection of Ca++ should he very slowly otherwise the heart will be stopped in the systole (irreversible contraction of the heart).
K+ : Increase in K+ more than 3 times decreases the power of contraction due to delay in conduction in cardiac muscle and may stop the heart during diastole. Also decrease K+ leads to weak contraction due to the associated hyperpolarization or may has no effect.
Ca++: -Increase Ca++ leads to increase power of contraction and causes Ca++ rigor which may stop the heart during systole. -Decrease Ca++ causes decrease contractility.
Na+: decrease Na+ lead to decrease amplitude of action potential with less contraction
Chemical factors and drugs
Cholinergic drugs, ether, chloroform and some bacterial toxins → decrease the heart contractility (-ve inotropic).
Catecholamine (epinephrine), thyroxin, cortisol, glucagon and digitalis → increase the heart contractility (+ve inotropic).
pH
Excess alkalosis or acidosis→ has a - ve inotropic effect and may stop the heart in diastole
Moderate acidosis → has - ve inotropic effect.
Moderate alkalosis → has a +ve inotropic effect.
Nervous factors :
Parasympathetic (vagal) stimulation (or acetyl choline) produces-ve inotropic effect on the atrial only (it does not supply the ventricles i.e. vagal escape phenomenon) by decrease Ca++ influx in cardiac muscles.
Sympathetic stimulation (or adrenaline) produces +ve inotropic effect on both atria and ventricles (because it leads to an increase in Ca++ influx in the cardiac muscle fibers).
Physical factors : -
Cooling (or excessive warming) → decrease contractility.
Moderate warming → increase the contractility.
Excitation - contraction coupling:
This in turn produces the muscle contraction, while muscle relaxation occurs as result of active Ca++ reuptake by the sarcoplasmic reticulum.
Then Ca++ diffuse into the myofibrils and catalyze the chemical reactions that promote sliding of the actin and myosin filaments along each others.
The T tubules action potentials in turn act on the membranes of the longitudinal sarcoplasmic tubules to cause release of very large quantities of Ca++ into the muscle sarcoplasm from sarcoplasmic reticulum. Also Ca++ diffuses from the extracellular fluid
When the excitatory impulses reach the cell membrane of the cardiac muscle fibers, they will propagate into the interior of the cardiac muscle fibers along the membranes of the T tubules
Definition : It is the ability of the heart to contract and pump the blood against the peripheral resistance. It contract both isotonically (with decrease in its length) and isometrically (with increase in its tone).
Conductivity
factors affect conductivity are the same ones that affect rythmicity (page16) .
conductivity is measured by P-R interval in the ECG and a-c interval in jugular venous pulse wave.
The conductive system of the heart:
The purkinje system
Importance: to conduct the impulse to whole ventricles at the same time and causes good ventricular pump.
cause: the very rapid junction’s transmission via the ionic gap with low ionic resistance
The branches of the AV bundle are divided into many branches to penetrate the ventricular muscles and continue with its fibres. -The rate of conduction in AV bundle & purkinji fibres is the highest rate =4m/sec.
A-V bundle (bundle of Hiss):
It is divided into right & left branches which run in the interventricular septum to ventricles.
It is the only connection between atria and ventricles
AVN (Atrio-ventricular node):
Rate of conduction is the slowest rate = 0.2 m/sec.
Importance: The AV nodal delay of conduction (0.13sec.) is important to:
Protect the ventricle from high atrial abnormal rhythm as AV node can’t conduct more than 150-200 impulses/minute.
delay start of ventricular contraction till the end of atrial contraction and complete evacuation of blood into ventricle.
cause: prolonged refractory period of its fibres due to opening of slow Na+ channels only and inactive Na+ fast channels due to the low negativity of its potential(-55)
Its lower part forms the penetrating portion of A-V bundle.
Its upper part is connected to the internodal pathways by transitional fibres.
It is located near tricuspid valve.
Internodal pathways:
It is 3 bundles (anterior,middle & posterior) from SAN to AVN. with conduction rate of 1m/sec.(atrial muscle itself has conduction rate of 0.4 m/sec.
Bachman’s bundle
it is interatrial tract from SAN to left atrium with conduction rate of 1meter/second.
S.A.N
located on the posterior wall of right atrium and arise from in the sinus rhythm.
Definition: It is the ability of the cardiac muscle to conduct the excitation wave from S.A.N to all parts of the heart.
Cardiac Rhythmicity (Automaticity)
Difference between ventricular and pace maker action
Factors affecting rhythmicity (chronotropic effect):
Other factors affect rhythmicity:
Effect of ischemia and bacterial toxins: they decrease rhythmicity.
Effect of changes in blood gases: severe O2 lack or CO excess decreases rhythmicity.
Effect of blood pH:
Excessive changes in pH: causes cardiac arrhythmias due to ionic disturbances.
Moderate changes in pH: direct relation with rhythmicity i.e.
Acidosis: increases blood Ca++ decreasing rhythmicity.
Alkalosis: decreases blood Ca++ increasing rhythmicity.
Effect of drugs:
Cholinergic drugs: decrease rhythmicity.
Digitalis: decreases rhythmicity and conductivity as it depresses the nodal tissue and produces an effect like that of vagus nerve stimulation particularly on the AV node.
Digitalis is used in treatment of heart failure as it increases the myocardial contractility (positive inotropic) and decreases rhythmicity (negative chronotropic).
Effect of extracellular ions:
Decrease K+: shortens the slope of the prepotentials increasing rhythmicity.
Excess K+: prolongs the slope of prepotentials decreasing rhythmicity and weakens the myocardial contractility and may stop the heart in diastole i.e. K+ rigor.
Ca++: inverse relation with rhythmicity
Decrease Ca++: increases rhythmicity. B. K+: inverse relation with rhythmicity i.e.
Excess Ca++: decreases rhythmicity and strengthen the myocardial contractility, favoring systole and may leads to stoppage of the heart in systole i.e. Ca++ rigor.
Effect of body temperature:
Excessive warming or cooling decreases rhythmicity.
Moderate warming (fever): increases metabolic activity of SA node (direct effect) shortens the slope of prepotentials increasing rhythmicity.
Hormones: as thyroxine and catecholamines (adrenaline and noradrenaline) increase rhythmicity (as they increase metabolism) i.e. they have a positive chronotropic effect.
Pacemaker potential:
importance of prepotential:
The rapidity (shortening) of the slope of prepotential depends on
Ca++ influx
any factor decreases Ca++ influx as calcium channels blocker (verapamil) decreases the heart rate.
K+ efflux:
any factor increases K+ permeability (efflux) prolongates and delay up the slope of prepotential, decreasing heart rate.
The rate of slope (the speed with which it is reached to the firing level of prepotential) determines the heart rate i.e. the more rapid is the slope (e.g. for SA node), the more will be the heart rate.
It is the cause of rhythmicity (automaticity).
Diastolic prepotential of the SA node:
Differences between ventricular and pace maker action potentials:
Repolarization is due to the opening of K+ channels.
Once the firing level is reached (about -40 mV), opening of L–type Ca2+ channels (long acting type) occurs and depolarization is produced.
Cause of depolarization and repolarization:
Definition: spontaneous slow diastolic depolarization.
Resting membrane potential (RMP) of the SA node
Cause of unstable RMP of SA node:
Opening of the T-type (transient type) Ca2+ channels.
Leakage of Na+ through slow Na+ channels.
Decreased K+ efflux (end of repolarization of previous action potential) by closure of K+ channels.
is -55 to -60 mV (unstable).
Idioventricular rhythm: is 20-40/min (of ventricles) occurs if SA node and AV node are damaged or over inhibited by vagal stimulation.
Cardiac impulses initiated by other specialized cardiac cells: AV node rhythm is 60/min, Purkinje fiber rhythm is 30/min, and ventricular muscle rhythm is 20-40/min.
SA node is the normal cardiac pace maker as it has the highest rhythm (90-110/min) and the rest of the heart obeys it.
Cause of automaticity of cardiac muscle: presence of specialized self-excitable fibers that can initiate cardiac impulses
Definition: it is the ability of the cardiac muscle to initiate its own impulses regularly spontaneously i.e. independent of any nerve supply i.e. myogenic property i.e. heart beating continues even if heart is removed from the body.
Cardiac Excitability
Excitability includes
resting membrane potential RMP
Factors affecting cardiac muscle excitability:
Other factors affect cardiac muscle excitability:
Effect of blood pH changes on cardiac excitability:
Normal blood pH is 7.35-7.45.
Severe changes in blood pH decrease cardiac excitability.
Moderate changes in pH:
moderate acidosis increases blood Ca++ decreasing excitability.
moderate alkalosis decreases blood Ca++ increasing excitability
Decrease of cardiac metabolic processes decreases excitability as in:
Affection by bacterial toxins.
Hypoxia: decrease in O2 supply to the heart.
Ischemia: decrease in blood supply to the heart.
Drugs e.g. caffeine increases excitability.
Effect of changes in body temperature on cardiac muscle excitability:
Severe cooling or heating cause loss of cardiac muscle excitability.
Mild and moderate increase in body temperature (as in fever) increase metabolic process of cell increasing cardiac muscle excitability.
Effect of ionic changes on cardiac muscle excitability:
K+
Low K+ in the extracellular fluid increases K+ efflux (by its concentration gradient) increasing RMP hyperpolarization decreasing cardiac excitability.
Excess K+ in the extracellular fluid decreases K+ efflux decreasing RMP causing partial depolarization increasing cardiac excitability.
Ca++
Ca++: interferes with Na+ influx as there is competition between Na+ and Ca++ i.e. inverse relation between Ca++ and excitability i.e.
Low Ca++ increases excitability.
Excess Ca++ decreases the cardiac excitability.
Na+
Low Na+ in the extracellular fluid reduces the amplitude of the action potential (deficient depolarization) decreasing the cardiac excitability.
Excess Na+ in the extracellular fluid has no effect on excitability.
Hormones e.g. thyroxine increases excitability.
Autonomic nervous system:
Sympathetic stimulation: increases excitability
Vagal stimulation: decreases excitability.
Relation between
action potential (electrical response) of ventricular muscle fiber:
And
mechanical response
Excitability changes during action potential:
Positive after potential (after hyperpolarization):
Negative after potential (after depolarization, supernormal phase, vulnerable period, dangerous period):
Relative refractory period (RRP):
Absolute (effective) refractory period (ARP, ERP):
The duration of action potential of atrial fibers lasts about 150 msec (short plateau), while that of ventricular and Purkinje fibers last about 300 msec (long plateau).
Action potential of a ventricular muscle fiber:
Phases and ionic basis of the ventricular action potential:
4. Returning to the resting membrane potential (phase 4):
3. Late rapid repolarization (phase 3):
due to closure of Ca2+ channels and K+ efflux through slow K+ channel.
2. Prolonged plateau (phase 2):
Mechanism: the voltage gated L-type Ca2+ channels produce inward current. So, they maintain prolonged period of depolarization causing plateau in the action potential. The flow of Ca2+ ions into the cell just balances the flow of K+ out of the cell and keeps the membrane at the plateau level.
Cause: the slow but prolonged opening of the voltage gated L-type Ca2+ channels (L = long lasting).
Description: repolarization slows down forming a plateau, during which the membrane potential is near 0 mV.
1. Initial rapid repolarization (rapid small repolarization, phase 1):
The membrane potential changes from +20 to about zero mV.
is caused by )
Also, Cl- influx occurs.
closure of Na+ channels and opening of transient outward K+ channels (K+ efflux
0. Depolarization (initial rapid depolarization and the overshoot, phase
Mechanism: stimulation of the cell membrane by an adequate stimulus causes Na+ influx (entry) which depolarizes the cell and sustains the opening of more Na+ channels in a positive feedback manner.
Na channels include
slow (for Na+ and Ca++, open during plateau and blocked by calcium channel blockers as verapamil) channels.
Ca++ enters the myocardial cells is needed for myocardial contraction
Catecholamines and sympathetic stimulation increase the opening of the slow Na+ channels (not the fast Na+ channels) leading to an increase in the force of myocardial contraction.
fast (for Na+ only, open during rapid depolarization and blocked by tetrodotoxin)
Fast Na+ channel has an outer gate which opens at the start of depolarization and an inner gate that when closes, prevents further Na+ influx.
Cause: opening of fast voltage gated Na+ channels.
Description: it forms the rapid ascending limb of the action potential till reaching the reversal of polarity (overshoot) i.e. +20 mV.
action potential.
Causes (ionic basis) of RMP of a cardiac muscle:
Na+/K+ pump:
Mechanism: it is an electrogenic pump i.e. 3 Na+ are pumped to the outside of the membrane and 2 K+ are pumped to the inside.
It keeps more sodium extracellularly and more potassium intracellularly.
Unequal distribution of ions across the cell membrane by:
Donnan's effect: presence of a non-diffusible anion (protein) on the inner side of the cell membrane causes redistribution of diffusible ions till equilibrium occurs.
Selective permeability of the membrane (ionic leakage channels):
As the membrane is more permeable to K+ than Na+, K+ will diffuse from inside to outside along the concentration gradient.
There is a high concentration of Na+ outside and a high concentration of K+ inside the cardiac muscle fiber.
RMP for the conductive tissue in the heart is -90 to -100 mV.
Normal value of RMP of a cardiac muscle: -90 mV (from -80 to 95 mV) i.e. the potential difference during rest between intracellular fluid (ICF) and extracellular fluid (ECF) across the membrane of cardiac muscle is 90 mv with interior negative in relation to exterior.
Definition: it is the ability of the cardiac muscle to respond to an adequate stimulus (of strength and duration) by generating a propagating action potential followed by contraction.
The pericardium
Applied anatomy:
N. B. Bare area of the pericardium: - It is the area of the pericardium not covered by lung and pleura. It lies opposite the Anterior ends of the left 4th and 5th intercostal spaces where the left lung and the left pleura deviate laterally to form the cardiac notch.
Pus (pyopericardium).
Pericardiocentesis: a needle is introduced vertically into the pericardial cavity through the bare area of the pericardium to aspirate Excess fluid.
Air (pneumopericardium)
Blood (hemopericardium)
Excess serous fluid >50ml (hydropericardium).
In certain diseases the pericardial cavity may contain:
Blood and nerve supply of pericardium
Nerve supply of the pericardium
N.B. Pain of pericarditis originates from parietal pericardium
The visceral layer of serous pericardium is supplied by branches of sympathetic trunks and vagus nerves (autonomic nerve fibres). It is insensitive to pain.
The fibrous pericardium and parietal layer of serous pericardium are supplied by the phrenic nerves (somatic nerve). They are sensitive to pain.
Blood supply of the pericardium
The visceral layer of serous pericardium is supplied by the coronary arteries.
The fibrous pericardium and parietal layer of serous pericardium are supplied by branches of the following arteries:
Musculophrenic arteries.
Internal thoracic artery.
Sinuses of the pericardium:
Oblique sinus.
The Oblique sinus permits the distension of the left atrium during return of oxygenated blood from the lungs.
On each side
upper and lower left pulmonary veins (left side).
upper and lower right pulmonary veins and IVC (right side).
Inferior: (opening of sinus) the sac is continuous with rest of pericardial cavity between IVC and lower left pulmonary vein
Superior: reflection of visceral pericardium to become parietal from back of the left atrium at level of upper pulmonary veins.
Posterior: parietal pericardium and structure in posterior mediastinum (esophagus and descending thoracic aorta).
Anterior: back of left atrium and covering visceral pericardium
Oplique sinus is a recess of serous pericardium behind left atrium separating it from esophagus and descending thoracic aorta.
Transverse sinus.
Importance: allow distention of great vessels during systole and the atria during diastole.
Boundaries:
Inferior: reflection of visceral pericardium on the back of the great vessels from front of the atria
Superior: right pulmonary artery
Posterior: 2 atria and superior vena cava
Anterior: ascending aorta and pulmonary trunk
Formation: it is formed by reflection of visceral pericardium from front of 2 atria on the back of ascending aorta and the pulmonary trunk.
Transverse sinus is a Pericardial recess formed by visceral layer of pericardium.
Subdivisions
The pericardium consists of two components:
Serous pericardium: inner double layered (serous sac).
It represents the inner coat of the heart.
Visceral layer
it is the inner layer; it is closely adherent to the heart except along the cardiac grooves where it is separated from the heart by blood vessels. It is also called epicardium.
Parietal layer:
it is the outer layer; it lines the fibrous pericardium and is reflected around the roots of the great blood vessels to become Continuous with the visceral layer.
Fibrous pericardium: outer single layered (fibrous sac).
It is a conical shaped fibrous sac. It has an apex, base, anterior, posterior and two lateral surfaces.
Posteriorly:
It is pierced by the 4 pulmonary veins.
On each side: related to the mediastinal pleura separated from it by phrenic nerves and pericardiophrenic vessels.
is related to
middle 4 thoracic vertebrae.
descending thoracic aorta
oesophagus
principal bronchi
Anteriorly: is connected to the back of the body of the sternum by Superior and inferior sterno-pericardial ligaments.
Base: directed downwards. It is broad, rests on and fuses with the central tendon of the diaphragm. It is pierced by the IVC.
The apex: directed upwards. It surrounds the roots of the great blood vessels and fuses with their outer coats.
Is the outermost coat of the heart.
Functions of the pericardium:
Limits the cardiac distension.
Serves as a lubricated container in which the heart can contract and relax smoothly.
Restricts excessive movements of the heart.
The pericardium is a fibro serous sac which encloses the heart and the roots of its great vessels.
The Heart
External features of the heart (Fig. 2):
The heart has:
Four borders (upper-lower-right-left).
Upper border:
It is hidden by ascending aorta and pulmonary trunk lies in front of it.
It is formed by the two atria mainly the left atrium.
Lower border:
It separates the sternocostal surface from the diaphragmatic surface.
It is formed by the right ventricle.
It extends from the opening of IVC to the apex of the heart.
It is a horizontal border.
Left border:
It separates the sternocostal and the left surfaces.
It extends from the left auricle to the apex of the heart
It is formed mainly by the left ventricle and partly by the left auricle.
It is curved and oblique border.
Right border:
It separates the base from the sterno costal surface.
It extends from the right side of the opening of SVC to that of IVC.
It is a vertical border and is formed by the right atrium
Three surfaces (sterno costal – diaphragmatic – left).
left surface:
It directed upward, backward and to left.
It is formed mainly by the left ventricle and partly by the left atrium and auricle.
Diaphragmatic surface:
Formation: The left two thirds is formed by the left ventricle, and the right one third is formed by the right ventricle.
This surface is flat and rests on the central tendon of the diaphragm.
sterno costal surface:
Sterno-costal surface is convex and formed by:
Relations
2-6 costal cartilage separating from it by anterior border of lung and pleura except at cardiac notch.
Back of body of sternum.
part of sternocostal surface is uncovered by the left lung (cardiac notch) forming an area of superficial cardiac dullness.
The left atrium is hidden on the front by ascending aorta and pulmonary trunk.
Ventricular part:
Left one third formed by left ventricle
Right two third formed by right ventricle
Atrial part:
Left auricle.
right auricle
right atrium
Base
Descending thoracic aorta.
Esophagus
Oblique pericardial sinus
middle four thoracic vertebrae
Site: It lies in front of the middle four thoracic vertebrae
Direction: It is directed backwards and to the right.
The base or the posterior surface of the heart is formed by the two atria mainly by the left atrium.
Apex
Relation
Left copula of diaphragm separated it from fundus of stomach and left end of liver.
The left lung and pleura.
Site: It lies at the level of the left 5th intercostal space 3.5 inch (9cm) from the midline at the midclavicular line.
Direction: It is directed downwards, forwards and to the left.
The apex of the heart is a conical area formed by the left ventricle.
On the surface the atria are separated from the ventricles by the atrioventricular groove (coronary sulcus) which encircle the heart and ventricles are separated from each other by interventricular grooves.
Size
The heart is slightly larger than one’s clenched fist.
Weight = 300g in males, 250g in females.
Width = 9 cm.
Length = 12 cm.
Shape: pyramidal or conical.
The heart consists of 4 chambers: right atrium, right ventricle, left atrium and left ventricle.
It placed obliquely behind the sternum and adjoining parts of costal cartilages, one third of the heart is to the right of median plane and two thirds of the heart is to the left of the median plane.
The heart is a hollow muscular organ situated in the middle mediastinum, enclosed in the pericardium.
The mediastinum
Divisions: The mediastinum is divided by an imaginary plane passing through the sternal angle anteriorly and the lower border of the fourth thoracic vertebra posteriorly into two parts:
Inferior mediastinum.
The Inferior mediastinum is further subdivided into three parts by the pericardium (enclosing the heart).
Middle mediastinum: contains the heart and pericardium.
Posterior mediastinum: behind the heart and pericardium.
Anterior mediastinum: In front of the heart and pericardium.
Superior mediastinum.
On each side: The two pleural cavities.
Inferior: The diaphragm.
Superior: Thoracic inlet.
Posterior: The vertebral column (bodies of the thoracic vertebrae and intervertebral discs from T1 to T12).
Anterior: The sternum.
The mediastinum is the median space of the thoracic cavity between the two pleural cavities.
blood vessels
lower limb
superficial veins
small (short) saphenous vein
clinical correlation
if these factors failed to help the drainage , then the stagnation of blood
in the superficial veins causes varicose veins
the venous drainage of the lower limb is against the gravity and it is maintained by several factors
presence of
valves that alloon the direction of blood from superficial to deep
pulsations of the adjacent arteries
contraction of cuff muscles
End:
or may biforcate with
one limb terminating in the great saphenous vein
but some times it may end in the great saphenous vein
it usually ends into the popliteal vein
course: It runs upward behind the lateral malleotus , along the lateral edge of tedocalcaneusand is accompanied by Sural nerve on its lateral side
Then it ascends in the middle of the back of the leg them pierces the deep fascin , and it reaches the midle of the populated fossa
beginning: it is formed below and behind the lateral malleolus by the union of the
lateral dorsal digital vein of the little toe
lateraldorsal venous arch
great saphenous vein
valves in great saphenous vein:
Clinical correlation
vene section of the great saphenous vein
in emergency when the superficial veins all over the body are collapsed and invisible, the most prefered site of vene section (cut down) is the great saphenous vein in front of the medial malleolus to insert a Canulla for prolonged adminstration of intravenous fluide.During this procedure the saphenous nerve should be recognized (as it lies in front of the artery, to avoid its jury
there are about 10 to 20 values in the great saphenous vein
and the other lies at its Junction with the femoral vein (saphenofemoral valve)
one lies must before it Peirces the cribriform fascia
two of them lies at its end
tributaries: throughout its course, it receives superficial veins along the medial side of the foot, leg and thigh
Just before openning into the femoral vein it receives deep external pudendal vein
Just before piercing the cribriform fascia
superficial external pudendal vein
superficial circumflex iliac vein
superficial epigastric vein
course: The vein runs upward about 2.5cm in front of the medial maleolus, it crosses obliquely the medial"de of the Leg reach then neewhereitliesmontone hand-dreadth posterior to the patella; from here it runs upward along thect the thign to reach the saphenous opening
NB: Along its course on the dorsum of fast and Legaccomanied by saphenous nerve
Beginning: it is formed in the dorsum of the foot by the union of the medial end of the dorsal venous arch of the foot
it is the longest vein of the body and it is also called long saphenous vein
Popliteal region
Popliteat vein
tributaries: The tributaries of the popliteal vein are as following:
small saphenens vein
End: it continues as the femoral vein at adductor hiatus
course: it ascends superficial to popliteal artery and Crosses it from medial to lateral side in the popliteal fossa
Beginning: it is formed at the lower third poplitens by the union of veins (Venae commitants) accompanying the anterior and posterior tibial arteries
popliteal artery
Branches:
Genicular (articular) branches: They are five in number and supply the knee joint
middle germicular artery: It supplies the cruciate ligaments and synovial membrane of the knee joints
inferior medial and lateral genicular arteries
superior medial and lateral genicular arteries
muscular branches: to the nearby muscles
cutaneous branches: they supply the overlying skin
End:Itends at the lower border of the poplite us where it terminates by dividing into anterior and posterior tibia arteries
course: It descends downwards and laterally in the floor of popliteal fossa
through the fossait has a triple relation with popliteal vein and tibial nerve
At the lower part poplitear vein and tibial nerve are medial to the artery. Throughout the whole course the poplitear artery is separated from tibial nerve by popliteal vein.
at the middleport popliteal vein and tibial nerve are supercficial to artery
At the upper part popliteal vein and tibial nerve are superficial to artery
beginning: it begins at the adductor hiatus as a contillation of femoral artery
it is the deepest of neurovascular structures in the popliteal fossa
profunda femoris region
Profunda femoris vein
It drains into the femoral rein in the femoral triangle
It reaceives tributaries that correspond to the branches of the artery
profunda femoris artery
clinical Correlation
the femoral artery can be compressed against the femoral head at the miding iunal point to complete the bleeding in the distal part of the limb
four perfornting arteries: They are numbered from above downward
Lateral circumflex femoral artery
it is the largest branch
Medial circumflex femoral artery
acetatibular branch
ascending branch
transeverse branch
End: Itends as the fourth perforating artery to reach the back of the leg
Course: it arrises behind the femoral vessels then it passes to the back of the thigh
bigenning: it arrises from the lateral side Femoral artery in the femoral triangle about 4cm below the inguinal ligament
it is the largest branch of the femoral artery
Femoral region
femoral vein
tributaries
muscular tributaries
Deep external pudendal vein
Medial and lateral circumflex
profunda femoris vein
greats saphenous veinl longest tributary)
End: it continues as the external iliac vein behind the inguinal ligament medial to the mid-inguinal point
course: It ascends in adductor canal and enters the femoral triangle traversing the midle compartment of the femoral sheath
Beginning: it is the upward continuation of the popliteal vein at the adductor hiatus courseot
femoral artery
branches
in the adductor cannal
descending genicular artery
in the femoral triangle
three deep branches
Muscular branches
deep external pudendal artery
three superfacial branches: arranged from medial to lateral
superfacial circumflex iliac artery
superfacial epigastric artery
Superfacial external pudendal artery
end: it passes through adductor hiatus to enter the popliteal fossa as it continues as the popliteal artery
Course :
Lower 1/2
transaverses the adductor cannaltill it reaches adductor hiatus
upper 1/2
it enters the femoral triangle behind the inguinal ligament and descends downward and medialy to its apex
Beginning: it begins at midinguinal as continuation of external iliac artery
it is then main artery of the lower limb
Upper limb
Hand region
Superficial palmar arch
Cutaneous branches
Digital artery runs along the medial side of the little finger.
Three common palmar digital arteries for medial three and half finger.
Site: The superficial palmar arch lies deep to palmar aponeurosis and superficial to long flexor tendons. It lies nearly at the level of the heads of metacarpal bones.
Formation: It is formed by anastomosis between superficial palmar branch of the ulnar artery and the superficial branch of the radial artery.
It is the direct continuity of ulnar artery.
Deep Palmar Arch
Recurrent branch
Three perforating arteries
Three palmar metacarpal arteries
Site: The deep palmar arch lies deep to long flexor tendons and on the bases of metacarpal bones. It is 1 cm proximal to the superficial palmar arch
Formation: it is formed by anastomosis between direct continuation of the radial artery and the small deep palmar branch of the ulnar artery.
It is the direct continuation of radial artery.
Forearm region
Ulnar artery
Terminal branches
Clinical correlation: ❖ Examination of ulnar pulse: at the wrist just lateral to the pisiform carpal bone.
Smaller deep branch joins the deep palmar arch.
The superficial branch (the continuation of the artery) anastomoses with superficial palmar branch of the radial artery to form the superficial palmar arch.
In the forearm
Palmar and dorsal ulnar carpal branches which take part in the formation of palmar and dorsal carpal arches.
Common interosseous artery which arises from the upper part of the ulnar artery and passes for a very short distance till the upper border of interosseous membrane then divides into anterior and posterior interosseous arteries.
Anterior and posterior ulnar recurrent arteries which take part in the arterial anastomosis around the elbow joint.
Muscular branches to the neighboring muscles
End: It ends in the palm of the hand by dividing into large superficial and small deep branches.
Beginning: It begins in the cubital fossa at the level of the neck of the radius.
It is the larger terminal branch of the brachial artery.
Radial artery
Clinical correlation: While examining the radial pulse the thumb should not be used because it has its own pulse
Clinical correlation: ❖ Examination of radial pulse: It is felt on the radial side of the front of the radial artery covered only by the skin and fascia. The radial pulse is the commonest site for examining the pulse rate
In the palm of the hand:
Princeps pollicis artery which supplies the medial and lateral sides of palmar surface of the thumb.
Radialis indicis artery which supplies the lateral side of the palmar surface of the index finger.
In the dorsum of the hand:
The first dorsal metacarpal artery, which supplies adjacent sides of the index finger and thumb.
Dorsal carpal branch which joins the dorsal carpal arch.
In the Forearm:
Superficial palmar branch arises just above the wrist and enters the palm of the hand by passing in front of the flexor retinaculum. It joins the terminal part of the ulnar artery to form the superficial palmar arch.
Palmar carpal branch arises near the wrist and anastomosis with the palmar carpal branch of the ulnar artery.
Radial recurrent artery arises in the cubital fossa and takes part in the arterial anastomose around the elbow joint.
Muscular branches to the lateral muscles of the forearm
End: it passes between the two heads of the first dorsal interosseous muscle to enter the palm of the hand and form the deep palmar arch.
The radial artery leaves the forearm by winding around the lateral aspect of the wrist to reach the anatomical snuff box on the posterior (dorsal) surface of the hand.
In the distal part of the forearm, the radial artery lies on the anterior surface of the radius where it is covered only by the skin and fascia.
The superficial radial nerve lies lateral to the middle one-third of the radial artery.
The superficial radial nerve lies lateral to the middle one-third of the radial artery
Beginning:
It begins in cubital fossa at the level of the neck of radius.
It is the smaller terminal branch of the brachial artery.
Arm overall
Cubital region
The important features of median cubital vein:
It receives median vein of the forearm.
Median vein of the forearm
End: it ends in any one of three veins in front of elbow (cephalic, basilic and median cubital veins).
Course: it runs upwards in the midline on the anterior aspect of forearm.
Beginning: it begins from palmar venous network.
It is superficial to the bicipital aponeurosis which separates it from the brachial artery.
End: it ends in the basilic vein 2.5 cm above the elbow.
Course: it runs obliquely upwards and medially.
Beginning: It begins from the cephalic vein 2.5 cm below the elbow.
It is a communicating venous channel between the cephalic and basilic veins which shunts blood from the cephalic vein to the basilic vein.
Brachial region
Profunda brachii artery
Descending branch: It divides into smaller anterior and larger posterior terminal branches.
Muscular branch
Nutrient artery to humerus.
Ascending branch: It anastomoses with the descending branch of the posterior circumflex humeral artery.
End: it terminates by dividing into anterior and posterior descending branches which take part in the arterial anastomosis around the elbow joint.
Course: It accompanies the radial nerve while passing through the lower triangular intermuscular space to enter the spiral groove on the back of the humerus. It supplies the posterior compartment of the arm.
Beginning: It arises from the brachial artery just below the lower border of the teres major
Brachial artery
Clinical correlation:
Compression of brachial artery: The brachial artery can be effectively compressed against the shaft of humerus at the level of insertion of coracobrachialis to stop the hemorrhage occurring from any artery distal to the brachial artery.
Examination of brachial pulse: The brachial pulse is commonly felt in the cubital fossa medial to the tendon of biceps (cubital pulse) and its pulsations are auscultated for recording the blood pressure.
Terminal branches: Radial and ulnar arteries
Inferior ulnar collateral artery arises near the lower end of humerus and divides into the anterior and posterior branches, which take part in the arterial anastomosis around the elbow.
Superior ulnar collateral artery arises near the middle of the arm and accompanies the ulnar nerve.
Nutrient artery to the humerus.
Muscular branches to the muscles of the anterior compartment of the arm
Profunda brachii artery (the largest and first branch).
End: it ends in cubital fossa at the level of the neck of the radius where it divides to radial and ulnar arteries.
Course: it descends downwards and laterally in the arm. Its upper half is medial to the humerus while its lower half is in front of it. At the level of insertion of coracobrachialis, the median nerve crosses superficial (anterior) to the brachial artery from lateral to medial. In the cubital fossa, the brachial artery lies immediately medial to the tendon of the biceps brachii muscle and the artery is crossed by the bicipital aponeurosis.
Beginning: it begins at the lower border of teres major muscle as continuation of axillary artery.
It is the artery of the arm.
End: it pierces the clavi-pectoral fascia and drains into the axillary vein
Course: It crosses the roof of anatomical box, ascends on the lateral border of the forearm, continues upwards in front of elbow along the lateral border of biceps, pierces the deep fascia at the lower border of the pectoralis major, runs delto-pectoral groove.
Beginning: it begins as the continuation of lateral end of the dorsal venous arch.
End: it unites with the brachial veins and runs along the medial side of the brachial artery to become continuous with the axillary vein at the lower border of the teres major.
Course: It runs upwards along the back of the medial border of the forearm, winds round this border near the elbow to reach front of the forearm, where it continues upwards in front of the elbow along the medial side of the biceps brachii up to the middle of the arm, where it pierces deep fascia.
Axillary region
Axillary vein
End: it ends at the outer border of the first rib by becoming subclavian vein.
Course: it runs medial to the axillary artery.
Clinical correlation: Venipuncture in the cubital fossa: The veins in front of the elbow, e.g., median cubital vein, cephalic vein, and basilic vein are routinely used for giving intravenous injections and for withdrawing blood from the donors.
Cephalic vein after piercing the clavipectoral fascia
Veins which correspond to branches of the axillary artery.
Beginning: it is formed at the lower border of teres major muscle by union of basilic vein and vena commitants of brachial artery
Dorsal venus arch
Brachial veins
Deep veins of the forearm accompany the arteries and drain into brachial veins associated with the brachial artery in the cubital fossa.
They end in axillary vein.
They receive tributaries corresponding to the branches of the artery.
Paired brachial veins (venae comitantes) pass along the medial and lateral sides of the brachial artery.
Axillary artery (upper limb)
From the third part (3 branches):
Posterior circumflex humeral artery.
Anterior circumflex humeral artery.
Subscapular artery.
From the second part (2 branches):
Lateral thoracic artery.
Thoraco-acromial artery.
From the first part (1 branch):
Superior thoracic artery
End: it ends at the lower border of teres major muscle as the brachial artery.
Parts
Third part: below pectoralis minor.
Second part: deep to pectoralis minor.
First part: above pectoralis minor.
Course: it runs in the axilla from apex to base surrounded by the cords and branches of brachial plexus. The axillary vein lies medial to it throughout the course It is crossed superficially by pectoralis minor muscle which divides the artery into three parts.
Beginning: it begins at the outer border of the first rib as continuation of subclavian artery.
It is the main artery of the upper limb.
Subclavian region
Subclavian vein
Tributaries
Cephalic vein. Only sometimes
Anterior jugular vein. Only sometimes.
Dorsal scapular vein.
Thoracic duct on the left side and right lymphatic duct on the right side (Main)
External jugular vein. (Main)
extends from the outer border of the first rib to the medial border of the scalenus anterior, where it joins the internal jugular vein to form brachiocephalic vein. The subclavian vein is principally the vein of the upper limb.
Hint about Veins of the upper limb
The veins draining the upper limb are divided into
deep
lie deep to muscles and accompany arteries as venae comitantes (previously mentioned with the arteries).
superficial
Consist of:
Median cubital vein
Basilic vein
Cephalic vein
Dorsal venous arch
lie in the superficial fascia and are easily accessible they are frequently used by the clinicians for drawing blood samples or for giving intravenous injections.
Subclavian artery:
Branches of the Subclavian Artery
From the third part:
Dorsal scapular artery: It is an occasional branch that may arise from the third part of the subclavian artery. When present, it replaces the deep branch of the transverse cervical artery.
From the second part:
deep cervical artery
superior intercostal artery
Costocervical trunk.
From the first part:
Internal thoracic artery
Thyro-cervical trunk
Suprascapular artery
Transverse cervical artery
Inferior thyroid artery
Vertebral artery
Termination
At the outer border of 1st rib, it ends by becoming axillary artery
Course
In the neck, both the arteries have a similar course. Each subclavian artery arches laterally deep to the scalenus anterior muscle which divided it into 3 parts
Third part—extends from the lateral border of scalenus above the upper surface of the first rib.
Second part—lies behind the scalenus anterior muscle.
First part—extends from its origin to medial border of scalenus anterior in front of cervical pleura.
The left subclavian artery arises from the arch of aorta in the thorax.
The right subclavian artery arises from the brachiocephalic trunk behind the right sternoclavicular joint at the root of neck.
Neck
Superficial veins of the neck
Anterior jugular vein
Termination: terminates in the external jugular vein. In the suprasternal space, the anterior jugular vein is united across the midline to its fellow of opposite side by a transverse venous channel called jugular venous arch.
Beginning: It begins below the chin in the submental region by the union of small unnamed veins from the chin.
External jugular vein
Termination: it terminates in the subclavian vein.
Beginning: It begins just below the angle of the mandible by the union of posterior division of retromandibular vein and posterior auricular vein.
Internal jugular vein
In addition to the abovementioned tributaries
thoracic duct on the left side,
the right lymphatic duct on the right side
Tributaries (Fig. 54)
Occipital vein (only sometimes).
Middle thyroid vein.
Superior thyroid vein.
Lingual vein.
Common facial vein.
Pharyngeal veins.
Inferior petrosal vein.
Termination: it ends behind the sternal end of the clavicle by joining the subclavian vein to form the brachiocephalic vein.
Course: it descends vertically inside the carotid sheath lateral to ICA then CCA
Beginning: It begins as the direct continuation of the sigmoid sinus at the base of the skull below the jugular foramen.
The internal jugular vein is usually the largest vein in the neck.
Common carotid arteries
Branches
internal carotid artery
Cerebral part:
Terminal branches:
Middle cerebral artery
Anterior cerebral artery
Posterior communicating artery
Anterior choroidal artery
Ophthalmic artery
Cavernous part:
Superior and inferior hypophyseal arteries to the hypophysis cerebri (pituitary gland).
Cavernous branches to the trigeminal ganglion.
Petrous part:
Pterygoid branch (small and inconstant) enters the pterygoid canal.
Caroticotympanic branches to middle ear.
Cervical part: In the neck, the internal carotid artery gives no branches.
Termination: it ends below the anterior perforated substance of the brain by dividing into the anterior and middle cerebral arteries.
Course: the course of the internal carotid artery is divided into the following four parts:
4. Cerebral part: This part lies at the base of the brain.
3. Cavernous part: lies within the cavernous sinus.
2. Petrous part: lies in the petrous part of the temporal bone in the carotid canal. It enters the cranial cavity by passing through the upper part of the foramen lacerum.
1. Cervical part: lies on the front of transverse process of upper cervical vertebrae. It is enclosed in the carotid sheath along with the internal jugular vein and vagus nerve. It enters the carotid foramen at the base of the skull
Beginning: at the upper border of the lamina of thyroid cartilage at the level of the disc between C3/C4 vertebrae as one of the two terminal branches of the common carotid artery.
external carotid artery
Branches (Fig. 52): The external carotid artery gives rise to eight branches as follows:
8. Superficial temporal artery.
7. Maxillary artery.
6. Posterior auricular artery.
5. Occipital artery.
4. Facial artery.
3. Lingual artery.
2. Ascending pharyngeal artery.
1. Superior thyroid artery.
Termination: In the substance of the parotid gland behind the neck of the mandible by dividing into the superficial temporal and maxillary arteries.
Course: It extends upwards outside the carotid sheath. It first lies in the carotid triangle then deep to posterior belly of digastric and finally inside parotid gland.
Beginning: at the upper border of the lamina of thyroid cartilage at the level of disc between C3/C4 as one of the two terminal branches of the common carotid artery
Termination: opposite the upper border of the lamina of thyroid cartilage (C3/C4), where it terminates by dividing into internal and external carotid arteries.
N.B The carotid sinus is a dilatation of the end of CCA and the beginning of ICA. Branches
The internal carotid artery is considered as a continuation of common carotid artery.
Course: In the neck, from the sternoclavicular joint, each artery runs upwards and backwards in front of transverse processes of lower four cervical vertebrae inside the carotid sheath medial to IJV and under the cover of anterior border of the sternocleidomastoid muscle.
The left common carotid artery arises in thorax (superior mediastinum) directly from the arch of aorta. It ascends behind left sternoclavicular joint and enters the neck.
The right common carotid artery arises in neck from brachiocephalic trunk (innominate artery) behind the sternoclavicular joint.
There are two common carotid arteries: right and left. They are the chief arteries of the head and neck.
Renal
مستجد
الرينال بالتحديدات
Anatomy Not included
Obstructive
*stones
*hydronephrosis
*pyonephrosis
Mcq
Pharma All topics
Pharmacology
DRUGS AFFECTING POTASSIUM HOMEOSTASIS
Treatment of hyperkalemia:
K+ losing diuretics.
I.V. NaHCO3.
I.V. glucose + insulin (6-8 units +20 gm i.v. glucose).
I.V. calcium:
Ca+2 rises threshold of firing away from resting potential.
Ca+2 antagonizes the effect of K+ at membrane potential.
Causes of hyperkalemia
Spironolactone
ACEIs decrease aldosterone.
Hypoaldosteronism
Impaired renal function.
Acidosis
Digitalis
Succinylcholine
Blocking B1 receptors & NSAIDs →inhibit renin.
Blocking B2 receptors.
Treatment of hypokalemia:
Oral K+ (irritant) or I.V. K+ (produces phlebitis).
K+ retaining diuretics in case of using K+ losing diuretics or hyperaldosteronism.
K+ rich diet (banana).
Causes of hypokalemia:
Hyperaldosteronism, liquorice and carbenoxolone.
K+ losing diuretics e.g. loop and thiazide diuretics.
Metabolic alkalosis induced by diuretics increases outflux of H+ in exchange with K+.
Catecholamine (B2 agonists).
Insulin in large doses.
Control of K+ permeability:
Aldosterone enhances excretion of K+ in exchange with Na+ in distal convoluted tubules.
Na+ /K+ ATPase enzyme, insulin and B2 agonists activate this enzyme.
ANTI-diuretics
Noradrenaline and serotonin which are powerful vasoconstrictors and decrease renal blood flow.
Thiazides have antidiuretic effect only in nephrogenic diabetes insipidus.
Antidiuretic hormone "ADH" (Vasopressin): ADH regulates H2O reabsorption from collecting ducts. Secretion of ADH is stimulated in cases of hypovolemia and hypertonictiy leading to increase H2O reabsorption and excretion of concentrated urine. In cases of volume expansion and hypotonicity secretion of ADH is inhibited, H2O reabsorption is decreased with excretion of diluted urine.
K+ sparing diuretics
Side effects of K+ sparing diuretics
N.B.In choosing a diuretic for the patient with kidney disease, there are a number of important limitations:
Lastly, although excessive use of diuretics can impair renal function in all patients, the consequences are more serious in those with underlying renal disease.
Thus, loop diuretics are often the best choice in treating edema associated with renal failure.
Thiazide diuretics are generally ineffective when glomerular filtration rate falls below 30 mL/min.
Potassium-sparing diuretics may cause hyperkalemia.
Acetazolamide must usually be avoided as it can exacerbate acidosis.
Spironolactone has delayed onset of action
Spironolactone has anti- androgenic effect. It may cause gynecomastia in males and menstrual disturbance in females
Metabolic acidosis.
Uses of K+ sparing diuretics
Both groups are used in:
When loop diuretics and thiazides are contra- indicated as in:
Digitalis toxicity. _ Gout. _ Hypokalemia. _ Hypersensitivity.
Hypertension in combination with thiazides to increase diuretic effect and correct hypokalemia.
Reduces edema in nephrotic syndrome.
Reduces edema and ascites associated with hepatic cirrhosis (Spironolactone is considered the diuretic of choice in patients with hepatic cirrhosis).
Spironolactone decreases edema, increases the survival of patients in advanced stages of heart failure (prevents the remodeling that occurs as compensation for the progressive failure of the heart).
Spironolactone is used in hyperaldosteronism, either primary or secondary, that may be a cause of refractory edema :
Amiloride and triametrene: both directly block Na+ channels, leading to inhibition of NaCl reabsorption and decreasing K+ and H+ secretion. They have rapid onset of action, compared to spironolactone.
Spironolactone and eplerenone: competes with aldosterone for its binding site in collecting duct cells, blocking protein synthesis which stimulates Na+ pump, this leads to inhibition of NaCl reabsorption and decreasing K+ and H+ secretion, predisposing hyperkalemia and metabolic acidosis. So, spironolactone has delayed onset of action (3-4 days).
Weak diuretics. Figure (3.22):
Thiazide Diuretics
Contra-indications
In renal failure, thiazides are not effective (defective secretion).
Liver impairment (hepatic encephalopathy)
Hyperlipidemia
Digitalis toxicity
Allergic reactions: thiazides are sulfonamides and so, there is cross hypersensitivity with other sulfonamides.
Hyperlipidemia: thiazides increase serum cholesterol and LDL, increasing risk of atherosclerosis (except indapamide).
Hyponatremia: an important adverse effect with thiazides.
Hyperglycemia: thiazides inhibit pancreatic insulin release due to K+ channel opening, increasing K+ efflux and decreasing Ca2+ influx. Also, thiazides decrease tissue utilization of glucose
Hyperuricemica: thiazides compete with uric acid at organic acid secretory system in PCT, inhibiting its secretion.
Hypokalemia and metabolic alkalosis due to increased secretion of K+ and H+ in the collecting duct.
Intermediate-acting thiazides: (given twice daily)
Benzathiazide
Cyclothiazide
Long-acting thiazides: (given once daily)
Indapamide
Chlorthalidone
Short-acting thiazides:
Hydrochlorothiazides
Chlorothiazides
Nephrogenic diabetes insipidus: By chronic use, thiazides decrease plasma volume and reduce glomerular filtration rate (paradoxical anti-diuretic effect).
Idiopathic hypercalcuria: Thiazides by increasing Ca2+ reabsorption, decrease its excretion prevent stone formation.
Mild and moderate CHF.
Hypertension: thiazides are used in mild and moderate hypertension.
Initial fall of blood pressure results from diuretic effect and reducing blood volume. The persistent antihypertensive effect results from vasodilatation due to opening of k+ channels.
Mechanism of action Figure (3.21 ):
At high doses, thiazides inhibit C.A. enzyme.
Opening K+ channels.
Effect on Ca2+: Thiazides increase Ca2+ reabsorption from the DCT, increasing Ca2+ level in blood. This effect may result from increasing Na+/Ca2+ exchange due to reduced intracellular Na+ concentration.
Thiazides inhibit Na+/Cl− cotransporter in early part of distal convoluted tubule (DCT) so inhibit NaCl reabsorption from early part of DCT, increasing excretion of NaCl and water.
All thiazides reach site action by active secretion through organic acid secretory system in PCT and compete with uric acid secretion by that system, increasing serum uric acid.
Moderate efficacy diuretics.
Drug interactions of LDs
Aminoglycosides ( ototoxicity).
Warfarine: displacement form plasma protein binding sites.
NSAIDS: inhibit secretion of LDs in PCT and inhibit PG synthesis.
Probencid: inhibit secretion of LDs in PCT.
Contra-indications of LDs
Liver disease
With steroids
Gout
Hypokalemia
Digitalis toxicity.
Resistance to LDs (Causes and how to overcome)
Increase Na+ reabsorption in DCT combine with thiazides.
Decreased secretion to site of action due to renal impairment ® increase dosage of loop diuretic.
Hypoalbuminemia (decreased protein binding) mix with albumin.
Decreased bioavailability due to defective GIT reabsorption (CHF) given by I.V. route.
Side effects of LDs
Interstitial nephritis
Severe GIT disturbance with ethacrynic acid
Hypersensitivity reactions "sulfonamide moiety".
Reversible ototoxicity, especially with other ototoxic drugs as aminoglycosides. Ethacrynic acid is more ototoxic than other loop diuretics
Hypomagnesemia and hypocalcemia
Hypovolemia, hypotension and haemoconcentrationزيادة تركيز كرات الدم الحمراء فى الدم
الوحية اللى بتزيدHyperuricemia: lds decrease secretion of uric acid in PCT.
Hyponatremia
Hypokalemia and metabolic alkalosis.
Preparations and dosage of LDs
Torsemide
Ethacrynic acid.
Bumetanide
Frusemide
Uses of LDs
هام جداN.B. For treatment of hypercalcemia and anion over dosage, saline should be given to avoid hypovolemia and to replace urinary loss of NaCl.
Anion overdosage, as bromide, fluoride and chloride.
Hypercalcemia
Acute renal failure to enhance K+ excretion and to increasing urine flow (by increasing renal vasodilator PG and glomerular filtration).
Refractory oedema; in severe CHF, nephrotic and nephritic syndromes, and liver cirrhosis.
Acute pulmonary oedema.
Pharmacodynamics of LDs: Figure (3.20)
LDs increase PG synthesis that participate in the renal action, through V.D. of afferent arteriole and increase renal blood flow.
LDs inhibit Na+/ K+/2Cl- cotransport system in the thick ascending loop of Henle. This will lead to:
Decrease luminal positive potential →inhibiting reabsorption of Ca2+ and Mg2+
Inhibition of NaCl reabsorption →Abolish hypertonicity of medulla, preventing concentration of urine
Pharmacokinetics of LDs
LDs reach their site of action by active secretion by organic acid secretory system in PCT, the fraction not secreted is metabolized in the liver.
LDs are strongly bound to plasma proteins
Bioavailability is high, reaching 100% with bumetanide.
Rapidly absorbed from GIT and injection sites rapid onset.
Osmotic Diuretics
Mannitol, urea and Glycerol
Side effect
Hypersensitivity reactions.
Headache, nausea and vomiting.
Extracellular volume expansion; Mannitol for example, is rapidly distributed in the extracellular compartment and extracts water from cells. Prior to the diuresis, this leads to expansion of the extracellular volume and hyponatremia.
Dose: Mannitol is given by I.V. infusion.
Prophylaxis of acute renal failure: In impending renal failure, osmotic diuretics increase rate of urine flow and rapidly excrete toxic substances that may cause renal damage.
Cerebral oedema (↑ ICP) and acute glaucoma (↑ IOP). Osmotic diuretics increase plasma osmolarity, leading to extraction of H2O from the brain and the eye reducing ICP and IOP.
Mechanism of action
As a result of use of these diuretics, urine osmolality is low, urine flow increases, and Na+ loss is minimal.
By increasing osmotic pressure in tubular fluid, osmotic diuretics inhibit H2O reabsorption, increasing water excretion and increasing urine volume. The increase in urine flow rate decrease contact time between fluid and tubular epithelium, decreasing Na+ reabsorption. They do not have major effects on the Na+ reabsorption processes in the tubules. The increase in urine flow rate decrease contact time between fluid and tubular epithelium, decreasing Na+ reabsorption. But natriuresis is less that H 2 O diuresis.
Not absorbed from GIT; if given orally they produce osmotic diarrhea.
Not metabolized - Not reabsorbed from renal tubules.
They act by increasing the tubular osmotic pressure in the segments freely permeable to water such as the PCT, descending loop of Henle and collecting duct.
These diuretics are freely filtered at the glomerulus.
Carbonic anhydrase inhibitors (CAIs)
Preparations
Dorzolamide, local for treatment of glaucoma.
Methazolamide
Ethoxazolamide
Acetazolamide
Side effects of CAIs
Hypersensitivity reactions
Renal stones "calcium and phosphate stones" due to alkalinization of urine.
Metabolic acidosis leading to drowsiness and disorientation.
Uses of CAIs:
Epilepsy: CAIs are used as an adjuvant agent in treatment of epilepsy.
Acute mountain syndrome: CAIs are given 24 hours before the ascent to decrease CSF formation.
Metabolic alkalosis: Due to excessive use of diuretics in CHF.
Alkalinization of urine: To enhance excretion of acids and acid drugs as aspirin.
Glaucoma: The most common indication for CAIs.
Dorzolamide is a topically active CAI, used in treatment glaucoma.
As a diuretic, CAIs inhibitors are weak when used alone. They are used in combination with loop diuretics in refractory congestive heart failure (CHF).
Actions of CAIs: Figure ( 3,19).
CNS: CAIs decrease formation CSF. Also, CAIs- induced acidosis suppress epileptic foci.
Eye: CAIs decrease formation of aqueous humour leading to decrease of IOP.
Diuretic actions:
CAIs are weak diuretics because Na+ reabsorption in remaining tubule is enhanced.
When acidosis occurs, H+ is derived into the tubules without the action of CA enzyme (carbonic anhydrase–independent mechanisms) and tolerance develops to the diuretic effect of CAIs (self- limiting diuretics).
This will lead to excretion of alkaline urine and decrease in blood HCO3- causing metabolic acidosis.
CAIs interfere with H + production and excretion in renal tubules, leading to inhibition of NaHCO3 reabsorption from PCT.
CA enzyme is also present in:
Eye for the formation of aqueous humour.
Brain, RBCs, stomach.
CA enzyme is present in proximal convoluted tubule (PCT) cells, both luminal and intracellular, where it calalyses NaHCO3 reabsorption.
Each type of the diuretic targets specific transporters in the nephron segments as shown
Diuretics are used to increase the renal excretion of Na+ and water
MCQs and OSPE exams topics:
All curriculum will be covered.
HISTOLOGICAL STRUCTURE OF EXCRETORY PASSAGES
Female Urethra
Paraurethral (Littre) glands
(Bartholin glands)
It formed of smooth muscle fibers inner longitudinal and outer circular, striated muscle fibers in external sphincter at its end.
Lamina propria
It is a corium of connective tissue with mucus secreting cells like litter's gland and plexus of veins
At the orifice, it changes to stratified squamous epithelium
The lining epithelium is transitional and stratified or pseudostratified columnar from urinary bladder outwards.
Contains longitudinal folds.
It extends from the bladder and ends in the vestibule.
It has a skeletal muscle sphincter at its terminus.
It is much shorter than male urethra (4cm). (Fig. 4.18)
Male Urethra
Associated glands
Bulbourethral glands (Cowper’s glands).
Urethral glands of Littre.
Seminal vesicles.
Prostatic gland.
Its wall is formed from:
Lamina propria: It is a corium of connective tissue rich in elastic fibers with branched tubular gland (Littre's gland lined by columnar mucous cells).
It is covered by
stratified squamous in terminal part (penile part).
, pseudostratifid columnar or stratified columnar in membranous part
transitional epithelium in prostatic part,
It is divided into: (Fig 4.17, 4.18).
Cavernous (penile) urethra extends in the corpus spongiosum (12-15cm).
Membranous urethra: extends from the apex of the prostate to the bulb of the penis (1cm), surrounded by the external urethral sphincter formed by the pelvic muscles.
Prostatic urethra: in the prostate (3-4cm), surrounded by the internal urethral sphincter.
Urinary Bladder
Its wall formed from 3 layers: mucosa, musculosa and adventitia or serosa (Fig 4.16).
Adventitia: It has a fibro-elastic connective tissue except in the upper surface replaced by serosa (simple squamous epithelium).
It consists of 3 main coats: inner longitudinal, middle circular and outer longitudinal, but they are irregular and randomly mixed with collagen fibers.
The bundles of detruser muscle are less regularly arranged as in the tubular excretory passages.
It forms the involuntary internal urethral sphincter at the urethral opening.
The smooth muscle forming the wall is the detruser muscle.
Lamina propria: Connective tissue with abundant elastic fibers.
Lined by transitional epithelium which has a remarkable ability to change its morphology in relaxed and distended states:
In distended state, it is about 3 layers.
In empty state, it is 6-8 layers.
It has 3 openings, two for the ureters and one for the urethra. These 3 openings form a triangular smooth area (not folded) and constant in thickness (has different embryological origin).
Its wall is thicker than ureteric wall.
It is a distensible reservoir of urine.
Ureter
Its wall formed from 3 layers: mucosa, musculosa and adventitia (Fig 4.15).
Adventitia: Fibrous connective tissue containing blood vessels, nerves and lymphatic cells
The contraction of these muscle layers produces peristaltic waves that push urine along to enter the urinary bladder.
The lower 1/3 formed inner longitudinal, middle circular and outer longitudinal layers.
The upper 2/3 formed of inner longitudinal and outer circular layers.
The lumen appears narrow and stellate due to infoldings of the mucosa.
Corium of connective tissue contains blood vessels and lymphatics.
It is composed of transitional epithelium.
It is a hollow long tube (25-30cm long and 3-4mm in diameter) extending from the renal pelvis to the urinary bladder.
The transitional epithelium is the main lining of the urinary passages (so called urotheluim). It is characterized by:
The surface cells are called" facet cells” characterized by:
The apical border also contains small vesicles continuous with the cell membrane (represent inward folds of the membrane) to help accommodation during distension (become unfolded).
They have occluding junction in-between.
Some cells are binucleated.
They are large, dome-shaped with thick apical cell membranes, called “plaques”.
It acts as an osmotic barrier against hypertonic urine.
Its number of layers is changeable according to the state of distension (3-8 layers).
It is a type of stratified epithelium.
The wall of these passages is formed of three layers:
Adventitia
Musculosa
Mucosa
Urine formed in the kidney is collected and transported into; minor and major calyces, renal pelvis, ureters and then to the urinary bladder where it is stored until conducted by the urethra to outside the body.
Written
●Nephron including:
1- Renal Malpighian corpuscle.
2- Proximal convoluted tubule.
3- Loop of Henle.
4- Distal convoluted tubule.
5- Juxtaglomerular Apparatus (JGA)
●Collecting system including:
1. Collecting tubule
2. Collecting ducts
Nucleotide Metabolism
Synthetic nucleotide analogue:
They act by inhibiting enzymes essential for nucleic acid synthesis or their incorporation into nucleic acid with disruption of base pairing.
They are used chemotherapeutical to control cancer or infection.
They are prepared by altering the ring or sugar moiety.
Hereditary orotic aciduria:
It is characterized by increased excretion of orotic acid in urine, anemia and growth retardation. It is treated by oral uridine. There are two types of orotic aciduria.
Type II: Deficiency of ortidylate decarboxylase.
Type I: Deficiency of orotate phosphoribosyl transferase.
Synthesis of deoxyribonucleotides:
This reaction needs the presence of reduced thioredoxine and NADPH as hydrogen donors.
Ribonucleoside diphosphate is reduced by ribonucleoside reductase to form deoxyribonucleoside diphosphate.
Prymidine nucleotides
SYNTHESIS OF THE PYRIMIDINE NUCLEOTIDES
The origin of the bases in the pyrimidine ring:
CO2 gives C2
Glutamine gives N3
Aspartic acid gives N1,C4,5,6
Purine nucleotides
Degradation of purine nucleotides:
End product
Humans convert adenosine and guanosine to uric acid
Uric acid
DISEASES ASSOCIATED WITH PURINE DEGRADATION:
GOUT
Treatment of Gout
Long-term therapeutic strategies for gout involve Uricosuric agents, such as probenecid or sulfinpyrazone, that increase renal excretion of uric acid, are used in patients where “underexcretors” of uric acid.
Clochicine: It is anti-inflammatory drug. It inhibits phagocytsis of uric acid crystals by white blood cells that leads to lysis of W.B.Cs and enhancing the inflammatory response and inflammatory arthritis.
Allopurinol: competitive inhibitor for enzyme xanthine oxidase, so, inhibits production of uric acid.
Diet: Avoid rich sourced of nucleoproteins e.g. meat, liver, kidney (Substituted with other sources of proteins for these patients should be milk, cheese, yoghurt and eggs).
Effects of hyperuricemia (Gout):
When the blood uric acid exceeds 7 mg/dl, it will form crystals of sodium urate.
Precipitation of uric and/or sodium urate in renal tubules → kidney stone formation.
- Precipitation of sodium urate under the skin → Tophi. The tophi cause an inflammatory reaction.
Precipitation of sodium urate, in joints [small joints] → Arthritis which usually starts at metatarsophalangeal joint of big toe.
Causes of gout: - Metabolic gout -Renal gout
Renal gout: Due to decreased excretion of uric acid as in case of renal failure.
Metabolic gout: There are two types of metabolic gout: primary and secondary
Causes of Secondary Metabolic Gout Due to increased synthesis (↑ cell division) and catabolism of nucleic acid and nucleotides leads to increased production of uric acid. This occurs in cancer, leukemia, psoriasis, hemolytic anemia and polycythemia
Causes of primary metabolic gout:
It is due to increase of de novo synthesis, increase production of phosphoribosyl pyrophosphate (PRPP). It is usually an inherited metabolic defect.
Lesch Nyhan syndrome:
They are also prone to chewing off their fingers and performing other acts of self-mutilation.
Deficiency HGPRT ase → Block salvage pathway, enhance catabolic pathways for guanine and hypoxanthin to xanthin and uric acid. Also, de novo biosynthesis of purine base is upregulated leading to increased production of uric acid .
It is an X-linked recessive disease characterized by deficiency of hypoxanthine guanine phosporibosyl transferease [HGPRT ase] enzyme activity.
Von – Gierk disease (deficiency of glucose -6- phosphatase): Deficiency of glucose -6- phosphatase →↑ glucose -6-P that take part in HMP pathway →↑ ribose -5-P → increase production PRPP, which in turn leads to increased purine base biosynthesis and increase uric acid formation.
It is a metabolic disease characterized by hyperuricemia i.e. plasma uric acid more than 7 mg/dl in males or 6 mg/dl in females. Gout occurs predominantly in males.
Normal uric acid levels :
Plasma uric acid (urate) levels are 4-7 mg/dL for males and 3-6 mg/dL for females during fasting.
FORMATION OF URIC ACID
In liver for purine nucleotide synthesized by denovo pathway.
In small intestine for dietary nucleic acids.
Synthesis of purine nucleotides
There are two synthetic pathways:
Salvage pathway for purine nucleotide biosynthesis:
Salvage of purine nucleosides:
Deoxy adenosine by Kinase will give deoxyadenosine monophosphate
Adenosine by Kinase to give AMP
Salvage of free purines:
Hypothansine or Guanine by hypoxanthine guanine phosphoribosyl transferase (HGPRTase) to give IMP or GMP
Adenine by adenine phosphoribosyl transferase will give AMP
Purines that result from the normal turnover of cellular nucleic acids, or that are obtained from the diet and not degraded, can be converted to nucleoside triphosphates and used by the body.
↓ Uric acid formation.
↓ ATP utilization
↓ de novo biosynthesis.
Advantage of salvage pathway includes:
This is referred to as the “salvage pathway” for purines.
Because the de novo pathway requires six high-energy bonds per purine produced, a salvage pathway, which is used by many cell types, can convert free bases and nucleosides to nucleotides.
De novo synthesis of purine nucleotides:
Nine steps are proceed to form inosine monophosphate (IMP). 4-IMP is converted to AMP and GMP.
PRPP reacts with glutamine in the presence of glutaminePRPP amidotransferase to form 5-phosphoribosylamine with release of PPi.
Ribose 5- P is converted to 5-phosphoribosyl-1-pyrophosphate (PRPP) by PRPP synthetase.
Site: In the liver, and the nitrogenous bases and nucleosides are then transported to other tissues by red blood cells. The brain also synthesizes significant amounts of nucleotides.
Sources of the individual atoms in the purine ring:
Nitrogen 1 by aspartate.
Carbon 6 by CO2.
Nitrogen 3 and 9 by glutamine,
Carbon 2 is provided by formyl tetrahydrofolate.
Carbon 8 is provided by methenyl tetrahydrofolate .
Carbons 4 and 5 and Nitrogen 7 of the purine ring is provided by glycine.
Most tissues are able to synthesize its own purine by de novo synthesis.
Importance of nucleotides:
ATP plays an important role as “energy currency” in the cell.
cAMP and cGMP serve as second messengers in signal transduction pathway.
Structural components of coenzymes e.g. coenzyme A, FAD, NAD, and NADP.
Nucleotides e.g. UTP, CTP, GTP serve as carriers of activated intermediates in the synthesis of some carbohydrates, lipids, and proteins.
Formation of RNA and DNA.
Mcq كله
Renal handing
BLADDER FILLING, MICTURITION REFLEX
Abnormalities of Micturition:
In all types, bladder contractions are NOT sufficient for evacuation leaving “residual urine”.
Abnormalities of micturition arise from.
Interruption of facilitatory and inhibitory pathways from brain (Transection of the spinal cord).
Note that in all stages of spinal cord lesion the patient does not feel the filling or emptying of the bladder.
Stage of failure: resulting from bacterial toxins → destruction of sacral segments → retention with overflow.
Stage of recovery: release of spinal centres from the inhibitory effect of higher centres resulting in “automatic bladder” means that accumulation of urine → ↑ intra vasical pressure → micturition (as occurs in infants).
Stage of shock: bladder distended and flaccid i.e., there will be retention with overflow.
Trauma of spinal cord with complete transection above the level of the sacral segments
Interruption of afferents and efferent of bladder (De-nervation).
Then, the bladder becomes shrunken and hypertrophied and sometimes is called “neurogenic bladder” As the bladder becomes more sensitive to circulating transmitter leading to dribbling of urine.
At first, bladder becomes atonic i.e. there will be retention with over flow.
Trauma to sacral segments 2, 3, & 4.
Tumours affecting cauda equine
Interruption of afferents from bladder (De afferenation).
When bladder becomes full of urine, any extra urine will pass via urethra as drops “retention with overflow”.
Bladder becomes distended with urine and flaccid (Atonic bladder).
cutting of the sacral roots by:
Experimental
Tabes dorsalis
Modulation of micturition reflex
Voluntary control of micturition:
This is present after myelination of pyramidal tracts.
So, adults have a voluntary control over micturition reflex in two ways:
Voluntary initiation of micturition (Voiding reflex):
With voluntary helping of micturition, less than 5 ml of residual urine remains in bladder. This prevent infection & stone formation.
This initiation occurs by:
Relaxation of perineal muscle & pelvic floor muscles.
Contraction of abdominal muscles increases intra vesical pressure.
Relaxation of the external sphincter.
Facilitation of spinal centre (sacral 2,3,4).
Voluntary delay of micturition (Storage reflex):
This delay occurs by:
Contraction of the external sphincter.
Inhibition of spinal centres (sacral 2,3,4).
By descending pathways from higher centres to spinal cord.
Activity of sacral micturition centre can be modified by higher centres:
Facilitatory area in Pons.
Facilitatory area in Posterior hypothalamus.
Inhibitory area in midbrain
Cortical area (voluntary): mainly inhibitory. (But, can do facilitation).
Sympathetic control of micturition: -It has no role in normal micturition.
Table 4.4: Reflex arc
Response
Effector organ: Bladder wall & internal urethral sphincter.
Efferent: Parasympathetic pelvic sacral nerve.
Centre: Sacral 2,3,4 in the spinal cord.
Afferent: Parasympathetic pelvic sacral nerve.
Receptors: Stretch receptors in the wall of bladder.
Stimulus: Increase Intra vesical pressure by accumulated urine (400 ml).
Table 4.3: Innervations of urinary bladder:
Somatic
Supply the external sphincter and Allows voluntary control on micturition.
No ganglia. Direct to organ.
AHCs of sacral (S 2,3,4) to form Pudendal nerve.
sympathetic
(Delay micturition)
Contraction of the internal sphincter. .
Relaxation of the bladder wall.
Inferior mesenteric ganglia
LHCs of lumber (L 1,2) to form Lesser splanchnic nerve.
Parasympathetic
Relaxation of the internal sphincter. (Micturition).
Sustained contraction of the bladder wall.
Relay
Terminal ganglia inside bladder wall.
Origin
LHCs of sacral (S 2,3,4 ) to form Pelvic sacral nerve.
It is visceral, central, unconditioned (inborn), spinal reflex with voluntary control.
Renal handling of FLUID, ELECTROLYTES AND ACID BASE BALANCE REGULATION
Renal Handling of Hydrogen & Bicarbonate (Acid-Base Regulation)
Factors affecting H+ secretion:
Aldosterone hormone: causes Na+ reabsorption, inc.H+ secretion & HCO3 reabsorption --> Alkalosis
Carbonic Anhydrase enzyme: dec. CA --> dec.H+ secretion & acidosis.
Cl- secretion: dec. Cl- secretion (retained in plasma) -->inc.H+ secretion & HCO3 reabsorption --> acidity.
K+ secretion: inc.K+ level -->inc.its excretion -->dec.H+ secretion & HCO3 reabsorption--> acidosis.
Plasma content of CO2: increaseCO2 --> decreaseH+ secretion.
Importance of H+:
H+ ion conc. affects many hormones as insulin and epinephrine & many drugs as digitalis.
H+ ion concentration affects other ions level as K+.
Change in H+ conce-->structral changes of protein
H+ ions bind to some enzymes and contractile molecules affecting their activities.
Sources of H+ in the body:
Hydrolysis of high-energy phosphate bond of ATP or CP.
Anerobic glycolysis in muscle leads to lactic acid accumulation.
Ingestion of acids as lemon or acidifying salts as NH4Cl.
Oxidation of sulphur & phosphorus in the proteins and lipids
Oxidation of carbon in organic food substances
Renal handling of HCO3-:
In late DCT & collecting ducts:
Ammonium salts formation in the proximal & distal tubules: Steps:
Net result:
For each H+ ion excreted also one NaHCO3 is added to blood giving alkaline tide.
Ammonia traps H+ & excretes it in urine as ammonium salts (If H+ is not removed the pH in urine will decrease (till 4.5) → no further H+ secretion despite the high H+ conc. gradient → this is called life-saving adaptation mechanism).
The amount of ammonium salts excreted in urine depends on activity of glutaminase enzyme & H+ secretion that increased in cases of chronic acidosis.
Then ammonium in the lumen either combines with:
Phosphate group (of Na H2PO4 to form Na + cation and ammonium phosphate salt(NH4H2PO4 )
NH4H2PO4 is excreted in urine and Na+ is reabsorbed forming NaHCO3
Cl of NaCL to form cation and ammoniu Na + m chloride salt (NH4Cl
NH4Cl is excreted in urine
In the lumen: Ammonia (NH3) + H+ (secreted) reconstructed to ammonium (NH4+) which is trapped in the lumen and not re-diffused to blood (ammonia trapping mechanism). It is estimated that about 40mEq of H+ ion combines with NH3 are excreted/day.
H+ is secreted to the lumen by active proton (ATP-driven) pump present on the intercalated cells. However, ammonia (not ammonium) diffuse rapidly, because it is lipid soluble into tubular fluid (if urine is acidic) or diffuse to blood (if urine is alkaline).
Metabolic reactions in the renal tubular cells produce ammonium (NH4+) which is in equilibrium with NH3 (ammonia) + H+
Formation of acid phosphate:
It associated with Cl- excretion.
High gradient as H+ can be excreted against high conc. Gradient 1000 folds. (pH in CD = 4.4).
Low capacity by which only 5% of H+ excreted.
The net result:
H+ excreted in form of acid phosphate in the urine.
NaHCO3 added to blood.
Step 4: HCO3- formed inside the cell moves passively to interstitial fluid where bind with actively pumped Na+ to form NaHCO3 (alkaline tide) in blood.
Step 3: In the lumen: H+ + Na2 HPO4 (dibasic phosphate, alkaline) → Na+ + NaH2PO4 (monobasic phosphate, acid).
Step 2: H+ is secreted to the lumen in exchange with Na+ (from filtered Na2HPO4) by secondary active transport (Na+/H+ counter-transport) at the luminal border. Then Na+ actively transported to interstitial fluid by Na+/K+ counter-transport through the basal membrane then to blood.
Step 1: In tubular cells CO2 enters from blood inside the cell to CO2 + H2O CA H2CO3 H+ + HCO3- .
In the intercalated cells of DCT & collecting duct, H+ secretion mechanisms is either dependent on Na+ (formation of acid phosphate) or independent of Na+ (formation of ammonia).
In the PCT
This mechanism is characterized by:
No Tm (tubular maximum) for HCO3- reabsorption. but when plasma HCO3- concentration is high (above 26-28 meq/L = renal threshold for HCO3-) → HCO3- appears in the urine and the urine becomes alkaline.
In PCT, H+ secretion is dependant on tubular Na+ reabsorption (while in DCT & CD, H+ secretion mechanisms is either dependent or independent of Na+).
Occur in thick loop of Henle & part of DCT.
HCO3- reabsorption is an active process since it requires H+ secretion & carbonic Anhydrase enzyme.
High capacity because 100% of NaHCO3- is reabsorbed & 95% of H+ secreted occurs by this mechanism.
Low gradient as H+ secretion stops if H+ concentration in lumen becomes 3-4 folds as in PCT cells.
For each H+ ion secreted, one Na+ ion & one HCO3- ion are reabsorbed to interstitial fluid.
Step 4: Formed HCO3- inside the cell moves passively through basal border to interstitium → bind Na+ → NaHCO3.
Step 3 (intra-luminal): Secreted H+ combine with the filtered HCO3- by the help of CA enzyme in the brush luminal border of the PCT cells → H2CO3 → H2O & CO2 (which diffuses into the tubular cells again).
Step 2: H+ is secreted to the lumen in exchange with Na+ (from filtered NaHCO3) by secondary active transport (Na+/H+ counter-transport) & then Na+ diffuses to blood.
Step 1(intracellular): CO2 of blood & of tubular fluid diffuses into cells of PCT → CO2 bind with H2O in presence of Carbonic Anhydrase, CA enzyme → H2CO3 → ionized forming HCO3- + H+.
Renal tubules are poorly-permeable to HCO3-. However, it is reabsorbed in the form of CO2 (highly permeable)
This reabsorption is affected by the acid base balance:
Acidosis → complete HCO3- reabsorption.
Alkalosis → increase excretion of HCO3- & urine becomes alkaline (normal urine is acidic PH=6)
More than 99% of HCO3- is reabsorbed by the kidney especially in PCT.
Bicarbonate HCO3- is the normal alkali reserve in the body which must be kept constant at a concentration of 26-28 mEq/litre at arterial PCO2= 40mmHg.
Control of ECF Volume
Blood and ECF volumes are controlled by:
Nervous and Humoral Factors:
These are short-term mechanisms controlling blood volume in acute conditions but for chronic conditions their effect will be no more than 5-10%.
Role of renin angiotensin system:
Angiotensin converting enzyme (ACE) in lungs and other tissues converts angiotensin I to angiotensin II.
Angiotensin II leads to:
Vasoconstriction Periphral--> resistance-->Increase arterial blood pressure
Release of aldosteron that increase water and salt retention
Release of ADH that increase water retention
Thirst and stimulation of salt appetite center. This lead to increase water and salt intake
Direct renal effect causing salt and H2O retention.
Renin will convert angiotensin (which is an alpha 2 globulin manufactured in liver) to angiotensin I.
Role ADH: excessive ADH leads to increasing water retention which inctreases arterial blood pressure which leads to excreation of excess volume by kidney so, blood volume is not increased more than 5-10%.
Role of aldosterone: Aldosterone causes strong Na+ reabsorption from late DCT and CD. This increases blood volume by 10-20% that lead to increasing blood pressure at the first and second day of increased aldosterone level due to Aldosterone escape phenomenon:
Aldosterone escape phenomenon:
Effect
Excess potassium excretion and impairment of potassium concentration in the body fluids. Thus, aldosterone is even more important as a regulator of potassium concentration than it is for sodium concentration.
Body escapes Na+ retaining effect of aldosterone due to increased ECF volume which stimulates ANP release leading maintenance of sodium balance.
Causes: marked increase in aldosterone secretion
Role of atrial natriuretic peptide (ANP): +& H2O excretion by kidney from 3to10 folds in acute cases, but in chronic diseases, its effect is slight.
Role of baroreceptors and stretch (volume) receptors:
Baroreceptors (in big arteries) and stretch receptors (in atria and veins) are stimulated by increasing blood volume. When paro receptors are stimulated they inhibit sympatetic tone so the renal arterioles are dilated which lead to increasing GFR and urinary output This is called volume reflex.
Pressure Natriuresis and Pressure Diuresis:
The most important mechanism for controlling blood volume (and secondary ECF volume as well) is the effect of blood volume on the arterial blood pressure and then the effect of arterial blood pressure on the urinary excretion of salt and H2O.
Control of Blood and ECF Volumes
Regulation of water content in urine:
Role of ADH
At maximal ADH secretion: whole length of MCDs becomes water-permeable → 4.7 % of water is reabsorbed (instead of normal 4.2%) → total water reabsorption of 99.7% → urine volume about 0.5 L/day with osmolality = 1400 mosmol/litre.
Occurs in cases of
Decrease water-permeable area in CDs → Decrease H2O reabsorbtion → excretion of a large volume of urine with low osmolality.
Urine volume is about 23.3 litres/day (because the normal osmotic load =700 mosmol is excreted at a concentration of 30 mosmol/litre → 700/30 = 23.3 approx).
In complete absence of ADH, urine osmolality will be 30 mosmol/L.
There is excretion of a large volume of dilute urine with an osmolality Less than 80 mosmol/L
While, Na+ reabsorption is continuous → Decrease osmolality of the tubular fluid in CCDs to 90 mosmol/L (normally, isotonic)
Late parts of DCTs & whole length of the CDs become water-impermeable → marked decrease in H2O reabsorption
Diabetes insipidus (pathological decrease ADH secretion):
Drinking large amounts of water.
At the low rate of ADH secretion
At high rate of ADH secretion:
Increase MCDs H2O-permeable parts → increase water reabsorbtion → excretion of concentrated urine with high osmolality.
Occurs in cases of hypovolaemia (e.g. haemorrhage) & blood hypertoncity (e.g. due to excessive salt intake).
At the normal rate of ADH secretion:
Total water reabsorption of about 99.2% & urine volume = 1.5 L/day with osmolality = 400 mosmol/litre (mechanism of urine concentration).
10% of H2O is reabsorbed in cortically collecting ducts (CCDs) & 4.2% in medullary collecting ducts (MCDs).
ADH is synthesized in the hypothalamus, stored in posterior pituitary & released due to many factors especially ↑ plasma osmolality which is detected by osmoreceptors of the hypothalamus.
The final adjustment of the urine volume & osmolality (concentration) depends only on the extent of facultative water reabsorption in the CDs, which is determined by 2 main factors:
Hyper-osmolality of the medullary interstitium: which developed by the counter current mechanism, causing passive water reabsorption from the CDs into the renal medulla.
ADH blood level: ADH make CDs (& DCTs to little extent) highly water permeable.
Urine volume may reach up to 20 L/day of Osmolarity = 50 mosmol/L or be reduced to 500ml/day with a concentration of 1200 mosmol.
It is the ability of the kidney to excrete either concentrated or dilute urine.
From 180 litres plasma filtered/day in both kidneys, only 1.5 liters of urine are excreted i.e. 99% of water is reabsorbed.
This occurs as follows:
Water reabsorption in the DCT & collecting tubules:
In late portion of DCT & collecting ducts:
This is called facultative water reabsorption i.e. depends on ADH ADH acts on H2O channels (aquaporine-2) present in principal cells of collecting tubules → increase luminal membrane permeability to H2O.
10% of water is reabsorbed.
In the 1st portion of DCT: about 5% of filtered water is reabsorbed (This segment is considered as continuation of thick ascending limb of Henel’s loop i.e., relatively impermeable to water & allow pass of solutes).
Water reabsorption in the loop of Henle:
Thin & thick portions of the ascending limb are impermeable to water but allow some solutes to pass out to medullary interstitium → fluid pass into DCT becomes hypotonic (= 100 mosmol/liter).
Thin descending limb is permeable to water but much less permeable to solutes → tubular fluid becomes hypertonic (= 1200 mosmol/L at the tip of the medullary pyramid).
Another 15% of water is reabsorbed in loop of Henle due medullary hyperosmolality.
Water reabsorption in PCT:
Water reabsorption in PCT is helped by presence of water channels called aquaporin.1 which are located in the luminal border of cells.
This mechanism is called obligatory water reabsorption because it is independent of ADH effect.
This reabsorption is passive i.e. as a result of active transport of other solutes (NaCL, glucose & amino acids) which create a high osmotic pressure in the renal interstitium.
About 70% of water is reabsorbed in PCT.
Renal Handling of Calcium & Phosphates
Non-reabsorbed amount of phosphate is used in the tubular fluid in DCT to buffer H+ ion.
In the PCT, under effect of Parathormone: inhibits phosphate reabsorption in same time of increasing Ca2+ reabsorption → keep solubility product constant.
Forms of phosphate in blood:
Organic form as ATP & creatine phosphate, important for energy supply & pH buffers.
Inorganic form as calcium salts in bone and teeth (about 85%)
Renal Handling of Calcium:
Ca2+ reabsorption
The factors that affect Ca2+ reabsorption are:
Plasma concentration of phosphate
Increase rate of Na+ reabsorption: → Increase Ca2+reabsorption by PCT.
Dietary calcium intake: Increase Ca2+ intake → Increase Ca2+ secretion & vice versa.
Parathormone hormone: → Increases Ca2+ reabsorption in DCT & loop of Henle.
99% of filtered Ca2+ is reabsorbed as follow:
DCT 10%
loop of Henle 25%
PCT 65%
Importance of calcium: it is essential for:
Blood coagulation.
Many hormone secretions are Ca+ dependant.
Muscle contraction (all types of muscles).
Controls cell membrane permeability.
Bone and teeth formation.
Activation of many enzymes.
Excitability of nerve and muscle.
Forms of Ca2+ in blood: Blood calcium level ranges = 9-11 mg/100ml & present in 3 forms:
Bound with other anions (5%) as citrate & phosphates, can be filtered with ionized form.
Bound to plasma proteins (45%) as a pool for the ionised amount & cannot be filtered.
ionized form (50%) → performing most of Ca2+ functions in the body.
Renal handling of potassium and potassium balance
Factors that affect potassium excretion:
Factors that Decrease K + excretion
acu te Increase in H+ concentration inside the distal convoluted tubules by suppression of the activity of Na+, K+ ATPase pump as well as the competition for Na + in the tubular fluid
Amiloride drug by inhibiting Na channels.
Endothelins, IL1, PGE 2 5. , ANP
Decrease tubular flow rate through the distal portions
Decrease Aldosterone hormone
Decrease K + intake
Factors that increase K + e xcretion
Chronic acidosis which decrease Na + & water reabsorption by PCT → Increase tubular flow rate to distal tubules
Some diuretics
Increase excretion of anions as Cl , HCO 3-- & HPO .
Increase tubular flow rate through the distal nephron
Increased Aldosterone hormone
Increase K + intake
Excreted K+ is derived from secretion rather than from filtration as follows:
↑ H+ secretion → ↓ K+ secretion.
Intracellular migration of Na+ → ↓ potential difference across the tubular cell → ↑ movement of K+ into the tubular lumen.
At principal cells Na+, K+ ATPase pumps Na+ outside basilar membrane & K+ to inside the cell then it diffuses out to the lumen.
K+ is secreted in these sites by the principal cells in exchange with Na+ by counter transport under the effect of Aldosterone hormone.
Mainly in DCT & cortical collecting tubules.
K+ load = 760/mEq per day. This amount is completely reabsorbed as follows:
10 % is absorbed from cortical collecting duct only if Aldosterone is absent.
25% is reabsorbed by secondary active co-transport with Na+ & Cl- in the thick ascending limb of the loop of Henle (1 Na+, 1 K+, 2Cl-).
65% is reabsorbed by the PCT.
The most important functions of potassium are:
Cardiac contraction, gland secretion and other body functions, which are all preceded by action potential, are K+ dependent.
Helps glucose transport inside cell from extracellular compartments.
Tissue repair & growth are K+ dependant.
Maintains electrical activities of the cell as the resting membrane potential & the depolarization & repolarization processes.
Controls the osmotic pressure inside the cells & regulate intracellular fluid content.
Accurate regulation of K+ balance is done mainly by the effect of Aldosterone on the kidney.
K+ is the chief intracellular cation (150mEq/L) and its ECF concentration is (4.2mEq/L)
More than 99% of the filtered chloride are reabsorbed and this reabsorption may be either:
Active in the thick ascending limb of Henel’s loop (Na+, K+ & 2 Cl-).
Passive in PCT & collecting tubules secondary to Na+ reabsorption.
Chloride ions are the main extra cellular anion & it equals about 104 mEq/L.
Renal handling of PROTEINS & AMINO ACIDS
Renal handling of UREA & URIC ACID (UA)
Writen
Renal handling of GLUCOSE
Control of ECF Osmolality (Tonicity)
When the ECF Osmolality Decreases: (Over-hydration or hypotonic dehydration)
In such cases, the ECF osmolality is increased to the normal level by the following mechanisms:
Increased salt intake (salt craving):
This occurs due to stimulation of the salt appetite center. It also helps to increase the ECF osmolarity.
Decreased thirst sensation:
This occurs due to deficient stimulation of the thirst center and as a result, the desire for drinking is reduced. Thus, water intake is decreased (which helps to increase the ECF osmolality).
Inhibition of ADH secretion:
This occurs due to deficient stimulation of the osmoreceptors, and maximal inhibition occurs in an ECF osmolarity of 285meq/liter. As a result of lack of ADH secretion, its blood level is reduced, thus the renal CDs become water-impermeable and excessive amounts of water are lost in the urine (which helps to increase the ECF osmolality).
When the ECF Osmolality Increases: (hypertonic dehydration)
The ECF osmolality is returned to the normal level by the following mechanisms:-
Decreased salt (NaCL) intake:
which is also located in the anterior hypothalamus close to the thirst centre at the AV3V region. This centre is inhibited when the ECF osmolality increases, thus the salt intake is reduced which tends to decrease the ECF osmolality.
The desire for salt intake is controlled by a centre called the salt appetite centre,
Increased thirst sensation:
Excitation of the osmoreceptors occurs secondary to intracellular dehydration (due to outward diffusion of water from these cells by the hypertonic ECF). Such cells are also stimulated when their K+ content is excessively decreased (which reduces their volume).
Increased secretion of ADH:
By stimulating osmoreceptors in the AV3V region of the anterior hypothalamus (= thirst centre) which are probably the same osmoreceptors that induce ADH secretion. The thirst sensation leads to drinking and the increased water intake also tends to decrease the ECF osmolality.
The increased osmolality stimulates certain receptors in the anterior hypothalamus called osmoreceptors, which are located outside the blood brain barrier along the anteroventral border of the 3rd ventricle (in an area called the AV3V region). These receptors discharge to the supraoptic nucleus, which in turn stimulates release of ADH from the posterior pituitary gland. This hormone causes water retention in the body by increasing its absorption from the renal CDs that tends to decrease the ECF osmolarity.
The normal osmolality of ECF is ranged from 285-to-295 mOsm or mEq/litre (for ease 300 mOsm/L). It is determined by its water and electrolyte contents particularly Na+ (which represents more than 90% of the electrolyte content of this fluid) and the control systems operate for its regulation are:
Salt appetite mechanism.
Thirst
ADH (vasopressin).
Renal handling of Na+:
Events that occur inside PCT:
Remaining tubular fluid is isotonic (300mosmol) but slightly acidic (pH resistance-->Increase arterial blood pressure
Prostaglandin I2 (PGI-2)
Although, these nervous and humoral factors affect blood volume strongly in acute cases, yet their role in long term conditions does not exceed 5-10%. This slight effect of blood volume have a considerable effect in long term arterial blood pressure level
i.e., these factors affect arterial blood pressure more significantly than blood volume as slight changes in blood volume affects cardiac output markedly leading to marked changes in arterial blood pressure
Is released in case of
Decreased flow on distal tubules to macula densa.
Decrease affrent arteriolar blood pressure-->decrese GFR glomrular filtration rate
Increased sympathetic activity and catecholamine release.
Reabsorption & synthesis of NaHCO3
Absorption of CL- & secretion of H+ ions in the 2nd half of PCT.
Co-transport of K+, glucose, amino acids & other organic acids at the 1st half of PCT.
70% of water load is reabsorbed = obligatory water reabsorption.
70% of Na+ load is reabsorbed.
Na+ reabsorption in the distal convoluting & collecting tubules (10%) 10% of Na+ is actively reabsorbed, in exchange with H+ or K+ by the help of Aldosterone hormone.
Factors controlling Na+ reabsorption: The amount of Na+ excreted per day may be as low as 1mEq/day to as high as 400mEq/day. The factors controlling are:
NB: The most important factor for controlling Na+ reabsorption is Aldosterone which affects this ion not only in kidney tubules but also in intestine & sweat glands.
Diuretics
Aldosterone antagonists (Aldactone) → antagonise Aldosterone → Decrease Na+ reabsorption from DCT
Loop diuretics (Lasix) → Decrease Na+ reabsorption from Henle's loop
Osmotic diuretics as mannitol→ Decrease Na+ reabsorption from PCT
Effect of ABP:
This mechanism is independent of nervous or hormonal effect.
Increase ABP above 180mmHg → increase Na+ excretion & urine output “pressure diuresis”.
Glomerulotubular balance:
It is an intrinsic mechanism which is independent of any nervous or hormonal factors, occurs mainly in PCT & to less extent loop of Henle.
Increase GFR → increase tubular load of any substance → increase its reabsorption to prevent overloading of the distal tubules with these solutes.
Hormonal factors:
Atrial naturetic peptide (ANP)
Sex hormones (estrogens).
Glucocorticoids
Aldosterone
Amount of NaCL intake per day: increase intake → increase Na+ reabsorption & excretion (& vice versa).
NB: Na+ reabsorption is active along the nephron except in thin ascending part of loop of Henle.
Na+ reabsorption in the loop of Henle (20%)
Note: Thin descending part: The only part in the nephron in which Na+ is not reabsorbed (also this part is freely permeable to H2O → hypertonic tubular fluid).
Thick ascending part: active reabsorption of 20% of Na+ by co-transport protein carrier (1Na+, 1K+ & 2Cl-) mechanism (also this part is poorly permeable to water→ fluid leaving this thick part is hypotonic).
Thin ascending part: passive reabsorption of Na+
Na+ reabsorption in PCT (70%). About 70% of Na+ load is reabsorbed in PCT
At baso-lateral border: Transport of Na+ to interstitium fluid characterized by:
1ry active transport using active Na+- K+ pump
This reabsorption results in:
Passive diffusion of Cl- (in 2nd half of PCT due to ↑Cl- concentration).
Active co-transport transport of glucose, amino acids, HCO3- & other organic acids (these substance are carried by same carrier of Na+).
Passive reabsorption of 70% of water “obligatory water reabsorption” because of the high osmolality created by Na+ reabsorption.
To maintain the intracellular negativity in relation to luminal fluid and ↑ Na+ entry to the cell, K+ ions diffuse back again to the interstitium helped by concentration gradient & high permeability of cell membrane
Against its electrochemical gradient (for each 3 Na+ pumped out only 2K+ ions are carried in).
At the luminal border: Na+ is transported from lumen to inside cells by facilitated diffusion under effect of:
needs carriers.
Electrical gradient (in lumen – 3 mv & inside cell –70 mv).
Concentration gradient.
Na+ reabsorption in different parts of renal tubules
Na+ reabsorption is associated with transport of many other substances as glucose, amino acids, H2O, H+, Cl-, HCO3- , and K+.
It is the major function of the kidney to reabsorb Na+; 80% of O2 consumption by the kidney is used for both Na+ & Cl- reabsorption.
Functions of sodium in the body
Bone formation
Controlling release of many vital substances in body as renin & Aldosterone.
Skeletal & smooth muscle contraction by releasing Ca++ from sarcoplasmic reticulum.
Formation of resting membrane potential, action potential & conduction of nerve impulse.
Keeping volumes of both extracellular fluid & blood constant → maintains normal ABP.
Small amount are excreted in sweat & stool (only 4%).
Dietary intake of Na+ = 4-20 gm/day, If NaCL intake is increased its excretion in urine will increase (& vice versa)
Body content of Na+ = 92 grams present in:
Exchangeable form is found in extracellular fluid (46g) & has strict homeostasis.
Non-exchangeable form (35 g), found in bone.
Na+ is the chief cation in the extracellular fluid (11g only is in intracellular fluid).
Low plasma levels of ADH diminish efficiency of urea to create high osmolality in the renal medulla.
Urea cycle add about 500 mosmol/litre to the renal medulla → important role in urine concentration (especially with high protein diet as it give large amount of urea).
Then, urea enter again to the lumen of the descending & thin ascending parts of Henel’s loop to re-circulation again and again till it reaches the medullary collecting tubules to start a new cycle and so on.
Water reabsorbtion from the medullary collecting tubules (by the high osmolality of renal medulla) → marked elevation in urea concentration → diffuses to renal interstitium (helped by ADH) → increase osmolality in renal medulla.
Other parts are impermeable to urea.
The parts that are permeable to urea are
The lower thin descending & the thin ascending limb.part of Henle’s loop
Collecting tubules.
Re-circulation of urea has a role in hyper-osmolality of renal medulla
Countercurrent exchanger Mechanism:
Steps of counter current exchanger mechanism:
So, vasa recta keeps the high tonicity of the medulla by 2 mechanisms:
Reabsorption of excess water reaching the medulla to the blood.
Adjust removal of NaCL from medulla by blood flow.
2
water that leaves the descending loop of Henle & the collecting tubules is reabsorbed (due to increased concentration of plasma proteins)
Water pass to the hypertonic medulla ( because the hydrostatic pressure of blood in descending limb is higher than the osmotic pressure of plasma proteins
1
ascending limb of vasa recta
NaCL & urea diffuse out to the medullary interstitium . (high concentration in the vasa recta)
descendin g limb of vasa recta:
NaCL & urea diffuse from renal medulla to the blood (high concentration in the medulla)
It induces absorption of 20% of NaCL & 15% H2O loads inside the vasa recta to general circulation.
Vasa recta is a U shaped long thin capillary loop that supply the renal medulla & run adjacent to the Henel’s loop of juxta medullary nephrons.
It is the function of vasa recta to Maintains the medullary hypertonicity.
The third step:
Action: Some of NaCL diffuses passively out the to the interstitium results: Marked increase the osmolality of medulla. Then repetition of the first step & so on.
Site: thin portion of the ascending loop of Henle
The second step:
The osmolarity of fluid at the bottom of the loop =1200 mosmol/L.
Increasing of Na + and other ions concentration
Reabsorption of water from the tubular f luid in to the hypertonic medulla by osmosis.
thin descending part & CD
The first step:
Results
Action
This is not followed by water reabsorption
because the whole ascending limb is nearly impermeable to water.
Active co transport of Na+,K+,2Cl- (or other ions like Ca 2+ + & Mg2+ ). from the
thick ascending part of Henle’s loop
ميكرو
UROPATHOGENS
CANDIDA ALBICANS
ENTEROCOCCUS SPECIES
STAPHYLOCOCCI
Coagulase negative staphylococci (CONS)
Staphylococcus aureus
NON-FERMENTATIVE GRAM-NEGATIVE BACILLI
Acinetobacter
Multiple antibiotic resistance.
Ability to survive on the surfaces of hospital facilities and equipment for weeks.
Ability to resist desiccation & disinfectants.
Powerful biofilm production.
Pseudomonas aeruginosa
ENTEROBACTERACIE
Proteus species
Adhesins and swarming promote colonization and biofilm formation.
The production of a potent urease is associated with urinary stones because it splits urea to produce ammonia, rendering the urine alkaline. An alkaline urine pH favours the crystallization of calcium- and phosphate-containing stones.
Klebsiella species.
Capsule is the major virulence factor.
Virulence factors of uropathogenic E. coli (UPEC):
Production of haemolysins which cause kidney damage.
Lipopolysaccharides of cell wall.
Capsular polysaccharide (K) antigens which inhibit phagocytosis.
Adhesins: Type 1 fimbriae & type P. fimbriae (pyelonephritis-associated pili (PAP)) promote attachment and invasion of renal epithelium.
(Refer to practical parts for further details)
Other Parasitic Diseases of Urinary Tract
Urogenital Myasis
There may be severe pain due to obstruction of urinary passages by the larvae. Mucus, blood and sometimes larvae are discharged with urine; e.g. Sarcophaga, Musca and Fannia.
It is the invasion of human tissues by larvae of dipterous flies. Larvae enter through orifices of urinary or reproductive systems.
Filariasis
prolonged lymphatic obstruction giving different degrees of lymphatic varices in the various affected organs. Rupture of these varices may cause chyluria (if in urinary passages), chylocele or lymphocele (if in tunica vaginalis of the testis).
Filariasis involves lymphatic system. Obstruction give rise to elephantiasis
The intermediate host is mosquitos as Aedes, Anopheles and Culex species.
Trichomoniasis
It is a sexually transmitted infection caused by the flagellated protozoan, Trichomonas vaginalis, patients are generally presented with urethritis.
Cystic Echinococcosis
Isolated renal disease is rare, the other involved organs in the genitourinary system are urinary bladder, prostate, testes, and seminal vesicules; The most common symptoms are palpable mass, hematuria, pain and rupture of cyst lead to presence of hydatid scolices in urine.
The most affected organs are the liver and lung while kidneys are less affected sites.
Infection of human tissues by "hydatid cyst", the larval stage of Echinococcus granulosus.
ANATOMY OF URETER
Radiologically: ureteric stone is identified near the tip of the transverse process of lumbar vertebrae, opposite the sacro-iliac joint or medial to the ischial spine
Ureteric colic: It occurs due to obstruction of ureteric lumen by a stone. The referred pain of ureteric colic is related to the cutaneous areas innervated by the same spinal segments as that of the ureter, i.e., T12–L2. Pain of ureteric colic commences in the loin, shoots downward and forward to the groin and then into the scrotum or labium majus
Ureteric stone usually migrate from the kidney and impacted in one of the normal anatomical constrictions
The parasympathetic supply of ureter is derived from S2–S4 spinal segments through pelvic splanchnic nerves. The afferent fibres travel with both sympathetic and parasympathetic nerves.
The sympathetic supply of the ureter is derived from T12–L1 spinal segments through renal, aortic, and hypogastric plexuses.
BLOOD SUPPLY The ureter derives its arterial supply from the branches of all the arteries related to it. :
LYMPHATIC DRAINAGE The lymph from the ureter is drained into lateral aortic and iliac lymph nodes.
The venous blood from the ureter is drained into the veins corresponding to the arteries.
The important arteries supplying ureter from above downward are (Fig. 4.4)
Uterine
Middle rectal.
Vesical (superior and inferior)
Internal iliac
Direct branches from aorta
Testicular or ovarian.
SITES OF ANATOMICAL CONSTRICTIONS
The lumen of the ureter is not uniform throughout and presents constrictions at the following sites (Fig. 4.3):
At uretric orifice at the urinary bladder
At the uretero-vesical junction (i.e., where ureter enters into the bladder).
At the pelvic brim where it crosses the common iliac artery.
At the pelvi-ureteric junction
COURSE
The pelvic part of the ureter crosses in front of all the nerves and vessels on the lateral pelvic wall except vas deferens, which crosses in front of it. Near the uterine cervix, the uterine artery lies above and in front of it, a highly important surgical relationship (Fig. 4.2).
In the pelvis, the ureter first runs downward, backward, and laterally along the anterior margin of the greater sciatic notch. Opposite to the ischial spine, it turns forward and medially to reach the base of the urinary bladder, At the end, it enters the bladder wall obliquely where it narrows down, takes a sinuous course, and opens into the cavity of the bladder at the lateral angle of its trigone as ureteric orifice.
The ureter begins as a downward continuation of renal pelvis Then passes downward and slight medially on the psoas major. It enters the pelvic cavity by crossing in front of the bifurcation of the common iliac artery at the pelvic brim in front of the sacroiliac joint (Fig. 4.1).
MEASUREMENTS: Length: 25 cm (10 inches). Diameter: 3 mm. The ureter is generally divided into two parts: abdominal and pelvic. Each part is about the same length, i.e., 12.5 cm (5 inches)
The ureter is a retroperitoneal narrow, thick-walled, expansile muscular tube which conveys urine from the kidney to the urinary bladder.
ANATOMY OF URINARY BLADDER
RELATIONS
Superior surface:
In the female, it is covered by the peritoneum except for a small area near the posterior border, which is related to the supravaginal part of the uterine cervix. Here the peritoneum is reflected on to the uterine isthmus forming vesicouterine pouch.
In the male, it is completely covered by the peritoneum which separates it from: coils of the ileum, and/or sigmoid colon. Along its lateral borders, the peritoneum is reflected on to the pelvic walls.
The neck of urinary bladder
In female it is related to the urogenital diaphragm
In male it rests on the base of prostate.
It is the lowest and most fixed part of the bladder situated where the inferolateral and the posterior surfaces of the bladder meet. It is pierced by the urethra.
Base (posterior surface): is directed backwards. Its superolateral angles are joined by the ureters while its inferior angle gives rise to the urethra. Its relations differ in both sexes
In female: The base of urinary bladder is not covered by peritoneum and is related to anterior surface of body and cervix of uterus and upper part of vagina.
In male:
The triangular area between the vasa deferentia is separated from the rectum by rectovesical fascia (of Denonvilliers) (Fig.4.6)
The vasa deferentia lie medial to the seminal vesicles
Lower part is separated from rectum by the terminal parts of vasa deferentia and seminal vesicles.
upper part is covered by peritoneum and separated from rectum. by rectovesical pouch which contains loops of small intestine and sigmoid colon.
The apex is directed forwards towards the symphysis pubis. It is connected to umbilicus by the median umbilical ligament which represents the obliterated urachus. If this ligament is patent the umbilicus will discharge urine.
SHAPE & SURFACES: roughly pyramidal when empty, but spherical when distended. An empty and contracted bladder has an apex, base, neck, superior and two inferolateral surfaces. Four borders (anterior, posterior and two lateral) (Fig. 4.5).
CAPACITY: The mean capacity is about 220 ml. An amount of urine beyond 220 ml causes a desire to micturate. The filling of urine up to 500 ml may be tolerated but beyond this, it causes pain due to tension of its wall.
POSITION
In children, the bladder is an abdominopelvic organ. It begins to enter the enlarging pelvis at the age of six years but does not become a pelvic organ entirely until after puberty
situated behind the upper part of the symphysis pubis. When the bladder is empty it lies entirely within the lesser pelvis but when it becomes distended with urine, it expands upward and forward into the abdominal cavity.
بارا
Immune response to Schistosomes:
Concomitant immunity:
Complications of schistosomiasis:
Lung schistosomiasis (Bilharzial cor pulmonale): right-sided heart disease secondary to chronic lung disease. It occurs as a result of repeated embolism of ova into the pulmonary arterioles, S. haematobium (mainly), S. mansoni or S. japonicum (occasionally).
Central nervous system involvement: due to formation of granulomas around eggs embolised to C N S. Brain affection usually happens in S.japonicum owing to the small-sized eggs that can reach narrow cerebral vessels causing headache, epileptic fits, paraesthesia and poor vision. Lesions in the spinal cord may occur in S. haematobium and S. mansoni, leading to paraplegia.
Clinical Picture:
Chronic urinary schistosomiasis:
Early manifestations: “mainly inflammatory”
Late manifestations: “mainly fibrotic”
Fibrosis of the urinary bladder and ureters causes obstructive uropathy; Fig. (5.12) (hydronephrosis and pyonephrosis). Urinary calculi and bladder carcinoma may occur.
Dysuria (burning micturition), frequency & suprapubic pain.
Recurrent painless terminal haematuria is the cardinal complaint.
Acute schistosomiasis (Katayama syndrome) :
Mechanism: antibodies produced against schistosomula & adults cross-react with the huge amounts of soluble egg antigens (released from large number of eggs) at the time of oviposition leading to forming immune complexes that produce the previous manifestations.
Manifestations: serum sickness-like picture with sudden onset of fever & chills, urticarial, abdominal pain, nausea, vomiting, diarrhea, hepato-splenomegaly & lymphadenopathy and eosinophilia.
may occur about 6 weeks after the initial infection, coinciding with egg deposition, especially by S. mansoni and S. japonicum.
Cercarial dermatitis (swimmer's itch):
Manifestations: dermatitis (erythema & papules) and itching starting several hours after exposure to contaminated water and may persist for several days.
It tends to be more severe in infections with cercariae of non- human schistosomes (avian or bovine) due to their inability to complete the life cycle (unusual host), so,they die in the skin changing totally to antigens resulting in immune response.
It occurs infrequently among individuals living in endemic areas but is common among visitors and migrants.
Cercarial dermatitis is an IgE-mediated hypersensitivity response directed against penetrating cercariae.
Mechanisms
Another mechanism involving IgE & macrophages.
Antibody-dependent cell-mediated cytotoxicity (ADCC); Fig. (5.11): involving IgG & eosinophils.
It is a protective immunity against cercarial reinfection but adult worms of primary infection are unaffected. These adult worms evade the immune response by adding a layer of specific host antigens to their membranes
Immune evasion (escape) mechanisms of Schistosoma:
These mechanisms include:
Blocking antibody formation: - These are antibodies of little protective effect. They can attach to the parasite but can’t fix the effector cells of immune system. So, they occupy “block” the surface antigen sites on the newly infecting schistosomula making them unavailable for the effective IgE interfere with protective immunity.
Antigen shedding: Schistosomula continuously shed their surface antigens to divert the immune response away from them.
Antigen mimicry: Adult worms can produce surface antigens that are similar to human antigens to avoid recognition.
Schistosomula & adult worms acquire a layer of host molecules on their surfaces so that the host immune system considered them as if they are not foreign and consequently do not recognize the parasite as foreign.
These mechanisms explain:
The ability of adult worms to live for years in the blood vessels
The ability of schistosomula to migrate through the bloodstream to the liver.
These are the mechanisms that allow the parasite to survive within the host protected from the immune response.
Pathology and pathogenesis of Schistosomiasis
Pathogenesis of haematuria:
Late in the disease: due to ulceration of bladder mucosal lesions (nodules, polyps, sandy patches or carcinoma).
Early in the disease: due to disruption of bladder mucosa by S. hematobium eggs (with terminal spines) while leaving the body through urine.
Pathological lesions occur also in schistosomiasis due to immune complex deposition in various tissues especially kidney glomeruli .Immune complexes are formed from antigen –antibody combinations.
The resulting pathological lesions; Fig. (5.10):
Cancer bladder: late in the disease, squamous cell carcinoma may result. Fibrosis may induce hyperplasia and metaplasia, all of which are possible precancerous changes.
Sandy patches: develop when the submucosa becomes densely thickened by fibrous tissue containing large numbers of calcified eggs; and the mucosa becomes atrophic with a granular dirty yellowish appearance.
Nodules& polyps: develop when multiple granulomas coalesce together.
the disease passes into 3 stages; Fig.(5.9):
Fibrosis
Granuloma formation
Inflamation
Most of the pathological lesions in urinary schistosomiasis result from egg deposition in tissues .Soluble egg antigens (SEA) that diffuse out through the egg shell micropores into the surrounding tissues are:
Highly immunogenic : granuloma formation mainly in submucosa of urinary bladder, lower 1/3 of ureters& genital organs and it is a manifestation of delayed hypersensitivity through cell-mediated immune response. First granuloma is formed of Schistosoma egg surrounded by cellular aggregates of eosinophils, monocytes, lymphocytes, neutrophils, and plasma cells. Later on fibroblasts appear and predominate leading to fibrosis.
Highly irritant inflammation.
Eggs appear in urine about 8 weeks after infection
Paired worms then migrate to their final habitat against blood stream.
Schistosomula are carried by venous circulation to the right side of the heart ► lung ► left side of the heart ► systemic circulation ► hepatoportal circulation (liver) where maturation to adult stage & pairing of worms occurs.
During penetration, the cercaria leaves its tail outside, and its body only invades venous circulation of skin; now called (schistosomulum).
Man is infected by cercariae through skin penetration (while being in contact with infected water) or buccal mucous membrane penetration (while drinking infected water).
The cercariae (infective stage) then come out from snail & swim in water searching for final host (man).
The miracidium penetrates snail soft tissues & develops into 2 generations of sporocysts and the production of furcocercous cercariae.
After passing in urine; eggs will hatch on reaching fresh water releasing miracidia.
Miracidia swim in water searching for the specific snail intermediate host (Bulinus truncates).
Penetration of eggs through wall of intramural venule, submucosa & mucosa of urogenital tract into the lumen is helped by :
Pressure effect of egg spine.
Recoil of venule following retraction of female after egg laying.
Effect of proteolytic enzymes secreted by miracidium inside the egg and released through the egg wall micropores into the surrounding tissues.
Eggs may pass into one of three ways:
Other eggs embolize through systemic circulation to lung, CNS & other sites “ectopic lesions”.
Other eggs become trapped (arrested) in the walls of urogenital organs pathological lesions.
Some eggs succeed to penetrate into the urinary lumen pass with urine to the outer environment & can complete the life cycle.
The female worm proceeds furthermore (being thinner) to lay eggs in the intramural venules retracting forwardly after laying each egg leading to recoil of venule on the egg.
Paired adult S. haematobium worms live in the perivesical & pelvic venous plexuses. Male worm carries its female in the gynaecophoric canal and passes against blood stream toward walls of urinary bladder & lower 1/3 of ureters until male worm become wedged inside a narrow tributary blocking blood stream.
Body defense mechanism against PH change
Body defensive mechanisms against pH disturbances The body metabolism and muscle activities tend to add acids to the body fluids, hence we have an alkaline reserve in our body to oppose this tendency and maintenance of this pH depends on:
Slow mechanisms: renal & changes in cellular metabolism
Quick mechanisms: chemical & respiratory buffers.
Respiratory regulation of the pH. (1-12 minute) Respiratory system controls pH of body fluids by controlling CO2 tension in the arterial blood, which is the main source of H+ ions. - At pH 7.4 the ratio between HCO3 to CO2 = 20/1.
Chemical Buffers: (very rapid–in fraction of a second)
Yet, bicarbonate buffer is actually more important than all the
When strong base (NaOH) is added to plasma, it will combine with H2CO3 NaHCO3 (weak base) + H2O.
When strong acid (HCL) is added to plasma, it will combine with Na HCO3 NaCL (neutral) + H2Co3 (weak acid).
Examples
Protein buffer system:
It is a very important buffer and composed of plasma proteins, hemoglobin and intracellular proteins.
Intracellular protein :
It is a very important in the regulation of intracellular pH as it is the most plentiful buffer in the body
Hemoglobin
Hb plays a role in transport of CO2 as the following
At the lung: the reverse occurs i.e. reduced HB binds to O2 giving oxyHb and at the same time liberates up the hydrogen ion. These free hydrogen ions react with bicarbonate to form carbonic acid, which dissociates into H2O and CO2. The latter is removed by the lungs thus keeping pH constant. [Cl-shift phenomenon]
At the tissue: oxyHb gives O2 to tissue and converted to reduced Hb, at the same time CO2 diffuse to RBCs and converted to H+ and HCO3.This H+ is buffered by the reduced HB, preventing change the pH.
Hb has numerous imidazole groups of histidine residues which can dissociate liberating H+ and each one Hb molecule contains 38 histidine residues. Imidazole group is amphoteric substance (good buffer) as it has COOH and NH2 groups.
reduced Hb has greater affinity for H+ (strong buffer) than oxy Hb
The reduced Hb dissociate less than oxy Hb making the reduced Hb is weaker acid than oxy Hb
It is the most important buffer due to its high concentration (15gm%).
plasma protein:
It is of high concentration (7.4 gm%).In blood, proteins act as weak acids and they are negatively charged, thus they tend to dissociate (weakly) giving H+ ion and negatively charged proteinate ion.
Most buffers consisted of weak acids+salt of its base (acid-base buffer pair) e.g. H2Co3-NaHCO3. The relation between H+ conc. and the ratio of the buffer members is expressed by Handerson Hasselbach equation.
Hasselbach equation:
The effectiveness of any buffer system depends on:
The pKa of the buffer (the buffer is effective if its pKa is equal to the pH and this is preserved if the concentration of the salt & acid is equal as in equal concentration of HCO3- and dissolved CO2 the pH of the solution will be equal to its pKa since log “1” = zero).e.g.
The concentration of the buffer.
By substances which minimize changes in pH of solution when acids or bases are added.
Consequences of Intracellular pH disturbances:
Alkalosis stimulates dissociation of plasma proteins, which then bind more calcium and thus reduce Ca2+ activity in plasma. Conversely, acidosis reduces Ca2+ binding of plasma proteins. On the other hand, bicarbonate binds calcium, reducing plasma Ca2+ activity. In metabolic alkalosis and acidosis the two effects are additive and elicit marked changes of plasma Ca2+ activity.
Acidosis decreases and alkalosis increases the oxygen affinity of hemoglobin (the Bohr Effect).
Acidosis decreases and alkalosis enhances the gap junction’s conductance, which in the heart modifies the conduction of the cardiac impulse.
In pulmonary arterioles, H+ elicits vasoconstriction, whereas in the systemic circulation H+ favors vasodilatation; alkalosis favors vasoconstriction, especially of cerebral vessels.
Acidosis may lead to a decrease of Ca2+ entry through Ca2+ channels, resulting for instance in reduction of cardiac contractility.
The K+ channels are activated by alkalosis and inactivated by acidosis.
For DNA synthesis and cell proliferation to occur, cell pH must not be acidic; Accordingly, a wide variety of growth factors activate the Na+/H+ exchanger to alkalinize the cell. Alkaline pH usually prevails in tumor cells.
Gluconeogenesis is inhibited by alkalosis and stimulated by acidosis.
Intracellular alkalosis stimulates and intracellular acidosis inhibits glycolysis and lactic acid formation.
HCO 3= 27 mEq/L
Pa Co2 = 40 mmHg (arterial)
pH = 7.4 (arterial), pH=7.35 (venous)
hydrogen ion concentration = about 40 nanomol/L (arterial blood),
The pH urine is 4.4 and that of arterial plasma 7.4, there is a difference of 3 pH units which correspond to a urinary concentration of hydrogen ions that is 1000 times greater than the concentration of hydrogen ions in arterial plasma
A change of one pH unit represents a tenfold عشر اضعاف change in actual hydrogen ion concentration.
The value of pH is inversely proportional تتناسب عكسيا to the concentration of hydrogen ions.
Types of solutions according to pH:
Acidic solutions: pH 7.
Neutral: The [H+] is 7.
The term pH is the negative logarithm of hydrogen ion concentration [H+]. Or it is the log of the base of H+ ion concentration.
Kidney
ROLE OF KIDNEY IN METABOLISM
لاحظ الفرق بين
Creatinine
Urine Excretion:
Causes of Creatinuria:
Pathological Causes:
Increased tissue breakdown e.g. diabetes, thyrotoxicosis, Cushing syndrome, diabetes mellitus.
Vitamin E deficiency.
All forms of myopathies and muscle dystrophy.
In males with hypogonadism (decreased androgens).
Physiological Causes:
In females: During pregnancy, owing to increased production by the fetus and after labour due to involution of uterus.
Children and infants: due to decreased androgens and small muscle mass.
Creatinine is the excretory form of creatine. This is related to the muscle mass, not affected by diet, and of complete endogenous origin.
In females
1.0 gm / day
In males:
1.5 gm / day.
Serum creatinine:
0.7 - 1.2 mg /dl for men.
0.5 -1 mg /dl for women.
It is break down product of creatine phosphate in muscle. Creatinine is cleared from the body by the kidney, so serum creatinine is an important indicator of kidney function.
Creatine
Biosynthesis of creatine:
In muscle, creatine is phosphorylated to creatine phosphate by creatine kinase(CK ), using ATP as the phosphate donor . Creatine phosphate is a high energy compound that can reversibly donate a phosphate group to ADP to form ATP. It provides energy to the muscle during the first few minutes of intense muscular contraction.
Clinical importance of creatine kinase (CK): Elevated level of plasma CK is indicative of tissue damage and can be used in diagnosis of myocardial infarction and muscular dystrophy.
Creatine is synthesized from glycine, arginine and S-adenosyl methionine. The biosynthesis occurs in two steps:
In the liver : Guanidoacetic acid by transmethylation is converted to creatine.
In the kidney : Transamidinase enzyme transfer amidine group from arginine to glycine to form guanidoacetic acid.
It is present in blood, brain, and muscle.
Creatine is methyl-guanidoacetic acid.
The Cori and alanine cycles These two important cycles are related to gluconeogenesis
Alanine cycle:
Pyruvate is used to produce glucose by gluconeogenesis.
In the liver, alanine is converted back to pyruvate.
Alanine diffuses to the blood an then taken by the liver.
Pyruvate formed from glycolysis in the muscles is converted into alanine by transamination.
Cori cycle:
The liver converts lactate into glucose by gluconeogenesis, which returns back to the blood to be utilized by muscles and RBCs for energy production.
The lactate produced by skeletal muscles and RBCs diffuses to blood and then taken up by the liver.
Regulation of gluconeogenesis 2ATP The key regulatory enzymes of gluconeogenesis are pyruvate carboxylase, phosphoenolpyruvate carboxykinase, fructose 1,6-bisphosphatase and glucose 6 phosphatase.
ATP and acetyl CoA:
Fatty acid oxidation is increased during fasting stimulates gluconeogenesis by:
Acetyl CoA production is increased. This stimulates pyruvate carboxylase(gluconeogenesis) and inhibits pyruvate dehydrogenase directing pyruvate towards gluconeogenesis rather than oxidation.
Production of ATP, which inhibits glycolysis (inhibition of phosphofructokinase-1) and stimulate gluconeogenesis (stimulation of fructose 1,6 biphospatase).
biphosphate. Low levels of fructose 2,6 biphosphate inhibit phosphofructokinase-1 (glycolysis) and activate fructose 1،6 biphosphatase(gluconeogenesis ).
Hormonal regulation
Glucagon: stimulate gluconeogenesis by inhibiting the formation of fructose 2,6
Insulin: inhibits the gluconeogenesis as it represses the synthesis of the key enzymes.
Glucocorticoids: stimulate gluconeogenesis by:
They induce the expression of transaminases.
They stimulate protein catabolism, thus increasing glucogenic amino acids available for gluconeogenesis.
They induce the synthesis of the key enzymes.
Energy cost of gluconeogenesis
For conversion of 2 molecules of pyruvate to one molecule of glucose, 6 high energy phosphate bonds are hydrolysed ( 4 ATP and 2 GTP ) as follow:
Sources for gluconeogenesis
Propionyl CoA can be derived from the catabolism of some amino acids as methionine, isoleucine and threonine.
Amino acids
Amino acids on deamination or transamination give pyruvic acid or intermediates of kreb's cycle( α -keto-glutaric acid , succinyl CoA). Both are converted into oxaloacetate which finally produce glucose.
With exception of leucine, all amino acids are either glucogenic or mixed (glucogenic and ketogenic).
Even-chain fatty acids cannot produce new glucose, since they yield only acetyl-CoA equivalents.
Vitamin B12 deficiency results in excretion of large amounts of methyl malonyl CoA in urine (methyl malonic aciduria).
Glycerol: Glycerol can be generated from hydrolysis of triacylglycerols to yield free fatty acids and glycerol. Glycerol is phosphorylated by glycerokinase into glycerol-3 phosphate which is oxidized to dihydroxyacetone phosphate. Adipose tissues cannot phosphorylate glycerol because they lack glycerol kinase.
Odd chain fatty acids The odd chain fatty acids are oxidized in β-oxidation producing acetyl CoA molecules and one molecule of propionyl CoA, which is converted to succinyl-CoA--> Fumarate - - > Malate - - > join common pathway of glucose.
NB
The last unit of B-oxidation of an odd-chain fatty acid, propionylCoA, can also enter gluconeogenesis.
The glycerol backbone of triacylglycerols is a gluconeogenic substrate
Mammals cannot convert fatty acids into glucose, as there is no enzyme to catalyse the reaction of acetyl-CoA into oxaloacetate.
Lactate: Lactate is converted into pyruvate by lactate dehydrogenase.
Steps
Are those of reversal of glycolysis, except for the 3 irreversible reactions. The gluconeogenesis pathway is not simply a reversal of glycolysis.
Thermodynamics favour glycolysis direction of glucose l pyruvate
The 3 irreversible reactions can be bypassed as follows:
Bypass III: Reversal of hexokinase (glucokinase) Reversed by glucose-6-phosphatase, which is present in the liver and kidney, but not in the brain and muscles. Thus, glucose produced by gluconeogenesis in the liver, is delivered by the blood stream to the brain and muscles. Glucose-6-phosphate +H2O -- >Glucose +Pi
Bypass II: Reversal of phosphofructokinase reaction This is reversed by fructose 1,6 diphosphatase enzyme. Fructose 1,6 biphosphate +H2O---> Fructose-6-phosphate +Pi
Bypass I: Pyruvate kinase reaction is reversed by dicarboxylic acid shuttle Pyruvate is transported into the mitochondria from cytoplasm as enzyme pyruvate carboxylase is present only in mitochondria (mitochondrial matrix). Carboxylation of pyruvate to form oxaloacetate in the presence of biotin as cofactor. Reaction is driven by ATP hydrolysis.
Reaction is driven by GTP hydrolysis.
Can occur in either matrix or cytoplasm
Oxaloacetate + GTP--> phosphoenolpyruvate + CO2 + GDP
Clears lactate produced by muscle and RBCs and glycerol produced by adipose tissues from the blood.
Glucose is the source of energy for brain and RBCs.
Maintain blood glucose levels in case of fasting more than 18 hours (liver glycogen is depleted after 12-18 hours).
Site:
Subcellular: cytosol and mitochondria.
Organs : liver and kidney (Renal cortex contributes about 10%). Muscle cannot participate in gluconeogenesis because it lacks glucose-6- phosphatase.
GLUCONEOGENESIS
Definition: Biosynthesis of glucose from non-carbohydrate sources.
Endocrinal role:
Production of erythropoietin. It stimulates red blood cell production in the bone marrow.
The kidneys convert 25 hydroxy vit D3 into 1,25 dihydroxy vit D3 (calcitriol), which is the active form of vit D and now considered as a hormone responsible not only for calcium absorption by the small intestine and makes it available for bone development, but also plays a role in various conditions e.g. diabetes mellitus, cancer , autoimmune diseases and cardiac diseases.
Remember: Carnitine is important in fatty acid metabolism.
The kidney is the major site of carnitine synthesis, with liver to a lesser extent.
Creatinine is excreted by filtration by the kidneys, and its level in the blood can be used to assess renal function.
Creatine phosphate spontaneously forms creatinine.
The renal cortex converts citrulline via arginine to creatine, which is used by skeletal muscle to store high-energy phosphate bonds as creatine phosphate.
The renal cortex is the only tissue other than liver that can perform gluconeogenesis. It has a capacity of up to 10% of total glucose generation.
Kidneys are histologicaly formed of
Parenchyma
URINIFEROUS TUBULES
It consists of:
Collecting system.
Nephron
Each nephron is composed of:
Nephron tubules
Acute Tubular Necrosis (ATN)
Results of ATN
Causes of oliguria in ATN: Both ischemia and toxins cause tubular and glomerular damage.
Clinical course of ATN
3 stages
Recovery phase—polyuric; BUN and serum creatinine fall; risk of hypokalemia and renal
Maintenance phase—oliguric; lasts 1–3 weeks; risk of hyperkalemia, metabolic acidosis, uremia
Inciting event
Types: Ischemic, Toxic
Causes of toxic ATN
contrast media
irradiation
organic solvents
poisons
Causes of ischemic acute tubular necrosis
Transfusion reactions.
Sepsis: Acute pancreatitis
Dehydration, burns.
Shock, Heart failure.
Severe hypotension.
Vascular obstruction
Definition: Acute renal disease affecting the renal tubules characterized by oliguria or anuria due to destruction of tubular epithelium. The condition is usually reversible, but may pass to acute renal failure.
Renal tubules do the following processes
Excretion: the amount of substances that are found in urine.
Urine contains H2O and products of drugs, toxic substances, urea, uric acid & creatinine.
Only 1 ml/minute of 125 ml filtered fluid is excreted as urine (in normal adult = 1500 ml/day).
Synthesis: the formation of new substances as ammonia (for H+ regulation).
Secretion: the movement of substances from blood surrounding the tubules (in peritubular capillaries) to the tubular lumen to be excreted with urine.
Reabsorption: the movements of substances from lumen of renal tubules crossing tubular cells back to the blood. 99% of the Glomerular filtrate volume is reabsorbed.
Include
Distal convoluted tubule.
Loop of Henle.
Proximal convoluted tubule.
Secretion of creatinine, iodine, and some drugs.
Reabsorption of most water (63%).
Reabsorption of sodium, potassium, and chloride ions.
Reabsorption of glucose, proteins, amino acids, phosphorous, calcium.
The lateral surface has many interdigitations.
The basal region has many long mitochondria and basal infoldings (associated with active transport).
Numerous canaliculi and pinocytotic vesicles are seen in the apical cytoplasm.
The apical surface has many microvilli (increase the surface for absorption from the lumen).
They have indistinct lateral membrane (interdigitations with adjacent cells).
They have basal acidophilic striations (mitochondria and basal infoldings)
They rest on distinct basement membrane.
They have apical acidophilic brush border (microvilli).
Pyramidal cells with round basal nuclei.
Lining cells:
In cross section, the tubule has a diameter of about 60µm with relatively narrow lumen.
It is the longest segment of the nephron (15mm) which begins at the urinary pole of the renal corpuscle in the cortex and ends at the loop of Henle.
Renal Malpighian corpuscle.
Blood Renal- Barrier
It filters the blood plasma in the renal corpuscle by filtration selectivity, permits small molecules to enter capsular space, and prohibits large one.
The slits between the pedicles of podocytes with their slit diaphragm.
Fused continuous (not fenestrated) basal laminae of both podocytes and endothelial cells
Fenestrated endothelium of glomerular capillary without diaphragm (Fig 1.12).
It is a filtration membrane separating blood in glomerular capillaries from glomerular filtrate in the lumen of Bowman's capsul
It is formed of:
Mesangial cells (Intraglomerular).
Factors affecting mesangial cells
Mesangial cells are relaxed by
PGE2
Dopamine
Activation of Cyclic AMP
Atrial natriuretic peptide
Platelet derived growth factor
Platelet activating factor
Thromboxane A2
Leukotrienes C and D
PGF2α.
Angiotensin II
Noradrenalin
Histamine
Endothelins
Mesangial cells are Contracted by:
They support capillaries in the areas where the basement membrane is absent or incomplete.
They regulate blood flow through the glomerular capillaries.
They synthesize and maintain glomerular basal lamina.
They are phagocytic cells.
There are two types:
Intraglomerular mesangial cells: (Fig 1.12).
They are enclosed in the basal lamina of the glomerular capillaries (positioned as the pericytes).
They are branched (stellate) cells with basophilic cytoplasm and dark nuclei.
Present between adjoining glomerular blood capillaries.
Extraglomerular mesangial cells:
Share the formation of juxtaglomerular apparatus (will be discussed).
Specific contractile cells that are found between two neighbouring capillaries of glomeruli.
Glomerulus
Glomerular Diseases
Clinicopathological manifestations of glomerular diseases:
Syndromes
Mixed nephritic and nephritic:
Henoch- Schőnlein prupura.
IgA nephropathy.
Membranoproliferative GN.
Nephrotic syndrome:
Pathogenesis of nephrotic syndrome:
Capillary damage --> escape of lipid in urine --> Lipiduria.
The liver is stimulated by hypo- albuminemia --> compensatory increase in lipoprotein production --> Hyperlipidemia
Decreased plasma volume --> decreased GFR --> Aldosterone stimulation --> salt and water retention which accentuate edema.
Damaged capillary wall lead to escape of protein (mainly albumin) in urine --> Albuminuria --> Hypo- albuminemia --> decrease osmotic pressure --> Edema.
Glomerular lesions in nephrotic syndrome:
Secondary
Definition: A clinico- pathological syndrome characterized by:
Hyperlipidemia and lipiduria.
Generalized edema
Massive proteinuria.
Nephritic syndrome:
Glomerular lesions in nephritic syndrome:
Systemic diseases
Primary glomerular diseases:
Leucocytic infiltration with focal epithelial and endothelial cells damage as well as BM damage --> Escape of RBCs leading to Hematuria and protein -->proteinuria.
Fluid retention (hypervolemia ) -->Hypertension.
Proliferation of glomerular cells, and swollen endothelial cells cause closure of epithelial slits --> decreased GFR (Oliguria).
Definition: Clinico-pathological syndrome of acute onset characterized by oliguria, Hematuria, Hypertension. Mild proteinuria and little edema.
GN associated with vasculitis.
Goodpasture's syndrome.
Acute diffuse proliferative GN.
Glomerulonephritis
Types of glomerulonephritis:
Hereditary glomerulonephritis:
Fabry`s disease.
Alport`ssyndrome
Secondary glomerulonephritis: Group of diseases in which the glomerular lesion represents a part of systemic disease.
Goodpasture syndrome
Prognosis: Fatal in most cases due to ARF & pulmonary Hge.
I/F: Linear deposition of IgG in GBM and Alveolar BM.
E/M; Epithelial & endothelial degeneration with fibrin deposition.
L/M: As RPGN with crescent formation.
Causes: Smoking, Wegner's granulomatosis, systemic vasculitis, drugs, viruses. The GBM is damaged by Ag- Ab reaction against fixed antigen (Goodpasture Ag)
Age: young adults.
Definition: Autoimmune disorder characterized by:
Usually RPGN or ADGN.
Pulmonary hemorrhage: usually precedes renal affection.
Henoch- schenolin purpura.
Lupus nephritis.
SLE
Lupus Nephritis
Histopathological classification:
Granular deposits of IgG, IgM, IgA, C3 and fibrin.
In type IV, the capillary loops show marked accumulation of deposits in the mesangium and subendothelial regions. The deposits in the latter location give the characteristic 'wire- loop' lesions.
Type III, is characterized by segmental necrosis and leukocytic infiltration.
In Type II, the glomeruli show diffuse mesangial deposits and hypercellularity
Five different patterns:
V- Membranous GN.
IV- Diffuse proliferative GN.
III- Focal proliferative GN.
II- Mesangioproliferative GN
I- Normal histology (rare)
Clinically: Nephritic or Nephritic.
Occurs in 50- 80% of patients with SLE. The onset of renal affection is usually about 2 years after the onset of the disease.
Diabetes mellitus (D.M.)
Primary glomerulonephritis: Group of diseases which primarily affect the glomeruli.
Chronic GN.
Size: Bilateral small contracted kidneys ( CRF.
Causes: End pool of many different glomerular lesions
Post- streptococcal (acute diffuse ) GN (1- 2%).
IgA nephropahy (30-50%).
Membrano- proliferative GN (50%)
Membranous GN (50%).
Focal glomerulosclerosis (50%).
RPGN (90%).
IgA nephropathy
The site of deposits depends on the type of the lesion.
Focal segmental glomerulosclerosis (FSGNS).
Microscopic picture: Glomerular deposition of hyaline eosinophilic glycoproteins in one of the following 3 patterns:
Nodular glomerulosclerosis (capsular drop): One or more noules in one or more lobules of the capillary tuft.
Diffuse glomerulosclerosis: Thick GBM, Thick arterioles, Mesangial cell and matrix proliferation.
Capillary and tubular BM.
Gross picture: slightly enlarged kidneys
Clinically: .
Hematuria and Hypertension. Chronic renal failure in 20% within two years and 50% of cases after 10 years.
Non- selective proteinutia, not responding to steroids)
I/F: Deposition of IgM and C3.
E/M:
increase mesangial matrix in sclerotic segment.
Detachment of epithelial cells.
Denuded GBM.
Diffuse effacement of epithelial foot processes.
Interstitial fibrosis
Tubular atrophy.
Glomeruli: Early, the glomeruli show focal segmental sclerosis. Later on, more sclerotic glomeruli.
Secondary: HIV, Heroin addiction and also associated with loss of renal mass, massive obesity, or congenital malformations
Primary (idiopathic): commonly seen in steroid-resistant children with nephrotic syndrome.
Memranoproliferative GN.
Clinically: About 50% of the cases end up with renal failure within 10 years. Type II. has a mote worse prognosis, being autoimmune in nature it recurs in transplantation.
I/F
Type II: C3 is found with no antibody. This reflects the alternative complement pathway.
Type I: Complement components and Igs.
E/M
Type II: Dence deposits located within the lamina densa, (Dense Deposit Disease)
Type I: Subendothelial electron dense deposits.
L/M: Glomeruli: Are hypercellular (due to proliferation of mesangial cells) and show lobular accentuation. Staining with periodic acid Schiff (PAS) reveals basement membrane double contour (Tram- track) appearance, due to splitting of the basement membrane by interposed mesangial cell processes.
Gross picture: Bilateral kidney enlargement.
Type II: Mostly autoimmune initiated by C3 nephritic factor in serum activating the alternative pathway.
Type I: Idiopathic, chronic immune complex reaction initiated by some antigens, including: SLE, malignancy, HBV and HCV.
Pathogenesis: Ag-Ab complexes & complement fixation-- >Hypocomplementemia.
Type II: Activation of complement by the alternative pathway.
Type I: Activation of complement by the classic pathway.
About 65% of cases present by Nephrotic syndrome. Others present with a combined nephritic and nephrotic syndrome.
Glomerular disease Characterized by thickening of GBM by immune deposits and proliferation of glomerular cells.
Membranous (MGN).
Renal insufficiency, 60 %.
Hypertention + hematuria, 30%.
Hematuria, 15%.
Non- selective proteinuria, not responding to steroids.
Fig 6.9:
I/F: Diffuse granular deposits of Immunoglobulin and complement.
E/M: Irregular, subepithelial deposits with loss of epithelial foot processes. Marked diffuse thickening of the capillary walls without increase in the number of cells --> prominent 'spikes' of silver- staining matrix projecting from the basement membrane lamina densa toward the Bowman's space.
L/M
Interstitial tissue is infiltrated by mononuclear cells.
Tubules reveal hyaline droplets
Glomeruli: Early lesions reveal normal glomeruli. Later on there is diffuse thickening of GBM.
Gross picture: Both kidneys are enlarged and pale.
Secondary: infection (HBV,HCV), Drugs, Malignancy, SLE, D.M and thyroiditis. It is initiated by circulating Ag- Ab complexes.
Idiopathic: Diffuse thickening of GBM by immune deposits. Antibodies develop against renal auto- antigen on the basal surface of visceral epithelial cells. The immune deposits are mainly subepithelial --> Activation of mesangial cells to liberate proteases and oxidants --> Injury of the capillary wall and leakage of protein.
The most common cause of nephrotic syndrome in adults.
Minimal change disease (Lipoid nephrosis).
May be associated with Hodgkin's disease and NSAID therapy.
Improve at puberty.
Recurrence is common with steroid dependence.
Massive and selective proteinuria (albuminuria) with rapid response to corticosteroids.
E/M: Normal basement membrane, no deposits, diffuse effacement of epithelial foot processes.
IF: No deposits.
L/M: Within normal (minimal change) except for the proximal convoluted tubules which show lipid laden cells (lipoid nephrosis) due to tubular reabsorption of lipo- proteins.
Gross picture: Kidneys are within normal.
Immune dysfunction (evidenced by absence of immune deposits). Release cytokines --> damage visceral epithelial cells proteinuria.
Predisposing factors:
Atopy
Immunization
Respiratory tract infection.
Characterized by:
Good prognosis
High response to corticosteroids
No immune complex deposits
Diffuse loss of foot processes
The most common cause of nephrotic syndrome in children.
Diabetes
Amyloidosis
Focal segmental GN.
Membranous GN.
Rapidly progressive GN.
RPGN =Rapidly Progressing (Crescentic) glomerular nephritis
Renal dialysis or transplantation is needed in nearly all cases.
Nephritic syndrome with more oliguria & azotemia.
E/M: Rupture within GBM ± subepithelial deposits
I/F: Deposits depends on the type.
L/M: Epithelial crescent in Bowman’s space formed of proliferating epithelial cells, Endothelial and Mesangial cells with fibrin strands. There is degenerative changes in renal tubules and interstitial inflammatory cellular infiltrate. Sclerosis follow later on.
Gross picture: Bilateral enlarged, pale white kidneys with sub- capsular petechial hemorrhage.
Type III: Pauci immune:
Examples: Wegener’s granulomatosis and PAN.
There is ANCA (Anti- Neutrophil Cytoplasmic Antibody) in serum
Lack of anti-GBM antibodies or immune complexes by E/M or IF.
Type II: Circulating immune complex: SLE, post infectious .
Type I: Linear deposits (anti- GBM Ab): Goodpasture’s syndrome.
Rarely follow acute GN.
Systemic diseases: SLE, Goodpasture syndrome, PAN, Henoch- Schönlein purpura, Wegener’s granulomatosis.
Definition: Clinico- pathologic glomerular disease rapidly progressing to renal failure and death and characterized by crescent of cellular proliferation in Bowman’s space.
Acute diffuse proliferative (post- streptococcal) GN.(glomerular nephritis )
Prognosis: It differs according to age of patient.
Adults: 60% recover, the rest passing to RPGN or chronic GN.
Children: 95% complete recovery, 1% RPGN, 1% chronic GN.
Lab. findings:
Urine
Casts: Hyaline, Blood, Epithelial, and Granular casts.
Hematuria
Albuminuria
Oliguria
Dark smoky urine.
Blood
Increased ESR and ASO titre.
Decreased complement level.
Hypoalbuminemia
Immunofluorescence microscope (I/F): Diffuse granular deposits of IgG, IgM and C3 in mesangium and in GBM.
Electron microscope (E/M): Subepithelial dense deposits "Humps".
Light microscope (L/M):
Interstitium: Edema and neutrophilic infiltration.
Tubules: Red cell casts.
Glomeruli: Enlarged and hypercellular due to proliferated resident cells and leucocytic infiltration. Cellular proliferation and fibrin deposits obliterate capillary lumens.
Cut section: Good differentiation between cortex and medulla.
Bilateral enlarged kidneys with tense capsule and sub- capsular petechial hemorrhage.
Formation of circulating Ag- Ab complexes trapped in glomeuli with complement activation --> glomerular injury.
Antibodies to streptococcal M protein cross react with renal tissue due antigenic similarity.
Occurs 1- 4 weeks after streptococcal pharyngitis.
Develop 2- 4 weeks after streptococcal infection by beta- hemolytic streptococci both throat and skin.
Usually affects children
Histopathlogical features of GN:
Additional alterations: Thrombosis, fibrin deposition
Hyalinosis and sclerosis of glomeruli.
Thickening of GBM: Deposits of immune complexes
Leukocytic infiltration: PNL’s, monocytes and lymphocytes.
Cellular proliferation: Endothelial, epithelial and mesangial.
The lesions may be:
Global: all the glomerulus affection.
Segmental: affects parts of some glomeruli.
Focal: affects only some glomeruli (less than 50% )of the glomeruli
Diffuse: affects all or more than 50% the glomeruli
Definition: Group of renal diseases in which the essential lesion is glomerular.
Pathogenesis of glomerular injury:
The glomerular injury is either:
Non–immunologic.
MECHANISMS:
Inherited glomerular disease: Alport's syndrome.
Drugse: Nonsteroidal anti- inflammatory drugs (NSAIDs).
Deposition disease: Amyloidosis.
Hemodynamic glomerular injury: Systemic hypertension.
Metabolic glomerular injury: Diabetic nephropathy.
Immunologic
MECHANISMS
Mediators of glomerular injury:
Antibody deposition:
T- cell immune reaction: Stimulation of macrophages and mesangial cells --> glomerular injury
Immune mediated injury leads to:
Secrete cytokines and arachidonic acid metabolites by resident cells (epithelial, endothelial and mesangial cells).
Release biologically active molecules by macrophages.
Platelets aggregation --> prostaglandins and growth factors.
Immune complexs with activation of C5a --> recruit of neutrophils --> release of proteases, oxygen free radicals and arachidonic acid metabolites --> glomerular injury.
Activation of C5b- 9 -- > detachment of epithelial cells & release of chemical mediators.
It may be
Cell- mediated.
T- cell immune reaction: Stimulation of macrophages and mesangial cells --> glomerular injury.
T- cell- mediated glomerular injury:
Sensitized T- cell can produce glomerular injury through stimulation of macrophages and mesangial cells to produce mediators that leads to glomerular injury.
Anti- body mediated
Localization of immune complexes in glomerular injury.
Factors affecting localization of immune complexes:
Charge of the immune complex:
Neutral complexes are deposited in mesangium.
Negative do not cross GBM, deposited subendothelial.
Positive charged cross GBM, deposited subepithelial
Size of the immune complex:
Small- sized complexes: deposited in the glomerulus.
Very large complexes: phagocytosed.
The localization of immune complexes may be
EN, endothelium; EP, epithelium; LD, lamina densa; LRE, lamina rara externa; LRI, lamina rara interna; MC, mesangial cell; MM, mesangial matrix. اختصارات
Basement membrane, as in membranous GN.
Mesangial deposits, as in IgA nephropathy
Subendothelial deposits, as in lupus nephritis and membranoproliferative GN
Epimembranous deposits, as in Heymann GN.
Subepithelial humps, as in acute diffuse GN glomerular nephritis
This includes
Other mechanisms of glomerular injury:
Damage of epithelial cells and effacement of foot processes --> leakage of protein and proteinuria.
Epithelial cell injury caused by:
Antibodies to visceral epithelial cells
Circulating immune complexes:
The Ag- Ab complexes bind to the complement --> glomerular injury, PNL's polymorphneucliec lymphocytes infiltrate --> dense, granular subendothelial, subepithelial and mesangial deposits.
The Ag. May be:
Endogenous: SLE systemic lupus erythromatus
Exogenous: Bacterial or viral (HBV, HCV infection) or tumor antigen.
The circulating Ag- Ab immune complexes are trapped in glomeruli (type III hypersensitivity reaction).
In situ immune complex:
Antibodies directed against planted non- glomerular planted antigen:
Endogenous Ags: DNA, Igs, Immune complexes, presented by granular heterogeneous deposits.
Exogenous Ags antigens: Drugs & infectious agents e.g viral, bacterial or parasitic.
Hyemann nephritis: Antibodies react with antigen of epithelial cells leading to diffuse sub- epithelial granular deposits e.g. Membranous GN.
Anti- glomerular B.M. Basement membrane nephritis: Antibodies react with glomerular basement membrane Ag along its entire length, represented by linear pattern immune complex deposits e.g. Good- Pasture syndrome.
Antibodies react with glomerular antigens.
The deposited Ag- Ab complexes in the glomeruli is the major mechanism of glomerular injury.
In most types of GN.
Function
Glomerular filtration rate” (GFR): (125 ml/min). The rest of the plasma (700-125= 575 ml) return back to the efferent arterioles and runs, through the Peritubular capillaries, side by side with the glomerular filtrate in the kidney tubules.
Capillaries in the glomerulus is characterized by:
Forming special membrane, glomerular membrane (through which filtration occur).
Dynamics of glomerular filtration:
Net filtration pressure = 60 – (18 + 32) = 10 mm Hg.
Opposing forces for the filtration, are:
Oncotic pressure of plasma proteins = 32 mm Hg (here it is high because high concentration of plasma proteins).
Hydrostatic pressure in Bowman’s capsule = 18 mm Hg.
Driving force for GFR is the hydrostatic pressure in glomerular capillaries = 60 mm Hg.
Passage of molecules through glomerular membrane:
Negative Charge of complex proteoglycan lining the pores of glomerular membrane repel strongly with the -ve charge of the albumin so only 0.5% is filtered.
Charge and diameters of the molecules are the main factors
Substances with diameters greater than 8nm almost totally excluded.
Neutral substances up to 4 nm in diameter freely pass.
The glomerular membrane has 4 layers:
Filtration slit diaphragm: basement membrane of the podocytes, which is the second layer of the Bowman’s capsule.
Epithelial cells of Bowman’s capsules (podocytes): The most outer layer of interrupted epithelial cells arranged in a finger like projections (pseudopodia) forming filtration slit pores through it filtrate passes.
Basement membrane (basal lamina): formed of loose collagen bundles and proteoglycan filament with wide large spaces in between.
Endothelial walls: which has thousands of small holes (fenestrae, 70-99 nm in diameter).
Very high permeability (100-500 times as normal capillaries).
High pressure in comparison to other capillaries in body (60 mmHg).
Filtration in glomeruli.
Composition of the Glomerular Filtrate GF or Primary Urine:
However, it differs from the plasma in:
Non-protein anions (Cl- & HCO3-) are 5% > plasma, while cations (Na+ & K+) are 5% less as a result of Donnan equilibrium.
Contain small amounts of proteins (0.03 gm/dl) mainly albumin.
GF has the same properties as the plasma as regarding Its pH (7.4), specific gravity (1010 ) & osmolality (300 mosmol/litre).
GF composed mainly of water & freely filterable substances at equal concentrations with plasma (e.g. glucose, urea, electrolytes, amino acids,.. etc).
GLOMERULAR FILTRATION RATE (GFR)
Factors affecting GFR
Sympathetic stimulation:
Marked sympathetic stimulation as in severe exercise or intense emotional stress diminishes GFR by constricting the renal artery.
Systemic blood pressure:
Marked elevation above 200 mmHg causes an increase in GFR and urine formation phenomena called “pressure diuresis”.
Marked decrease of blood pressure below 70 mmHg as in severe haemorrhage there is marked decrease in GFR & may even stops → acute renal failure.
GFR remains more or less constant between blood pressure 70 & 180 mmHg due to auto-regulation of renal blood flow.
Permeability of glomerular membrane
It is affected by:
State of intra-glomerular mesangial cells (contractile cells)
Mesangial relaxation decrease GFR.
Mesangial contractions decrease effective filtration area with subsequent decrease in GFR.
Total surface area of filtration (which is determined by total number of healthy nephrons)
Oncotic pressure of plasma proteins = 32 mmHg.
Oncotic pressure of plasma proteins is here relatively high (32 instead of 28 mm Hg) because the filtered fluid is protein free filtrate which increases the concentration of plasma proteins.
Diminish formation plasma proteins (as in liver diseases or marked loss in kidney disease) increases GFR.
Antagonising force for filtration.
Hydrostatic pressure in Bowman’s capsule = 18 mmHg.
It is the antagonising force for filtration.
If maintained high leads to back pressure degeneration (hydronephrosis).
Increase Hydrostatic pressure in Bowman’s capsule as by stone any obstruction in the urinary tract decreases GFR
Hydrostatic pressure of the glomerular capillaries = 60mm Hg.
This pressure is affected by diameter of afferent or efferent arterioles as:
Therefore, the relation between the diameters of both afferent and efferent arterioles greatly determines the GFR.
Diminish renal blood flow (constriction of afferent arterioles and severe narrowing in efferent arterioles) will diminish the glomerular capillary pressure that decreases GFR.
Mild constriction of efferent arteriole alone could increase in the glomerular hydrostatic pressure with subsequent increase in the GFR.
An increase blood flow to the kidney (dilatation of afferent arterioles and mild constriction of efferent arterioles) will increase the glomerular capillary pressure that increases GFR.
GFR is directly proportional to glomerular capillary pressure i.e. ↑ glomerular capillary pressure → increase filtration force →increase GFR & vice versa.
Filtration fraction: It is the percentage of GFR as regard the renal plasma flow. = (GFR/Renal plasma flow) x 100 = (125/700) x 100 = about 20 %
The process of filtration is passive.
It is about 10% less in females than males.
It equals 125ml/min in normal 70 kg young adult.
Definition: It is the amount of protein free plasma which is filtered in both kidneys per minute across the glomerular membrane.
Average capillary area of filtration in one glomerulus = 0.4 mm2 and the total surface are of glomerular membrane in two kidneys = 0.8 m2.
It is an efficient filter with large surface area. It represents the blind cub-shaped end of the nephron which contains the glomerular tuft of capillaries. The blood is separated from bowman’s space by glomerular basement membrane (GBM).
Glomerular basement membrane
The GBM is highly permeable to water and small solutes. It has selective permeability to different protein molecules depending on:
The charge
The cationic (+ve charged) molecules are more permeable as the basement membrane is anionic (ve charged)
The size of the molecules
More permeable to smaller molecules.
The glomerular basement membrane is composed of 3 layers:
Epithelium rested upon basement membrane by foot processes, separated by gaps 30- 60 nm in diameter (filtration slits).
Basement membrane consists of a central lamina densa, lamina rara interna and lamina rara externa. It has strong anionic (- ve) charge.
Fenestrated capillary endothelium containing pores measuring (70- 100 nm in diameter).
NB. The afferent arteriole has a thick wall, thick media, and thick elastic lamina with juxtaglomerular cells in its media. The efferent arteriole has a thin wall, thin media, and thin elastic lamina.
The endothelium has well developed basal lamina.
Glomerular capillary wall is lined by fenestrated endothelium with pores of 70-90 nm in diameter.
Glomerulus is a Tuft (group) of capillaries about 50 in number that emerge from an “afferent arteriole” and then drained by an “efferent arteriole”.
Afferent arteriole diameter is about 3 times that of efferent arterioles.
The afferent arteriole divides into several capillary loops (Glomerulus) where blood enters under pressure and recollects forming the efferent arteriole (vascular pole of the nephron).
It is the vascular portion of the renal corpuscle.
Bowman's capsule.
Bowman’s capsule is the dilated blind end of the renal tubule which invaginates the glomerulus.
It is a double walled cup-shaped top of the nephron, formed of a doublewalled epithelial layer that encloses the glomerulus (tuft of capillaries).
The internal visceral layer is in contact with glomerular capillary and is formed by modified simple squamous epithelium; “Podocytes”.
Podocytes
EM
It is formed of three layers:
Two electron-lucent layers called lamina lucida or lamina rara (lamina rara interna adjacent to the endothelium and lamina rara externa adjacent to the podocytes)
Central electron- dense layer called lamina densa
The basal lamina of both podocyte and glomerular capillary endothelium fuse together and form a thick basal lamina.
The adjacent pedicles leave spaces in between called filtration slits (20- 40nm) which is covered by slit diaphragm.
The feet tightly attached to the basement membrane of fenestrated blood capillaries.
Minor (secondary) processes are small processes extend from the major process to grasp the glomerular capillaries by little feet or pedicles (Fig 1.11).
Major (primary) processes are large cytoplasmic processes extending from the cell body and contain microfilaments and microtubules.
The cell bodies are separated from the underlying capillary by a space of 1-3 µm called subpodocytic space.
The cytoplasm contains small Golgi, RER, abundant free ribosomes, intermediate filaments, and microtubules.
LM
Their cytoplasmic processes are of two types:
Their basement membranes are well developed and can be demonstrated by PAS as a positive line.
Secondary (minor or feet) processes or pedicles: each primary process gives rise to many processes which envelop the fused basement membranes of both the capillary endothelium and podocytes.
Primary (major) processes: arise directly from the cell body and is directed towards the capillary loop.
They are large flat modified stellate simple squamous epithelial cells with large oval nuclei.
The external parietal layer is composed of simple squamous epithelium which is continuous with the cuboidal epithelium of the proximal convoluted tubules.
The renal corpuscle has two poles:
Urinary pole: where the proximal convoluted tubule begins.
Vascular pole: where the afferent and efferent arterioles enter and exit.
Its diameter is about 150-200um.
NEPHRON DYNAMICS and RENAL BLOOD FLOW
Renal handling of
FLUID, ELECTROLYTES AND ACID BASE BALANCE REGULATION
Renal Handling of Hydrogen & Bicarbonate
RENAL HANDLING OF WATER
Renal handling of phosphate
Renal Handling of Calcium
Renal handling of chloride
Renal handling of potassium:
Renal Handling of Na+
PROTEINS & AMINO ACIDS
Renal Handling of amino acids: is similar to glucose reabsorption i.e. it occurs in PCT, in an active process that depends on Na+ transport & shows tubular maximum due to carrier saturation.
In some diseases e.g. nephritis → Decrease sialoproteins (which has -ve charge in glomerular wall) → Increase loss of albumin in urine (albuminurea).
Normally, about 1% of albumin is filtered in the kidney but it is completely reabsorbed by pinocytosis.
UREA & URIC ACID (UA)
Renal handling:
Urea balance: (its production = its excretion)
Filtered UA may be
Excreted in urine (20%) So the net reabsorption in PCT = 80%.
Secreted (10%) in the PCT
Reabsorbed (90%) in the PCT
Uric acid is produced as a product of purine metabolism.
Its excretion depends on
GFR glomerular filtration rate : Decrease GFR Decrease urea excretion increase plasma urea.
NB: Remember that, Urea Clearance less than inulin clearance as a part of urea is reabsorbed (= 0.60 x 125 = 75ml/min).
Urine flow rate:
Diluted urine & high flow rate 40% of urea reabsorption.
Concentrated urine & low flow 80% of urea reabsorption.
H2O reabsorption in collecting ducts: ↑↑ H2O reabsorption → ↑ concentration of urea inside renal tubules → passive diffusion of urea to medulla & ↓ its excretion.
Its production depends on protein metabolism.
Small amounts of urea is reabsorbed in PCT.
40 to 60% of the filtered urea is excreted & this amount depends on Urea concentration in plasma & GFR.
Blood urea nitrogen BUN = ½ blood urea = 10-20 mg/dl.
Normal blood urea level equals 20 - 40 mg/dl.
Urea is formed in the liver as an end product of nitrogen metabolism.
GLUCOSE
Handling of glucose in different parts of renal tubules
Renal threshold of glucose:
Definition: it is the blood level of glucose below it glucose is never appears in urine (completely reabsorbed & its plasma clearance = zero).
This level = 180mg/dl in normal adult.
Above 180 mg/dl glucose starts to appear in the urine & the capacity of the kidney to reabsorb glucose is also increased as a result of ↑ activity of the carries system.
Glucosuria
It is appearance of glucose in urine. The most common causes are:
Endocrinal disorders as Cushing syndrome
deficiency in carrier system of renal tubules.
Diabetes mellitus
The more hyperglycaemia → the more activation of carries system & more increase in capacity of kidney to reabsorb glucose accompanied by more and more glucosuria.
At a certain glucose level → carrier in the kidney becomes fully saturated → cannot transport any more glucose → any excess glucose is excreted totally in the urine (this level is called tubular maximum transport of glucose).
Splay
Splay can explain the difference between renal threshold value & TmG value
Nephrons have different maximum capacities for glucose reabsorption with different TmG values (not all TmG values = 375 mg/min).
Tubular maximum transport of glucose TmG:
Value: = 375 mg/min in males & 300 mg/min in females which is corresponding to plasma level = 300 mg/dl.
TmG depends on:
Carrier system:
It is Inhibited by the plant glucoside (competes with glucose at the carrier ) & Oubain (blocks Na+ K+ ATPase).
It Carry other monosaccharide as galactose, xylose & fructose → compete together for the carrier.
It binds “d” isomer of glucose more than “L” isomer.
Reabsorptive power of the nephrons: the maximum reabsorptive power of nephrons is different, so TmG level is reached gradually.
Definition: the tubular load level of glucose at which any excess filtered glucose is excreted in the urine.
Glucose is typical substance that is reabsorbed by secondary active transport (co-transport mechanism being coupled with Na+ reabsorption) as follow: Occurs in 1st half of PCT
Insulin here is not essential for glucose transport in PCT cells.
Energy needed for this transport is derived from energy released by Na+ K+ ATPase at basolateral border of cells.
Increased glucose concentration inside cells → passive transport of glucose across the basolateral border to interstitium by facilitated diffusion by glucose transporter 2 (GLUT2).
Common carrier [sodium glucose transporter 2] (SGLT2) binds both Na+ & glucose at the luminal brush border (where Na+ diffuses from lumen to inside the cell along electro chemical gradient) → glucose transported into the cell against concentration gradient.
It is nearly completely reabsorbed by the PCT of the kidney and only negligible milligrams may be found in the urine over 24 hours.
Factors controlling RBF renal blood flow
Auto-regulation of the renal blood flow:
Mechanism may be:
Tubulo-glomerular feedback: Signals from renal tubule feedback to affect glomerular filtration. Increase ABP increase GFR increase rate of flow in DCT signal from macula densa cells (adenosine) adenosine A1 receptors on macula densa cells increase release of Ca2+ to vascular smooth muscles in afferent arteriole VC of afferent art. decrease GFR and RBF to normal. decrease ABP decrease GFR decrease rate of flow through the ascending limb of loop and first a part of DCT decrease Na+ and K+ concentration signal from the macula densa which produces:
Both increase ABP and GFR to normal.
Secreting rennin increase formation of angiotensin II VC of efferent arterioles by.
Releasing prostaglandin PGI2 VD of afferent arterioles.
Intra-renal tissue pressure theory: tight capsule that surround the kidney, prevent marked change in RBF i.e. increase blood flow increase Intrarenal pressure diminish excess blood flow (and vice versa).
Myogenic: increased ABP stretch of arterial wall depolarization in its smooth muscles constriction of the arterioles diminish RBF (and vice versa).
increase ABP to 210 mmHg increase urine output 7 – 8 times which is called pressure diuresis.
decrease ABP to 50 mmHg stop urine output.
Change of blood pressure from 70 to 180 mmHg little change in RBF not more than 10% or Glomerular filtration rate (GFR).
Kidneys have an auto regulatory mechanism of RBF i.e.
Hormonal and toxic factors:
Some bacterial toxins and other pyrogens VD of renal vessels.
Endothelium derived relaxing factor (EDRF or NO) and PGE2, PGI2 renal VD.
Acetyl choline and dopamine renal VD.
Endothelins, ADH and serotonin decrease RBF (renal VC). c) Prostaglandins increase blood flow to cortex but diminish it to the medulla.
Angiotensin II and Norepinephrine decrease RBF (VC of interlobular arteries and efferent arterioles).
Hemodynamic factors:
High-protein diet increase glomerular capillary pressure increase RBF.
Sudden standing from recumbent position decrease RBF (by 20%).
During pregnancy increase renal blood flow (by 50%).
Drop in blood pressure as in haemorrhage markedly reduces RBF to the degree that causes papillary necrosis and acute renal failure.
Nervous factors:
Severe muscular exercise diminishes RBF reduces GFR and urine formation.
Strong stimulation of the sympathetic nerves diminishes greatly RBF (VC of renal artery).
Renal plasma flow: (700 ml/min)
O2 consumption by the kidney tissue is low.
About 180 Litres of plasma are cleaned/day (The whole plasma is cleared 60 times/day).
Renal blood flow (RBF) is the volume of blood that flows through kidney each minute = 1200 -1250 ml/min (it receive > 22% of the cardiac output)
It is the functional unit of the kidney arises in the cortex and descends into the medulla then return back to the cortex.
The kidney is a large compound tubular gland. It consists of structural units called uriniferous tubules The nephrons and the collecting tubules perform 2 different functions and are of different embryological origin.
STROMA
Capsule
The kidney is covered with a connective tissue capsule consisting mainly of dense, irregular collagen fibers with elastic fibers and smooth muscle cells. These cells help resisting volume and pressure variations of the kidney. The capsule is surrounded by perirenal fat that is protective to the kidney.
Pathological Disease of the Kidney and Urinary System.
Mind Map
ALBUMIURIA
Definition: Presence of albumin in urine.
Post renal: urinary tract infections.
Renal: Nephrotic and nephritic syndromes.
Prerenal: congestive heart failure.
HEMATURIA
General
Drugs as salicylates.
Hemorrhagic blood diseases.
Local
Prostate: Prostatitis.
Urinary bladder: Cystitis, stones, tumors.
Ureters: Stones, bilharzisis, tumors.
Kidney: Stones, Pyelonephritis, Glomerulonephritis, Renal infarction and Renal cell carcinoma.
Definition: Blood in urine above normal range (3-5/HPF).
CAUSES OF ENLARGED KIDNEY:
Chronic venous congestion.
Fatty change.
Cloudy swelling.
Early amyloidosis.
Acute diffuse GN, RPGN
Hydronephrosis, Pyonephrosis.
Polycystic kidney.
CAUSES OF CONTRACTED KIDNEY:
Radiation nephritis.
Benign nephrosclerosis.
Athrosclerosis
Late amyloidosis.
Chronic pyelonephritis.
Chronic glomerulonephritis.
Senile kiney.
Hypoplastic kidney.
Cystitis
Follicular cystitis: lymphoid aggregates with well-formed germinal centers in the lamina propria.
Non- specific cystitis: Chronic non specific cystitis either on top of acute inflammation or de novo. The bladder wall is thick with fibrosis and infiltration by mononuclear cells. The lining mucosa is granular and show epithelial changes as ulcerations, squamous metaplasia and dysplasia.
Specific cystitis: Bilharzial, tuberculous and fungal cystitis.
Chronic interstitial cystitis: Chronic inflammation associated with mucosal ulceration.
Polypoid cystitis: Chronic inflammation associated with polypoid mucosal projections.
Emphysematous cystitis: Infection by gas producing bacteria
Gangrenous cystitis: Infective gangrene, especially in debilitating diseases.
Eosinophilic cystitis: Allergic inflammatory reaction with abundant eosinophils
Suppurative cystitis: Acute suppurative inflammation on top of bacterial infection, reaching the bladder as ascending infection from urethra, descending from the kidney or hematogenous.
Definition: Inflammation of urinary bladder.
Urinary Tract Obstruction
Differences between Hydronephrosis and Pyonephrosis
Renal Calculi (Stones, Urolithiasis)
Types of renal stones:
Injury of bladder wall --> Hematuria.
Large sized stone -->Obstruction.
Infections (cystitis, pyonephrosis, pyelonephritis)
Calculus anuria.
Hydronephrosis, hydroureter.
Cystine stone Migration --> Renal colic.
Uric acid or Urate stone 5% Single, hard, yellowish-brown and smooth Caused by Hyperuricosuria (as in hyperuricemia with gout & leukemia) Formed in acidic urine Radiolucent
Calcium oxalate stone: 80%, Multiple, small, hard, dark brown and spiky Caused by Hypercalciuria , Hyperoxaluria, vitamin C abuse, hypocitraturia , malabsorption (Crohn disease). Formed in acidic urine Radio-opaque
Causes: Triad of disturbed urine composition, stasis & UT infection.
Urinary tract infection:
Produce a nidus for stone formation.
Change urine pH:
Pyogenic infection --> Alkaline urine phosphate stone.
E. coli infection --> Acidic urine, precipitate oxalates & urates.
Urine stasis (obstruction): Urine stasis predisposes to infection, helps precipitation of crystalloids and provides a nidus for stone formation.
Disturbed urine composition:
Super-saturated urine by crystalloids, e.g:
Cystine: Genetic defect in cystine metabolism.
Urates & Uric acid: Gout or leukemia.
Oxalates: Increased dietary intake, primary hyper-oxaluria.
Calcium: Idiopathic hypercalcemia, hyper-parathyroidism, Hypervitaminosis-D.
Concentrated urine.
Renal stone formed due to imbalance between crystalloids and solvents leading to precipitation of crystalloids in urine.
Glomeruli and tubules are compressed and atrophic
The epithelial lining is shredded and necrotic.
Enlarged kidney, bosselated with dilated-pelvicalyceal system filled by pus.
Either arises w ith chronic pyelonephritis or secondary infected hydronephrosis.
Dilated pelvi-calyceal filled by pus
Later glomerular and tubular atrophy with obstruction of blood vessels
Enlarged kidney, bosselated outer sur face with atrophic intervening renal tissue
The cavities filled by urine and have smooth lining.
Cause
UT obstruction
Nature
Dilated pelvicalyceal system filled by urine
Pyonephrosis
Gross picture
The intervening renal tissue is compressed and atrophic.
The pelvi-calyceal system is dilated and filled by pus. The epithelial lining is shredded and necrotic.
Secondary: Infection on top of hydronephrosis.
Primary: Chronic obstructive pyelonephritis.
Definition: Renal disease characterized by dilated pelvi-calyceal system, filled with pus causing pressure atrophy and fibrosis of renal parenchyma.
Hydronephrosis
Clinical course:
Urinary bladder wall trabeculation and diverticulosis in cases of Bladder neck or uretheral obstruction
Bilateral hydronephrosis: ended by CRF.
Hypertension (renal ischemia).
Pyonephrosis and pyelonephiritis: Hematuria &.pyuria.
Urine stasis: infection and stone formation.
Enlarged kidney: dull aching pain and heaviness at renal angle.
Interstitial tissue: Fibrosis, with obliterated blood vessels.
Tubules: Early dilated, later atrophied and fibrotic.
Glomeruli: Early intact but later atrophied.
Gross picture:
Dilated pelvi- calyceal system with smooth lining. The intervening renal tissue is atrophic.
Enlarged kidney with bosselated outer surface.
Effects: Dilated pelvi-calyceal system causing pressure atrophy of intervening parenchyma leading to progressive renal atrophy.
According to site of dilated pelvis: Intra- renal or extra- renal
According to site of obstruction: Unilateral or bilateral.
Causes: Obstruction at any level of urinary tract.
Strictures or stenosis of the urethera, ureter or bladder outlet.
Nodular prostatic hyperolasia.
Neurogenic bladder.
Calculi
Abdominal tumors.
Congenital abnormalities.
Definition: Abnormal dilation of the renal pelvis and the calyces of one or both kidneys, caused by an obstruction of urine flow causing kidney atrophy.
Urethera: Stricture, stone, tumor.
Prostate: Benign prostatic hyperplasia, tumor, prostatitis
Urinary bladder: Bladder neck fibrosis, stone, tumor, neurogenic bladder.
Ureter: Stricture, stone, tumor, blood clots, sloughed papillae.
Renal pelvis: Stone, tumor, aberrant renal artery, kinked pelvis or ureter, uretero- pelvic stricture.
MACROSCOPIC STRUCTURE
When the kidney is split longitudinally, it presents the kidney proper and the renal sinus.
Renal Sinus
The renal pelvis within the sinus is divided into two or three large branches, called major calyces,
which further divides to form 5–11 short branches called minor calyces (Fig. 1.8). Each minor calyx expands as it approaches the wall of renal sinus, and its expanded end is indented and moulded around the renal papilla.
It is a cavity of considerable size present within the kidney. It takes up a large part of the interior of the kidney and opens at the medial border of the kidney as hilus (Fig. 1.7). It contains:
Fat
Renal vessels, lymphatics, and nerves.
Greater part of the renal pelvis, major and minor calyces
Kidney Proper
The naked eye examination of the kidney proper presents an outer cortex and an inner medulla (Fig. 1.7). The cortex is located just below the renal capsule and extends between the renal pyramids as renal columns (columns of Bertini).
The medulla is composed of 5–11 dark conical masses called renal pyramids (pyramids of Malpighi). The apices of renal pyramids form nipple-like projections—the renal papillae which invaginate the minor calyces. N.B. A renal pyramid along with its covering cortical tissue forms a lobe of the kidney.
The cortex appears pale yellow with granular texture.
CLINICAL CORRELATION
Transplantation of kidney
It is done in chronic renal failure in selected cases. The donor kidney is placed retroperitoneally in the iliac fossa with hilum parallel to the external iliac vessels. The renal artery is anastomosed end to end to the internal iliac artery and renal vein is anastomosed end to side to the external iliac vein. The ureter is implanted into the urinary bladder (ureterocystostomy).
Floating kidney (hypermobility of the kidney)
However, each kidney moves up and down with respiration. If the amount of perinephric fat is reduced, the mobility of the kidney becomes excessive (floating kidney) A floating kidney can move up and down but not from the side to side within the renal fascia
The kidney is kept in position by the perirenal fat and renal fascia.
Renal pain:
The renal pain occur either due to stretching of the renal capsule or due to spasm of the smooth muscle in the renal pelvis.
The pain is commonly referred along the subcostal nerve to the flank and anterior abdominal wall and along the ilioinguinal nerve (L1) into the groin.
The afferent fibres pass successively through the renal plexus, lowest splanchnic nerve, sympathetic trunk, and enter the T12 spinal segment
The nature of pain varies from dull ache to severe spasmodic pain.
The renal pain is felt in the loin and often radiates downward and forward into the groin.
Renal failure
Chronic Renal Failure (CRF)
Stages of chronic renal failure
Consequences (MAD HUNGER):
Uremia: Azotemia accompanied with multi-organ affection.
Azotemia: Increased BUN & creatinine due to decreased GFR.
Renal osteodystrophy
Growth retardation and developmental delay
Erythropoietin failure (anemia)
Na+/H2O retention (HF, pulmonary edema, hypertension)
Uremia—clinical syndrome marked by:
Platelet dysfunction
Encephalopathy
Asterixis
Pericarditis
Nausea and anorexia
High potassium
Dyslipidemia (especially triglycerides)
Metabolic Acidosis
It passes through 4 stages:
End-stage renal disea se:
GFR<5%.
Renal failure:
GIT, neurological & cardiovascular complications.
Azotemia
Lack of volume regulation.
GFR< 20%.
Renal insufficiency:- GFR 20-50%. - Azotemia. - Anemia and hypertension. - Polyuria.
Diminished renal reserve: - GFR 50%. - Normal urea and creatinine. - Asymptomatic.
Definition: Prolonged deterioration of renal function with signs and symptoms of uremia.
Acute Renal Faliure
Complications:
Hyperkalemia
Hypertensive crisis.
Acute pulmonary edema.
Clinically
Hematuria, petechiae, ecchymosis.
Cold, clammy skin.
GIT symptoms.
Seizures and coma.
Lethargy and Confusion.
Tachycardia and hypotension
Oliguria or anuria.
Post-renal
Infections
Obstructions
Crush injuries.
Irradiation
Drugs
Acute GN.
Pre-renal:
Trauma, sepsis, tumors.
Arterial embolism, thrombosis, DIC, Vasculitis.
Hypovolemic shock: burns, dehydration, hemorrhage, diuretics.
Cardiogenic shock: MI, Heart failure.
Definition: Sudden interruption of renal function with severe oliguria or anuria, azotemia and uremia.
Neurovascularity
NERVE SUPPLY
Each kidney is supplied by the renal plexus of nerves which reach the kidney along the renal artery. The renal plexus consists of both
parasympathetic fibres
parasympathetic fibres are derived from both vagus nerves.
sympathetic fibers
The sympathetic fibres are derived from T10–L1 spinal segments,
Renal Vascular Diseases
Renal Cortical Necrosis:
Clinical effects: Oliguria, Anuria, ARF.
Morphology: Coagulative cortical necrosis.
Pathogenesis: Thrombosis of small arteries and arterioles
Infections: Pneumonia, diphtheria, scarlet fever.
Toxemia of pregnancy.
Malignant Nephrosclerosis:
Microscopic picture
Hyperplasic arteriolosclerosis: see general pathology.
Fibrinoid necrosis --> Necrotizing arteriolitis
Gross picture: The kidneys are normal size or slightly shrunken. The outer surface shows petechial hemorrhage (flea-bitten appearance)
Pathogenesis: Fibrinoid necrosis: Increased permeability to fibrinogen with endothelial cell injury and platelet deposition --> thrombosis and intimal hyperplasia --> narrowing of vascular lumina --> stimulation of the renin-angiotensin system --> more hypertension.
Vasculitis
Malignant hypertension
Benign Nephrosclerosis:
Microscopic picture:
Interstitial fibrosis with scanty lymphocytic infiltrate.
Glomerulosclerosis and hyalinosis.
Tubules undergo atrophic change.
Hyaline arteriolosclerosis: see general pathology.
Gross picture: The kidneys are uniformly atrophic with fine granular outer surface.
The term refers to renal changes in benign hypertension
Arteriolosclerotic Kidney:
Renal cortical necrosis.
Vasculitis: Polyarteritis nodosa.
Malignant nephrosclerosis.
Benign nephrosclerosis
Atherosclerotic kidney: Atheroma of the renal artery leads to renal infarction (general pathology), ischemic atrophy & fibrosis.
LYMPHATIC DRAINAGE
The lymphatics from the kidney drain into the para-aortic lymph nodes at the level of origin of the renal arteries (L2).
VENOUS DRAINAGE
The venous blood from the kidneys is drained by the renal veins (right and left). The left renal vein passes in front of the aorta immediately below the origin of the inferior mesenteric artery (Fig. 1.9)
ARTERIAL SUPPLY
The right renal artery passes to the right behind the inferior vena cava and right renal vein, while the left renal artery passes to the left behind the left renal vein
The kidneys are supplied by the renal arteries. Usually there is one renal artery for each kidney (arising directly from the abdominal aorta at the level of intervertebral disc between L1 and L2) (Fig. 1.9), but in about 30% individuals, accessory renal arteries are also found. They commonly arise from the aorta and enter the kidney at the hilus or at one of its poles, usually the lower pole.
CAPSULES (COVERINGS) OF KIDNEY From within outwards,
The kidney is surrounded by four capsules/coverings as follows (Fig. 1.5&1.6):
Pararenal (paranephric) fat.
It is a layer of fat lying outside the renal fascia. It consists of considerable quantity of fat being more abundant posteriorly and toward the lower pole of the kidney. It fills the paravertebral gutter and forms a cushion for the kidney.
Renal fascia (false capsule).
Extensions
At the medial border of the kidney, the two layers are attached by a connective tissue septum being pierced by the renal vessels. Because of this attachment (septum), perirenal effusion of the fluid does not usually extend across into the opposite perirenal space.
Laterally, the two layers unite firmly and become continuous with the fascia transversalis.
Inferiorly, the two layers remain separate and enclose the ureter.
Superiorly, the two layers first enclose the suprarenal gland and then fuse with each other and become continuous with the diaphragmatic fascia.
It is a fibroareolar sheath, which surrounds the kidney and perirenal fat. It consists of the following two layers:
A well-defined posterior layer (fascia of Zuckerkandl).
An ill-defined anterior layer (fascia of Toldt)
Perirenal (perinephric) fat.
In chronic debilitating diseases, the depletion of perinephric fat can cause downward displacement of the kidney, which may lead to the kinking of the ureter.
This fatty capsule is thickest at the borders of kidney and is prolonged through hilum into the renal sinus.
It fills the space inside the loosely fitting sheath of the renal fascia enclosing the kidney and suprarenal gland
It is a layer of adipose tissue, surrounding the fibrous capsule of the kidney.
Fibrous capsule (true capsule).
It is a thin membrane which closely invests the kidney. It is formed by the condensation of fibrous connective tissue in the peripheral part of the organ. It is readily stripped off from the surface of the normal kidney.
FACTORS CONTRIBUTING TO STABILITY OF KIDNEY:
Positive intraabdominal pressure causing apposition of neighbouring viscera to kidney.
Vascular pedicles (renal vessels connecting kidney to major vessels (aorta & ivc).
Fatty and fascial capsules coverings.
Position of kidney in depth of paravertebral gutter.
EXTERNAL FEATURES:
Each kidney presents the following external features (Fig. 1.3):
A hilum.
The medial border of the kidney presents a deep vertical slit called hilum. It transmits, from before backward, the following structures:
In addition to the above structures, the hilum also transmits lymphatics and nerves (sympathetic and mainly vasomotor).
Subsidiary branch of renal artery (Fig. 1.4)
Renal pelvis
Renal artery
Renal vein
Two borders (medial and lateral).
The lateral border of each kidney is convex.
The medial border of each kidney is concave in the middle. It presents a vertical fissure in its middle part called hilum.
Two surfaces (anterior and posterior).
The posterior surface is flat and faces posteromedially.
The anterior surface is convex and faces anterolaterally.
Two poles (superior and inferior).
The inferior (lower) pole is thin and pointed and lies 2.5 cm above the iliac crest.
The superior (upper) pole is thick and round and lies nearer to the median plane than the inferior pole. It is related to the suprarenal gland.
IDENTIFICATION OF SIDE IN KIDNEY
To identify the side of organ, you should know which part is superiorinferior, anterior-posterior and medial-lateral. After knowing this you can identify the side easily.
With these, you can place the kidney accordingly, to identify side.
Anterior-posterior: The orders of structures from anterior to posterior are vein, artery and ureter. Vein and arteries might be difficult to differentiate. Just know that ureter and pelvis is posterior.
Medial-lateral: this is easy. Hilum is medial.
Superior-inferior: it can be identified by orientation of proximal ureter which is directed inferiorly
WEIGHT: 150 g in males; 135 g in females.
MEASUREMENTS
Width: 6 cm. Thickness: (anteroposterior) 3 cm.
Length: 11 cm. (left kidney is slightly longer and narrower).
Their long axes are slightly oblique (being directed downward and laterally.
Transpyloric plane passes through the upper part of the hilum of the right kidney and through the lower part of the hilum of the left kidney.
Both kidneys move downward in vertical direction for 2.5 cm during respiration.
the lower poles are 7.5 cm away from the midline.
the hilum are 5 cm away from the midline
The upper poles are 2.5 cm away from the midline
LOCATION
The left kidney is little nearer to the median plane than the right.
The right kidney lies at a slightly lower level than the left one due to the presence of liver on the right side.
They occupy epigastric, hypochondriac, lumbar and umbilical regions (Fig. 1.1&1.2)
The kidneys lie on the posterior abdominal wall, one on each side of the vertebral column, behind the peritoneum (retroperitoneal), opposite 12th thoracic and upper three lumbar (T12–L3) vertebrae
The kidneys are
the major excretory organs and remove the waste products of
from the blood
thus
essential for maintaining the electrolyte and water balance in the tissue fluids of the body
necessary for survival.
excess of water and salts
protein metabolism
reddish-brown
two bean-shaped
MICROBIOLOGY OF URINARY TRACT INFECTIONS
Definitions
When discussing UTI's it is important to distinguish the following terms:
Urinary tract infection: It is the presence and multiplication of microorganisms in one or more structures of the urinary tract with associated tissue invasion.
Outcomes of UTI:
UTI usually results in:
Clinical presentations (Symptoms & signs).
Bacteriuria
Significant bacteriuria: This term was suggested by Kass in 1957 to differentiate between contamination of a collected urine sample and true infection since some urine samples may be contaminated with bacteria normally found on the skin (normal flora) during collection.
It is usually considered as the indication of infection
Pyuria
Sterile pyuria:
Viruses (e.g. adenovirus) are rare causes of UTIs.
Trichomonas vaginalis.
Infection with bacteria that require special media &/OR special growth conditions (e.g. N. gonorrhoeae and chlamydia trachomatris).
Infection with anaerobic bacteria which is not detected in routine aerobic culture.
Immune disorders that affect the kidneys e.g. post streptococcal glomerulonephritis.
Non-infectious causes of pyuria (e.g., stones, bilharzizasis & tumors).
Subtopic 2
Antibiotic treatment.
Defined as the presence of > 8 WBCs / HPF in urine examination, without bacterial growth in a concurrent urine culture. i.e., pyuria without apparent bacteriuria. i.e., pyuria without apparent bacteriuria
This estimation lacks standardization and that is why fluctuations in estimations of pus cells/HPF in urine are common.
It is obvious that estimation of pus cells /HPF in urine is variable and is affected by many factors as fluid intake and timing of urine collection.
Its best and most accurate measurement is by measuring the increase in excretion rate of PMNs in urine.
For simplicity, the presence of >8 pus cells/HPF in microscopic examination of the sediment of centrifuged urine is commonly used to correlate with significant pyuria.
This measurement is practically difficult for clinical use.
Pyuria is the hallmark of inflammation.
Other predisposing factors (Figure 2):
Diabetes mellitus.
Uncircumcised males due to bacterial colonization of the inside of the prepuce.
Catheterization is a major predisposing factor for UTI.
Back reflux of urine from the bladder up to the ureters (vesicoureteral reflux).
Functional obstruction due to loss of neurologic control of the bladder and sphincters.
Organic obstruction to complete bladder emptying (e.g. Prostatic hypertrophy, renal calculi, tumors and strictures).
Predisposing factors to UTI:
Any factor that causes obstruction or stasis of urine flow will predispose to UTI. These factors are divided into (Figure 5.2):
Pathogens-related factors.
Host-related factors.
Nearly 40 – 50% of females encounter UTI once in life with 50% recurrence within one year.
This is attributed to:
Pregnancy
Sexual intercourse facilitates the introduction of organisms up the urethra, so the incidence of UTI is higher among sexually active women.
Bacterial colonization of the periurethral area of the vagina.
The short female urethra.
MALES DO NOT USUALLY SUFFER UTI EXCEPT AFTER THE AGE OF 60Y WITH ENLARGEMENT OF THE PROSTATE.
UTI IS A DISEASE OF FEMALES.
Uropathogens (Figure 5.1):
Viral UTI is rare and is mainly seen in immunocompromised individuals, primarily transplant patients. Main causative viruses are adenoviruses and CMV. Patients usually present with fever, cystitis and gross haematuria.
Candida spp. (Particularly in nosocomial & catheter associated UTIs).
Haematogenous infection may be caused by Salmonella typhi, Staphylococcus aureus and Mycobacterium tuberculosis (renal tuberculosis).
Gram positive cocci (less common):
Staphylococcus epidermidis and Enterococci. (More often with nosocomial UTIs and infection in immunocompromised patients).
Staphylococcus saprophyticus. (Especially in young sexually active women).
Gram negative bacilli (The most common):
Non fermentative Gram negative Bailli:
Acinetobacter baumannii.
Pseudomonas aeruginosa.
Enterobacteriaceae
Other Enterobacteriaceae: Klebsiella, Proteus, Enterobacter and Citrobacter.
Escherichia coli is the commonest cause of UTI.
Routes of infection:
Less commonly, infection may result from haematogenous spread of an organism from a septic focus to the kidney.
Bacterial infection is usually acquired by the ascending route from the urethra to the bladder. The infection may then proceed to the kidney and may occasionally invade the bloodstream to cause septicemia.
UTI is most commonly caused by patient`s own intestinal flora (i.e. endogenous).
Complicated UTIs: Infections in a patient with anatomical or functional abnormalities in the urinary tract. Examples include pregnant women, UTI in men, obstruction and urinary retention from neurologic disease.
Uncomplicated UTIs: Infection in a healthy, non-pregnant, female patient with no anatomical or functional abnormalities in the urinary tract.
Colonization (asymptomatic bacteriuria): Organisms are present in the urine but are causing no illness or symptoms
Contamination: Organisms are introduced to the urine specimen during collection or processing.
Defense mechanisms of urinary tract:
High urea, organic acids & osmolality of urine.
Ureterovesical valve- like mechanism which prevents back urine reflux from bladder.
Antibacterial properties of prostatic secretion in males.
IgA of bladder mucosa (IgA).
Flushing effect of urine is the major mechanism (+++++).
Resident microflora of the urinary tract:
In females, the urethra exits the bladder near the vaginal area; the vagina could contribute to contamination of urine specimens by vaginal flora. In males, the foreskin when present may contribute to contamination and infection due to collection of bacteria beneath it.
Urine sterility is broken at distal urethra which is colonized by some microorganisms, the most common of which are:
Commensal mycobacteria & mycoplasma.
Anaerobes
Non-pathogenic Neisseria
Lactobacilli
Diphtheroids
Streptococcus viridans & non- hemolytic streptococci.
Coagulase negative staphylococci.
Urine is a sterile fluid until it reaches the urethra. All areas of the urinary tract above urethra in healthy individuals are typically sterile.
Renal medullary hyperosmolarity
characters present in the medulla
Source of energy mostly derived from ATP (for sodium pump).
Difference in permeability of both two limbs of the loop of Henel.
Some fluids run in opposite directions, parallel to and near to each other (countercurrents).
Medullary interstitial fluid is hyperosmotic to maintain. The production of concentrated urine.
Causes of hyperosmotic medullary interstitium:
Urea cycle (40%).
The countercurrent mechanisms (60%).
countercurrent multiplier (Loop of Henle).
Loop of Henle is a counter current multiplier:
Steps of countercurrent multiplier mechanism:
Thick ascending part of the loop has sodium pump which need energy derived from ATP.
Descending limb is permeable to water but not to Na+, while the ascending limb is impermeable to water but permeable to Na+.
Two currents of fluids run in opposite direction, parallel to & near to each other (descending & ascending limbs).
Hypertoncity in the renal medulla → shift of water from collecting tubules to renal interstitium & then to the blood of vasa recta → concentrated urine.
It is the mechanism by which the kidney can increase osmotic pressure in the renal medulla to 1200 mosmol/L (in cortex = 300 mosmol/L).
JUXTA GLOMERULAR APPARATUS (JGA)
Functions
Factors affecting renin release
Factors inhibiting renin release
Increase plasma level of K + (may be mediated by changes in NaCL delivery to the macula densa cells of DCT)
Vasopressin (ADH).
Increased Na and Cl concentration across macula densa cells
Angiotensin II ( +ve feedback mechanism)
Increased afferent arteriolar pressure (as in ↑↑ ABP) at the JG cells.
Factors stimulating renin release
Prostaglandins especially prostacyclin (PGI2) by direct action on JG cells.
Salt restriction and Clthat decrease Na + concentration across macula densa cells
Sympathetic stimulation or catecholamines (as in shock), acting on β1 receptors in the JGC
Renal ischemia
(in haemorrhage and renal artery stenosis) via ↑ 2. intrarenal baroreceptors
Hypotension ↓ renal blood flow
stimulate JG juxtaglomerular cells renin
formation of angiotensin I
By lung ACE angiotensin II
↑ Norepinephrine release at the sympathetic nerve endings.
↑ thirst sensation water intake
↑ ↑Aldosterone, ACTH and ADH
Generalized vc ↑ ABP
Macula densa cells act as receptors for NaCL in tubular fluid:
Increase NaCL in DCT release adenosine Ca++ release VC of afferent arteriole Decrease GFR (tubulo-glomerular feedback).
Decrease NaCL in DCT signals increase release of renin from juxta glomerular cells.
Juxta glomerular cells act as baroreceptors sensitive to decreased wall tension of the afferent arteriole release of renin act on angiotensinogen angiotensin I which converted by angiotensinogen converting enzyme (ACE) into angiotensin II restore blood pressure (when ABP drops as in haemorrhage).
Formed of three types of cells:
NB: Type I medullary interstitial cells present in the interstitial tissue of the medulla have a secretary function (prostaglandins, mainly PGE2).
lacis cells (extra-glomerular mesangial cells): special cells lie between macula densa and juxta glomerular cells (sometimes called Polar cushion cells).
Juxta glomerular cells (JGC, granular cells): muscles of the adjacent arterioles epithelioid cells and contain many granules (JGC contain B1-adrenergic receptors and are innervated by sympathetic nerve fibres).
Macula densa cells: tall crowded columnar epithelial cells of DCT.
It the region where the beginning of distal convoluted tubules lies close to both afferent and efferent arterioles that supply the nephron.
Pharma
Thiazides
Loop Diuretics (LDs)
These drugs are the most powerful of all diuretics (High ceiling diuretics).
As frusemide, bumetanide and torsemide which are sulfonamide derivatives and ethacrynic acid which is non-sulfonamide.
Git
عملي
فيديو
Histo
ميكرسكوب
فايل الكلية ٢
فايل الكلية ١
Liver function enzymes
Plasma proteins
billirubin
Jaundice
ملخص د.هيفاء منير
جدول د.إسلام جمال
فايل الكلية
محاضرات الكلية
Schistosoma
Trematode
Cestodes
Nematodes
Protozoa
Spleen
Liver
فارما عملي git
Anti-helmenthics
ملخص
Anti-Amebic Drugs
Classification of amebicidal drugs
Therapeutic agents are classified as
mixed (luminal and systemic) amebicides according to the site where the drug is effective (are effective against both the luminal and systemic forms of the disease, although luminal concentrations are too low for single-drug treatment.
Tinidazole
is a second-generation nitro-imidazole that is similar to metronidazole in spectrum of activity, absorption, adverse effects, and drug interactions. Tinidazole is as effective as metronidazole, with a shorter course of Treatment.
Metronidazole
Drug interactions
concomitant treatment with inducers of this enzymatic system, such as phenobarbital, enhances the rate of metabolism. Conversely, those drugs that inhibit this system, such as cimetidine, prolong the plasma half-life of metronidazole. The drug accumulates in patients with severe hepatic disease.
Adverse effects:
Note: The latter are reasons for discontinuing the drug.] If taken with alcohol, a disulfiram-like effect occurs.
Other effects include oral moniliasis (yeast infection of the mouth) and, rarely, neurotoxicologic problems, such as dizziness, vertigo, and numbness or paresthesias in the peripheral nervous system.
The most common adverse effects are those associated with the gastrointestinal tract, including nausea, vomiting, epigastric distress, and abdominal cramps, unpleasant, metallic taste is commonly experienced.
The parent drug and its metabolites are excreted in the urine.
Metabolism of the drug depends on hepatic oxidation of the metronidazole side chain by mixed-function oxidase, followed by glucuronylation.
-distributes well throughout body tissues and fluids. Therapeutic levels can be found in vaginal and seminal fluids, saliva, breast milk, and cerebrospinal fluid (CSF).
Metronidazole is completely and rapidly absorbed after oral administration
Mechanism of action:
Some anaerobic protozoal parasites (including amebas) possess ferrodoxin-like, low-redox-potential, electron-transport proteins that participate in metabolic electron removal reactions.
The nitro group of metronidazole is able to serve as an electron acceptor, forming reduced cytotoxic compounds that bind to proteins and DNA, resulting in cell death.
Clinical uses of metronidazol:
Metronidazole is the drug of choice for the treatment of
effective in the treatment of brain abscesses caused by these organisms.
pseudomembranous colitis caused by the anaerobic, gram-positive bacillus Clostridium difficile
Treatment of infections caused by
anaerobic gram negative bacilli
(for example, Bacteroides species).
anaerobic cocci
Trichomonas vaginalis
Giardia lamblia
For the treatment of amebiasis, it is usually administered with a luminal amebicide, such as iodoquinol or paromomycin. This combination provides cure rates of greater than 90 %
Nitroimidazole, is the mixed amebicide of choice for treating amebic infections and kills the E. histolytica trophozoites.
systemic (are effective against amebas in the intestinal wall and liver)
Emetine and dehydroemetine: are alternative agents for the treatment of amebiasis.
Adverse effects
Their use is limited by their toxicities (dehydroemetine is less toxic than emetine), and close clinical observation is necessary when these drugs are administered. They should not be taken for more than 5 days.
Pain at the site of injection, transient nausea, cardiotoxicity (for example, arrhythmias and congestive heart failure), neuromuscular weakness, dizziness, and rashes.
It is slowly metabolized and excreted, and it can accumulate. Its half-life in plasma is 5 days.
Emetine is concentrated in the liver, where it persists for a month after a single dose.
Intramuscular injection is the preferred route
They inhibit protein synthesis by blocking chain elongation.
Chloroquine:
Chloroquine is also effective in the treatment of malaria.
but it is not useful in treating luminal amebiasis
It eliminates trophozoites in liver abscesses,
is used
in combination with
diloxanide furoate
metronidazole
These drugs are useful for treating liver abscesses and intestinal wall infections caused by amebas.
luminal (act on the parasite in the lumen of the bowel)
After treatment of invasive intestinal or extraintestinal amebic disease is complete,
a luminal agent,
should be administered for treatment of the asymptomatic colonization state.
such as
paromomycin
Adverse effects: Gastrointestinal distress and diarrhea are the principal
Very little of the drug is absorbed on oral ingestion, but that which is absorbed is excreted in urine.
Because it is not significantly absorbed from the gastrointestinal tract
Paramomycin is directly amebicidal and also exerts its antiamebic actions by reducing the population of intestinal flora.
Its direct amebicidal action is probably due to the effects it has on cell membranes, causing leakage
an aminoglycoside antibiotic, is only effective against the intestinal (luminal) forms of E. histolytica and tapeworm,
diloxanide furoate
The mechanism of action of diloxanide furoate is unknown.
In the gut, diloxanide furoate is split into
furoic acid;
and
diloxanide
The unabsorbed diloxanide is the active antiamebic substance.
about 90% of the diloxanide is rapidly absorbed and then conjugated to form the glucuronide, which is promptly excreted in the urine
Diloxanide furoate is a dichloroacetamide derivative.
iodoquinol
Side effects: Rash, diarrhea, and dose-related peripheral neuropathy, including a rare optic neuritis. Long-term use of this drug should be avoided.
a halogenated 8-hydroxy quinolone, is amebicidal against E. histolytica and is effective against the luminal trophozoite and cyst forms.
Life cycle of Entamoeba histolytica
Large numbers of trophozoites within the colon wall can also lead to systemic invasion.
The trophozoites within the intestine are slowly carried toward the rectum, where they return to the cyst form and are excreted in feces.
Cysts, ingested through feces-contaminated food or water, pass into the lumen of the intestine, where the trophozoites are liberated. The trophozoites multiply, and they either invade and ulcerate the mucosa of the large intestine or simply feed on intestinal bacteria.
Note: One strategy for treating luminal amebiasis is to add antibiotics, such as tetracycline, to the treatment regimen, resulting in a reduction in intestinal flora, the ameba’s major food source.]
Entamoeba histolytica exists in two forms:
Trophozoites
that are labile but invasive and do not persist outside the body
cysts
that can survive outside the body
AIM OF THERAPY: Therapy is aimed not only at the acutely ill patient but also at those who are asymptomatic carriers, because dormant E. histolytica may cause future infections in the carrier and be a potential source of infection for others.
CLINICAL PICTURE: Amebiasis (also called amebic dysentery) is an infection of the intestinal tract caused by Entamoeba histolytica. The disease can be acute or chronic, with patients showing varying degrees of illness, from no symptoms to mild diarrhea to fulminating dysentery. The diagnosis is established by isolating E. histolytica from fresh feces.
Amebic infections are common among people in underdeveloped tropical and subtropical countries, where sanitary conditions and hygienic practices, are inadequate.
Peptic Ulcer treatment
Case
Management of Peptic Ulcer
Treatment of acute upper GIT hemorrhage complicating ulcer:
Surgery: for severe hemorrhage, perforation and gastric output obstruction. ❖ Compelling contraindications
Mg (OH)2 antacid after meals.
After 48 hours, treat as mentioned above.
After control of bleeding, give light meal with cold milk 50-100ml by gastric tube.
PPIs e.g. omeprazole 20mg I.V/12 hours.
Gastric lavage with ice cold saline.
Fresh blood transfusion & oxygen.
Hospitalization
Prevention of relapse: therapy is given for 6 month. Use either:
H2 blockers half dose e.g. ranitidine 150mg once daily
or
PPIs e.g. omeprazole 20mg before breakfast.
Patients with a known history of ulcer and NSAIDs use is unavoidable:
Co-therapy with PPIs or misoprostol.
Use the lowest dose and duration of therapy of NSAIDs.
Active ulcers associated with NSAIDs are treated with an appropriate course of PPIs and cessation of NSAIDs.
Peptic ulcer with NO H. pylori infection:
Either proton pump inhibitors (omeprazole) or H2 blockers (Ranitidine) for 4 weeks in duodenal ulcer or 8 weeks in gastric ulcer.
Peptic ulcer with H. pylori infection:
Drugs used for eradication of Helicobacter Pylori
Regimens of treatment
The antisecretory drugs used for this regimen include PPIs or H2 blockers.
Then PPIs should be continued once daily for 4-6 weeks.
These regimens are used for 14 days.
Dual: A + Anti-secretory drugs
Clarithromycin (500mg tid) + Omeprazole (20mg bid).
Or
Amoxicillin (500-750mg qid) + Omeprazole (20mg bid).
Triple • M + A + Antisecretory drugs.
Example
Metronidazole+ Amoxicillin/Clarithromycin+ PPIs “Omeprazole 20 mg bid”.
Quadruple • B + M + A + Anti-secretory drugs.
A
Clarithromycin (5oomg three times daily).
Tetracycline (500 mg four times daily).
Amoxicillin (500mg three times daily).
M
Tinidazole (500mg bid)
Metronidazole (250 mg three times daily)
B
Bismuth subsalicylate (2 tablets; 262 mg each).
Bismuth subcitrate (120mg four times daily).
Drugs used in treatment of peptic ulcer:
Cytoprotective agents
Carbenoxolone
PG analogues (Misoprostol).
Colloidal bismuth.
Sucralfate
Eradication of Helicobacter pylori.
Neutralization of gastric acidity:
Antacids
Drugs that reduce gastric acid secretion:
PG analogue.
Gastrin antagonists:
Somatostatin and Octreotide: decrease gastrin release.
Proglumide: blocks gastrin receptor.
Muscarinic (M1) antagonists.
H2 histamine receptor antagonists:
Famotidine: 40 mg at bedtime or 20 mg twice daily.
Nizatidine: 300 mg at bedtime or 150 mg twice daily.
Ranitidine: 300 mg at bedtime or 150 mg twice daily.
Cimetidine: 800mg at bedtime or 400mg twice daily.
Proton pump inhibitors (PPIs):
Duration of treatment: 4wks for duodenal ulcer & 8wks for gastric ulcer.
PPIs should be given 30 min-1h before meals (usually breakfast).
Pantoprazole: 40 mg/day.
Lansoprazole: 30 mg/day.
Esomeprazole: 40 mg/day.
Omeprazole: 20-40 mg/day.
General measures:
Diet: strict dietary regulation is important.
Drugs to be avoided:
Stomachics & digestants.
Histamine-like drugs e.g. phentolamine.
Histamine releasers e.g. morphine & curare.
Parasympathomimetics e.g. neostigmine.
Reserpine
Methylxanthines e.g. theophylline.
Adrenal steroid and ACTH.
Non-steroidal anti-inflammatory drugs (NSAIDs).
Avoid
Chewing gum.
Smoking
Beverages: xanthines (coffee & tea), carbonated beverages (cola) & alcohol.
Heavy meals, spicy food, vinegar, fried meat & meat extract.
However excess milk → excess Ca++ & protein → gastrin → rebound hyperacidity.
Milk in reasonable amounts. Milk contains:
Fats → enterogastrone hormone → ↓acidity & motility.
Proteins which produce demulcent effect on mucosa (with adsorption of HCl & pepsin) in addition to chemical neutralization of HCl.
Small, frequent, light meals.
Rest
Avoid physical stress ONLY in presence of complications.
Avoid mental stress (anxiolytics e.g. diazepam can be used).
Peptic Ulcer
Goals of therapy:
Prevention of recurrence [maintenance dose (half the normal dose) for at least 6 months].
Promotion of healing (4-8weeks for D.U. or 8-16 weeks for G.U).
Treatment of symptoms.
Complications: Upper GIT hemorrhage, perforation & cancer (gastric ulcer).
Vomiting (gastric ulcer)
Pain (duodenal ulcer).
Symptoms
Definition: Erosion of the gastric or duodenal mucosa.
Defensive factors:
N.B. PGs (E2 & E1) are responsible for all these process.
Gastric mucosal blood flow.
Processes of restitution and regeneration after cellular injury.
Tight intercellular junctions.
Thick lipoprotein coat.
Mucus & bicarbonate secretion.
Aggressive factors:
Agents disturbing mucus & bicarbonate gel-like layer:
Alcohol
Anemia
Pancreatic juice.
Reflux of bile.
Mucosal ischemia.
Drugs (NSAIDs & cortisone).
Bile
Pepsin
Gastric acid secretion.
نظري
فارما
Prokinetic & antiemetic drugs
الجزء الثانى
الجزء الأول
Therapeutic strategies for GERD & peptic ulcer
Therapeutic strategies for peptic ulcer
gastric mucosa protection
Anti Helicobacter Pylori
Antacids
Muscarinic antagonist
Histamine antagonists
Proton pump inhibitor treatment of peptic ulcer and gastroesophageal reflux disease
Therapeutic strategies for GERD
Treatment of Constipation and diarrhea
Laxatives • Patients not responding to dietary changes or fiber supplements should undergo medical evaluation prior to the initiation of long-term laxative treatment.
Danger of laxatives:
Serious G.I.T. disturbance: a. Spastic colitis. b. Signs &symptoms that are mistaken for G.I.T. disease. 3. Excessive excretion of Ca (osteomalacia of v.c.). 4. Steatorrhea & protein losing. 5. Secondary aldosteronism.
Perpetuating dependence upon drugs (laxative abuse).
Uses of laxatives:
Before &after anti-helminthics (saline).
Treatment of oral poison (saline).
Before and after surgery.
To avoid straining during defecation (elderly, cardiac, hernia). 3. Before operation & radiological examination of G.I.T.
Constipation
Fiber-rich diet, exercise, fluid, reassurance, treatment of causes (nonpharmacological). b. Bulk forming agents. c. In refractory cases → stimulant laxatives (lowest effective dose & for short periods).
Increase the volume of non-absorbable solid residue → stimulation of peristalsis & softening the feces [Bulk laxatives]. 2- Increase the water content [Osmotic laxatives]. 3- Increase motility and secretion [Stimulant laxatives]. 4- Alter consistency of the feces [Stool softener or Lubricant purgatives].
Stool softeners (lubricant purgatives):
Glycerin suppository.
Dioctyl sodium sulfosuccinate (Docusate):
❖ An ionic surface active agent (surfactant agents). ❖ Softens stool material, permitting water & lipid to penetrate.
Paraffin oil: Acts on colon
Side effects: 1. Aspiration can result in a severe lipid pneumonitis. 2. Interferes with the absorption of fat-soluble vitamins as well as Ca & phosphate (long-term use). 3. Absorbed (paraffinomas). 4. Leak through anal sphincter → pruritis anus. 5. Prolonged use → anal polypi. 6. Delays healing of wound after anorectal operations.
Lubricates fecal material, retarding water absorption from the stool.
It is not palatable (mixed with juices).
Stimulant laxatives:
Castor oil:
Anthraquinone (Emodin cathartics):
Side effects: 1. Colicky pain. 2. Abnormal color of urine. 3. Excreted in milk. 4. Brown pigmentation of the colon (melanosis coli).
Act within 6-12 hrs if given orally & within 2 hrs if given rectally.
Senna, Cascara, Rhubarb, Aloe.
In colon: bacteria → emodin → stimulate myenteric plexus → ↑colonic motility.
Glycosides → emodin + sugar.
Diphenylmethane derivatives:
Phenolphthalein (Modan)
Cardiac toxicity (removed from the market).
Long duration (enterohepatic circulation).
Bisacodyl (Dulcolax) ❖ Minimal systemic absorption and appears to be safe for acute &long term use.
Pink or red urine.
Individual effective doses.
Act on colon (act after 6-10 hrs) within 30-60 minutes if given rectally.
Osmotic laxatives:
Balanced polyethylene glycol (PEG):
No significant
Cramps or flatus.
Intravascular fluid or electrolyte shifts occur.
Safe for all patients.
❖ Contains an inert, non-absorbable, osmotically active sugar (PEG) with sodium sulfate, sodium chloride, sodium bicarbonate & potassium chloride.
Treatment or prevention of chronic constipation (smaller doses mixed with water or juices “17g/8 oz” and ingested daily).
Lavage solution prior to G.I.T. endoscope (ingested rapidly “4 L over 2-4 hrs.”).
Sorbitol & Lactulose (fructose + galactose):
❖ Non-absorbable sugars. ❖ Metabolized by colonic bacteria → Lactate + other organic acids (↓ PH).
Saline purgatives:
Uses: 1. Treatment of acute constipation or the prevention of chronic constipation. 2. Empty the bowel prior to surgical & radiological procedures. 3. Eliminate parasites.
Saline purgatives include: 1. Magnesium oxide (milk of magnesia): It should not be used for prolonged periods in patients with renal insufficiency due to risk of hypermagnesemia. 2. Potassium sodium tartarate. 3. Magnesium citrate or sulphate. 4. Sodium phosphate.
❖ Act on small intestine. ❖ Act after 2-3 hrs. ❖ Taken before breakfast on an empty stomach in isotonic solution. ❖ High doses of osmotically active agents produce prompt bowel evacuation (purgation) within 1-3 hours.
Bulk laxatives: ❖ Indigestible, hydrophilic colloids that absorb water, forming a bulky, emollient gel that distends the colon & promotes peristalsis.
1. Bloating & flatus (bacterial digestion of plant fibers within the colon). 2. Decreased Ca & iron absorption.
❖ Take several days to work (1-3 days). ❖ Should be taken with sufficient fluid.
Semi-synthetic disaccharides Lactulose.
Indigestible polysaccharides Bran. Methylcellulose.
Synthetic fibers polycarbophil.
Natural plant products Psyllium. Methylcellulose.
Laxatives: Promote defection of well-formed stool. • Purgatives: Promote defection of semi-solid stool. • Cathartics: Promote defecation of watery stool.
Anti-diarrheal agents
Lines of therapy:
Non-antimicrobial antidiarrheal agents: should not be used in patients with bloody diarrhea, high fever or systemic toxicity because of the risk of worsening underlying condition.
They are classified into:
Others
Octreotide
Side effects:
Bradycardia
Prolonged treatment→ hypothyroidism.
Alters the balance between insulin, glucagon, and growth hormone → hyperglycemia or, less frequently, → hypoglycemia (mild).
Inhibition of gallbladder contractility & alteration of fat absorption. Long-term use → formation of sludge or gallstones (↑50%) → acute cholecystitis (rarely).
Impaired pancreatic secretion may cause steatorrhea → fat-soluble vitamin deficiency.
Alteration of G.I.T. motility → nausea, abdominal pain, flatulence & diarrhea.
Other uses:
Pituitary tumors (e.g. acromegaly).
Pancreatic fistula (inhibit pancreatic secretion).
Gastrointestinal bleeding.
Uses
Other causes of diarrhea: it is effective in higher doses for the treatment of diarrhea due to vagotomy or dumping syndrome as well as for diarrhea caused by short bowel syndrome or AIDS.
Secretory diarrhea (carcinoid,VIP-oma).
Action:
In higher doses (100-250 mcg S.C.) → inhibits motility.
In low doses (50 mcg S.C.) → stimulate motility.
Inhibits intestinal secretion & has dose-related effects on bowel motility.
Somatostatin has short half life (3miutes).
Bile salts-binding resins: Cholestyramine or colestipol
Bind a number of drugs and reduce their absorption; hence, they should not be given within 2 hours of other drugs.
↓ Diarrhea caused by excess fecal bile acids.
Diseases of terminal ileum (e.g. Crohn’s disease) or surgical resection → malabsorpation of bile salts.
Conjugated bile salts are normally absorbed in the terminal ileum.
Phenothiazine (Chlorpromazine): antisecretory.
Agents which modify fluid and electrolyte transport.
Bismuth subsalicylate [Bi³ (antibacterial) + salicylate (inhibit PG)]: ❖ Coat ulcer.
Dose: Pepto-Bismol; 2 tablets (520mg) every 30 min.
Bismuth compound have direct antimicrobial activity against H pylori.
Prevent & treat traveler’s diarrhea (30 ml or 2 tablets four times daily).
Bismuth has direct antimicrobial effects & binds enterotoxins.
↓ stool frequency & liquidity in acute infectious diarrhea, due to salicylate inhibition of intestinal PG & chloride secretion.
They reduce secretion & or stimulate absorption of fluids.
GIT protective & adsorbents agents.
Kaolin. - Pectin. -Chalk. - Methylcellulose. - Charcoal.
Kaopectate (kaolin & pectin):
1.2-1.5 g after each loose bowel movement (maximum: 9g /d). ❖ Not absorbed (no adverse effects). ❖ Should not be taken within 2 hours of other medication.
Antimotility agents.
Lomotil: diphenoxylate (2.5 mg) + atropine (0.025mg).
Opioid agonists
Loperamide (Imodium):
Contraindications: 1- Chronic ulcerative colitis. 2- Young children. 3- Acute bacillary & amoebic dysentery.
Side effects: 1- Dry mouth, dizziness, headache, abdominal cramps, nausea and vomiting. 2- Paralytic ileus.
Relatively selective action on G.I.T.
Not crossing B.B.B.
Slow & incomplete absorption.
Diphenoxylate
Readily absorbed → systemic effects (sedation & addiction).
Stimulate intestinal opiate receptors (presynaptic). • Activate µ receptors on enteric neurons → ↑ K+ efflux → hyper polarization → inhibit Ach release →↓motility →↑ transit time → ↑absorption of fluid & electrolyte.
Anticholinergic: they reduce the motility and secretions of git as atropine and propantheline.
Anti-infective agents.
Rehydration
Pathophysiology of diarrhea:
Infection
Increased secretions and decreased absorption of fluids and electrolytes which lead to Na, water, and electrolyte disturbance.
Increased git motility.
Treatment of Inflammatory bowel Disease
Goal of therapy: Relieving abdominal pain and discomfort and improving bowel function.
Drugs Used in Treatment of Chronic Inflammatory Bowel Disease (IBD)
Aminosalicylates
Mesalamine compounds
Adverse effects:
Other aminosalicylate formulations are well tolerated:
Interstitial nephritis (rare, high doses of mesalamine).
Hypersensitivity (rare).
Olsalazine may cause secretory diarrhea (10%).
Sulfasalazine (→ sulfapyridine) has high incidence of side effects , >40% cannot tolerate therapeutic doses:
Impairs folate absorption.
Reversible oligospermia.
Hypersensitivity (fever, exfoliative dermatitis, pancreatitis, pneumonitis, hemolytic anemia, pericarditis, or hepatitis).
GIT upset, headache, arthralgia, bone marrow suppression & malaise.
Therapeutic uses:
Ulcerative colitis or Crohn’s disease confined to the rectum or distal colon, suppositories or enema are useful.
Ulcerative colitis or Crohn’s colitis that extends to the proximal colon, both azo & mesalamine compounds are useful.
Crohn’s disease involving the small bowel: mesalamine compounds, which release 5-ASA in the small intestine, have advantage over azo compounds.
First-line agents for treatment of mild to moderate active ulcerative colitis.
Balsalazide
After azo reductase, small amount of systemic absorption occurs.
<1% is absorbed
Sulfasalazine
Metabolite is excreted by the kidney.
Sulfapyridine undergoes hepatic metabolism.
After azo reductase, >85% of sulfapyridine is absorbed.
10% is absorbed.
Mesalamine
Metabolite is excreted by the kidneys.
5-ASA undergoes N-acetylation in the gut epithelium & liver.
20-30% of 5-ASA is absorbed.
Mechanism of action:
It may scavenger reactive oxygen metabolites.
Inhibits cellular functions of natural killer cells, mucosal lymphocytes, and macrophages
Inhibits the activity of nuclear factor-kB (NF-kB), an important transcription factor for pro-inflammatory cytokines
Interferes with the production of inflammatory cytokines.
5-ASA modulates inflammatory mediators derived from both the cyclooxygenase & lipooxygenase pathways.
Rowasa (enema formulations) & Canasa (suppositories): To deliver high concentration of 5-ASA to the rectum & sigmoid colon.
Subtopic
Asacol: has 5-ASA coated in pH-sensitive resin that dissolves at pH 7 (the pH of the distal ileum & proximal colon).
Pentasa: contains timed-release microgranules that release 5-ASA throughout the small intestine
Package of 5-ASA itself in various ways to deliver it to different segments of the small or large bowel.
Azo compounds:
Balsalazide (5-ASA + 4-aminobenzol-β-alanine).
Olsalazine (two molecules of 5-ASA).
Sulfasalazine (5-ASA “Active moiety” + Sulfapyridine “side effects”).
In terminal ileum & colon, bacteria cleave the azo bond by azo reductase, releasing the active 5-ASA.
Azo markedly reduces absorption of the parent drug from the small intestine
5-ASA bound by an azo (N=N) bond to an inert compound or to another 5-ASA molecule.
To overcome the rapid absorption of 5-ASA from the proximal small intestine, number of formulations has been designed to deliver 5-ASA to various distal segments of the small bowel or the colon.
Up to 80% of unformulated, aqueous 5-ASA is absorbed from the small intestine & does not reach the distal small bowel or colon in appreciable quantities.
Drugs used in treatment of IBD include:
Immunosuppressive agents: azathioprine - 6-mercaptopurine.
Corticosteroids: prednisolone.
Chronic inflammatory bowel disease (IBD) includes ulcerative colitis & Crohn's disease.
Drugs Used in Treatment of Irritable Bowel Syndrome
Irritable bowel syndrome:
idiopathic chronic, relapsing disorder, characterized by:
Alteration of bowel habits (diarrhea, constipation, or both).
Predominant constipation (Constipation-predominant IBS):
We can give
Tegaserod (partial 5-HT4 agonist). For short-term treatment of women with constipation-predominant IBS.
Osmotic laxatives, milk of magnesia.
Fiber supplements (however ↑gas production may exacerbate bloating and abdominal discomfort).
Predominant diarrhea (Diarrhea-predominant IBS):
Alosetron (5-HT3 antagonist): for women with severe diarrhea-predominant IBS.
Alosetron:
Side effects: Rare but serious G.I.T. toxicity may occur:
Restricted to يستخدم فقط مع women with severe diarrhea-predominant IBS.
Episodes of ischemic colitis (3 per1000).
Constipation (↑30%).
Dose: 1mg once or twice daily.
Uses: Women with sever irritable bowel syndrome with diarrhea.
Binds with higher affinity and dissociates more slowly from 5-HT3 R than other 5-HT3 antagonists (long duration).
❖ 5-HT3 antagonist.
Anti-diarrheal agents, loperamide.
Abdominal discomfort (pain, bloating, distention, or cramps).
Chronic abdominal pain:
Spasmolytics (Antispasmodics):
Direct spasmolytics:
Mebeverine (Colspasmin).
Nitrites
Aminophylline
Papaverine
Khellin
Volatiles oils.
Parasympathetic depressants:
Atropine substitutes:
Dicyclomin & hyoscyamine (inhibit M receptors in enteric plexus & on smooth muscle).
Metixene (Spasmocanulase).
Hyoscine-N-butyl bromide (Buscopan).
Propantheline
Atropine
Alter receptors for enteric neurotransmitters such as serotonin, affecting visceral afferent sensation.
Anti-cholinergic effects → reduce stool frequency & liquidity of stool.
At these doses, these agents have no effect on mood but may alter central processing of visceral afferent information.
Low doses of Tricyclic antidepresseants (TCAs) (amitriptyline or desipramine, 10-15mg/d).
Treatment of varicoceal Hemorrhag
Several drugs are available that reduce portal pressures. These may be used in the short term for the treatment of active variceal hemorrhage or long term to reduce the risk of hemorrhage.
Beta-Receptor–Blocking Drugs
Clinical Efficacy:
Among patients with a history of variceal hemorrhage, the likelihood of recurrent hemorrhage is 80% within 2 years. Non-selective β-blockers significantly reduce the rate of recurrent bleeding, although a reduction in mortality is unproved.
Among patients with cirrhosis and esophageal varices who have not previously had an episode of variceal hemorrhage, the incidence of bleeding among patient treated with non-selective β-blockers is 15% compared with 25% in control groups.
Non-selective β-blockers such as propranolol and nadolol are more effective than selective β1 blockers in reducing portal pressures.
Beta-blockers reduce portal venous pressures via a decrease in portal venous inflow. This decrease is due to:
Splanchnic vasoconstriction (β2 blockade) caused by the unopposed effect of systemic catecholamines on α-receptors.
Decrease in cardiac output (β1 blockade).
Vasopressin & Terlipressin
Terlipressin
Terlipressin is a vasopressin analog that appears to have similar efficacy to vasopressin with fewer adverse effects.
Vasopressin
Adverse Effects:
With systemic vasopressin (common):
The antidiuretic effects of vasopressin promote retention of free water, which can lead to hyponatremia, fluid retention, and pulmonary edema.
Nausea, abdominal cramps, and diarrhea (due to intestinal hyperactivity).
Systemic and peripheral vasoconstriction can lead to hypertension, myocardial ischemia or infarction, or mesenteric infarction. These effects may be reduced by coadministration of nitroglycerin, which:
Reduce the coronary and peripheral vascular vasospasm caused by vasopressin.
further reduce portal venous pressures (by reducing portohepatic vascular resistance)
In contrast, for patients with acute gastrointestinal bleeding from small bowel or large bowel vascular ectasias or diverticulosis, vasopressin may be infused—to promote vasospasm—into one of the branches of the superior or inferior mesenteric artery through an angiographically placed catheter.
Prior to the advent of octreotide, vasopressin was commonly used to treat acute variceal hemorrhage. However, because of its high adverse effect profile, it is no longer used for this purpose.
Although its primary physiologic role is to maintain serum osmolality, it is also a potent arterial vasoconstrictor. When administered intravenously by continuous infusion, it causes splanchnic arterial vasoconstriction that leads to reduced splanchnic perfusion and lowered portal venous pressures.
Vasopressin (antidiuretic hormone) is a polypeptide hormone secreted by the hypothalamus and stored in the posterior pituitary.
Somatostatin & Octreotide
Clinical Use:
They are generally administered for 3–5 days.
Although data from clinical trials are conflicting, these agents are probably effective in promoting initial hemostasis from bleeding esophageal varices.
Mechanism is poorly understood. They do not appear to induce direct contraction of vascular smooth muscle. Their activity may be mediated through inhibition of release of glucagon and other gut peptides that alter mesenteric blood flow.
In patients with cirrhosis and portal hypertension, intravenous somatostatin (250 mcg/h) or octreotide (50 mcg/h) reduces portal blood flow and variceal pressures.
Varices can rupture, leading to massive upper gastrointestinal bleeding.
Portal hypertension is caused by increased blood flow within the portal venous system and increased resistance to portal flow within the liver.
Portal hypertension most commonly occurs as a consequence of chronic liver disease
Treatment of Viral hepatitis
Human interferons (IFN)
Fatigue, myalgia, alopecia & weight loss.
Exacerbation of autoimmune diseases.
Bone marrow suppression.
Psychological depression & mood disorders.
Flu-like syndrome (common& resolves on continuous administration).
IFN-β:
multiple sclerosis.
some malignancies e.g. Kaposi sarcoma, malignant melanoma, renal cell carcinoma.
chronic HBV & HCV-
IFN-α
N.B. PEG-IFN allows sustained absorption & slower clearance → longer t1/2 than traditional IFN → once-weekly dosing.
The exact mechanism is unclear, but possibly they may act through:
Increase proliferation and survival of cytotoxic T cells.
Enhanced phagocytic activity.
Inhibition of viral penetration, translation, transcription, protein processing, maturation, and release.
They have wide range of antiviral and antitumor effects.
Glycoproteins normally synthesized by virally infected cells.
Treatment of chronic Hepatitis C Virus
New Treatment: Direct-acting antivirals (DDA)
Direct-acting antivirals (DAAs)
DAAs produce higher rates of SVR than the previous traditional therapy of pegIFN-α + ribavirin.
DAAs have fewer adverse effects than interferons and ribavirin (they target the viral structures rather than the patient's cells).
Any of the DAAs are not used as monotherapy (combined with other DAAs ± ribavirin ± pegIFN-α).
NS5A (replicase)inhibitors e.g. daclatasvir & ledipasvir
Inhibition of HCV NS5A replication complex (replicase) → ↓↓ viral replication.
NS5B polymerase inhibitors
Action: Inhibition of HCV RNA-dependent polymerase.
Non-nucleoside (dasabuvir)
Nucleoside (sofosbuvir)
Toxicity: sofosbuvir (Sovaldi) → headache & fatigue.
NS3/4A Protease inhibitors e.g. simeprevir
Toxicity: photosensitivity & rash.
HCV protease inhibitor → ↓↓ viral replication.
they target specific proteins of the virus and results in disruption of viral replication and infection
Ribavirin
Toxicity
Excreted by kidney → contraindicated in severe renal impairment.
Hemolytic anemia & teratogenicity
Clinical use
respiratory syncytial virus.
Chronic HCV
Mechanism
Inhibition of viral RNA polymerase.
Competitive inhibition of IMP (inositol monophosphate) dehydrogenase → inhibition of guanine nucleotides synthesis.
Treatment of chronic Hepatitis B Virus
Oral therapy includes lamivudine, adefovir, entecavir, tenofovir, or telbivudine.
Telbivudine
Telbivudine is eliminated by glomerular filtration as the unchanged drug, and no metabolites have been detected. The dose must be adjusted in renal failure.
The drug is administered orally, once a day, with or without food.
which can either compete with endogenous thymidine triphosphate for incorporation into DNA or else be incorporated into viral DNA, where it serves to terminate further elongation of the DNA chain.
The drug is phosphorylated intracellularly to the triphosphate
Telbivudine is a thymidine analog that can be used in the treatment of HBV.
Entecavir
Patients should be monitored closely for several months after discontinuation of therapy because of the possibility of severe hepatitis.
Very little
if any
drug is metabolized.
Entecavir undergoes both glomerular filtration and tubular secretion
Entecavir need only be given once a day.
Entecavir is a guanosine analog approved for the treatment of HBV infections. Following intracellular phosphorylation to the triphosphate, it competes with the natural substrate, deoxyguanosine triphosphate, for viral reverse transcriptase.
Tenofovir
Tenofovir is preferable than adefovir. (Why?).
Resistance has not been seen
Toxicity is minimal compared to adefovir.
AS an alternative for adefovir in lamivudine-resistant chronic hepatitis B, it showed an earlier and greater suppression of HBV DNA.
Tenofovir is a nucleotide analog approved for use in HIV and with activity against HBV.
Adefovir
Discontinuation of adefovir results in severe exacerbation of hepatitis in about 25 percent of patients.
Clearance is influenced by renal function. The drug should be used cautiously in patients with existing renal dysfunction.
Adefovir is administered once a day and is excreted in urine, with 45 percent as the active compound.
Adefovir dipivoxil is a nucleotide analog that is phosphorylated to adefovir diphosphate, which is then incorporated into viral DNA. This leads to termination of further DNA synthesis and prevents viral replication.
Lamivudine
Side effects
Lamivudine is well tolerated, with rare occurrences of headache and dizziness.
Pharmacokinetics
Dose reductions are necessary when there is moderate renal insufficiency
Seventy percent is excreted unchanged in urine.
Lamivudine is well absorbed orally and is widely distributed. Its plasma half-life is about 9 hours
Mechanism of action:
This compound competitively inhibits HBV DNA polymerase at concentrations that have negligible effects on host DNA polymerase.
Lamivudine must be phosphorylated by host cellular enzymes to the triphosphate (active) form
This cytosine analog is an inhibitor of both hepatitis B virus (HBV) DNA polymerase.
Traditional treatment: is the combination of peginterferon-α-2a or peginterferon-α-2b plus ribavirin, which is more effective than the combination of standard interferons and ribavirin.
Treatment of Hepatitis A Virus
No specific treatment options exist for HAV infections.
Nearly all individuals will have clinical resolution within 6 months of the infection, and a majority will have done so by 2 months.
The major viruses responsible for viral hepatitis are hepatitis A, hepatitis B, hepatitis C, delta hepatitis, and hepatitis E.
Hepatitis A, B and C are the most common.
Infection with delta hepatitis requires co infection with hepatitis B.
Both hepatitis A and E are spread through fecal–oral contamination; whereas hepatitis B, C, and delta are transmitted parenterally.
All share clinical, biochemical, immunoserologic, and histologic findings.
Micro
Hepatitis
Parasitic: Bilharziasis, Amebiasis, Hydatid disease.
Fungal: Actinomycosis, Candidiasis.
Viral: Viral hepatitis: Acute & Chronic.
However, hepatitis may be an unusual feature of a wide range of virus infections including Epstein-Barr virus, Cytomegalovirus and yellow fever virus.
For some viruses, their effect on the liver is the dominant feature of infection, and collectively these are known as the hepatitis viruses, identified by different letters of the alphabet.
Hepatitis E virus (HEV)
Treatment and Prevention: - Treatment is supportive only. There are no effective antiviral agents. There is also no vaccine at present.
Detection of the virus RNA in the stool.
Acute HEV infection is diagnosed by demonstration of an IgM anti-HEV response, but this test is only performed in reference laboratories.
The mortality from HEV infection is higher than with HAV, especially in pregnant women, where mortality rates are 10–20%, although the reasons for this are not clear.
Similar to hepatitis A, hepatitis E show no evidence of chronic infection or a carrier state (asymptomatic infection, acute hepatitis, and fulminant hepatitis).
Although HEV is entirely distinct virologically from HAV, it shares many epidemiological and clinical features. It is also transmitted via the feco-oral route.
The genome organization is unusual, and it is currently classified as caliciviridae .
the virus is about 32 to 34 nm in diameter.
HEV carries a positive ssRNA genome
Hepatitis D virus
Detection of the virus RNA in the serum is also diagnostic.
The hepatitis D virus is diagnosed by detection of delta antigen or possibly antibodies to delta (IgM) in the blood.
Patients who carry both HBV and HDV are at increased risk of serious liver disease and hepatocellular carcinoma.
Co-infection with HDV and HBV increases the risk that infection will become chronic
Infection with HDV can occur either at the same time as HBV infection (coinfection), or it can occur in someone who is already an HBV carrier (superinfection).
The risk factors for, and routes of transmission of, HDV are the same as those for HBV
HDV can only replicate in cells where HBV is also replicating.
helper function of HBV to replicate but is genetically completely different than HBV. HDV requires HBV for synthesis of envelope protein composed of HBsAg, which is used to encapsulate the HDV genome.
Its transcription and replication take place in the cell nucleus by means of a cellular polymerase. HDV is a defective virus single-stranded RNA virus that requires the
Delta agent is 36 nm in size and possesses a very short viral RNA containing 1683 nucleotides. This RNA is circular, has antisense (minus) polarity.
Hepatitis D virus (HDV) is an incomplete virus, consisting of a small piece of RNA, which encodes a single protein, its nucleocapsid contains the delta antigen.
Hepatitis B virus
Active immunization: Engerix and Recombivax which are subunit vaccines, consisting solely of HBsAg, is effective in inducing protective immunity against HBV infection. The standard regimen consists of three doses, at 0, 1 and 6 months. In Egypt it is administered at 2,4 and 6 months. The degree of protection induced by the vaccine is directly proportional to the level of anti-HBs achieved in the recipient’s serum. H
Passive immunization with hepatitis B immunoglobulin. This can be used for non-vaccinated individuals, or vaccine non-responders, to provide protection after an acute exposure incident. One particular use is for babies of high risk (i.e., HBeAg positive carrier mothers).
Screening of all blood and organ donors for evidence of current HBV infection by testing their sera for the presence of HBsAg to prevent the spread of HBV infection.
Diagnostic markers of hepatitis B virus
Serology inconclusive, mutants, therapeutic monitoring
Quantitative PCR
Exclusion of HBV HBc-IgG negative
Chronic infectious patient HBe and HBs-Ag, PCR
Recovered, healed HBs-Ab, HBc-IgG
Vaccine immunity HBs-Ab
Acute infection HBc-IgM, HBs-Ag
Detection of hepatitis markers i.e. antigens and antibodies in blood by ELISA:
N.B.: There is a period of several weeks when HBsAg has disappeared, but HBs-Ab is not yet detectable. This is the window phase. At this time the HBc-Ab is always +ve and can be used for diagnosis.
Occult HBV infection: by detection of DNA in peripheral monocytes of the blood. Occult HBV infection is a well-recognized clinical entity characterized by the detection of HBV-DNA in serum and/or in liver in the absence of detectable hepatitis B surface antigen (HBsAg). Occult HBV infection has been described also in patients without any serological markers of a past HBV infection.
Chronic hepatitis B: development of a chronic hepatitis B infection is revealed by a changed antigen antibody profile: HBs antigen (and raised transaminases) persists for over six months, whereby antibodies to HBe and HBs are not produced. A subsequent “late seroconversion” of HBe antigen to anti-HBe antibodies supports a better prognosis. Thorough clarification of chronic cases must include either immunohistological testing for HBV antigens in liver biopsies or PCR testing for the presence of viral DNA, and thus Dane particles, in patient serum.
Acute HBV infection is diagnosed by HBsAg or anti-HBc IgM in the serum.
Detection of viral DNA polymerase.
Detection of viral DNA by PCR.
Increased levels of liver enzymes.
Complications of chronic HBV infection:
0.5–1% of those infected experience a fulminant, often lethal, hepatitis.
In addition, HBV is a transforming virus as it may result in developing a primary tumor known as hepatocellular carcinoma (HCC) or hepatoma.
Liver Cirrhosis: occurs over a period of 20–30 years. It results in extensive replacement of liver tissue by fibrosis, and cirrhosis.
Forms of chronic infection:
Chronic aggressive hepatitis (CAH) with viral replication and a progressive course.
Chronic persistent hepatitis (CPH) without viral replication: the virus stimulates a chronic inflammatory response, which may compromise liver function and cause symptomatic chronic liver disease.
Healthy HBV carriers: in many chronic carriers, the presence of replicating virus does not impact on liver function, and they are not ill.
Consequences of infection:
Chronic hepatitis B: about 5-20% of adults infected with HBV become chronic carriers.
There may be such overwhelming liver damage that the patient goes into acute liver failure - fulminant hepatitis.
This occurs in ~ 1% of all HBV infections, and is more common than in HAV infection.
Alternatively, patients may present with an acute hepatitis, which is clinically indistinguishable from acute hepatitis A.
The majority of infections are asymptomatic.
The hepatic cell damage resulting from an HBV infection is not primarily due to cytopathic activity of the virus, but rather to a humoral and cellular immune response directed against the virus-induced membrane antigens (HBs, HBc) on the surface of the infected hepatocytes.
As explained above, in chronic carriers, HBV is a blood-borne virus. There are three routes of transmission of HBV:
Exposure to contaminated blood. This can occur via a number of mechanisms, most obviously by blood transfusion.
Sexual due to the presence of virus in genital tract secretions of chronic carriers.
Vertical i.e. from mother to baby. Globally, this is the most important route. Most commonly, this occurs perinatally.
Polymerase enzyme, derived from the Pol gene, has both DNA polymerase and reverse transcriptase activity.
Surface antigen (HBsAg), derived from the surface gene, surrounds the nucleoprotein core of the virus.
‘e’ antigen (HBeAg), also derived from the core gene.
Core antigen (HBcAg), derived from the core gene, encapsidates the viral genome.
Many 22 nm spherical particles and 22nm tubular particles of about 200 nm long are also found in serum. Both are composed of HBsAg and are non-infectious.
The complete, infectious virion, also known as a Dane particle, after its discoverer, has a diameter of 42 nm, the inner structure 27 nm.
It belongs to the hepadna virus family, which contains a number of viruses each of which infects the liver of its natural host.
HBV has an unusual, partially dsDNA genome
Hepatitis B virus (HBV) is an extremely important pathogen, especially in hospital medicine.
Hepatitis C Virus
Preventive measures include:
Implementation of infection control policies and procedures
Education and counseling
Implementation of sound sterilization policies
Screening and testing blood and blood products, plasma, organ and tissue
There is no vaccine, yet which induces protective immunity against HCV infection. Unfortunately, unlike with HBV, there is also no form of passive immunization for HCV.
Antigen detection assay:
Standardized commercial assay using a monoclonal antibody was developed for the qualitative detection of HCV core antigen. This assay is used to screen blood donations, as it reduces the serologic window period.
HCV-RNA PCR assay:
The RNA can be detected by means of RT-PCR and the course of therapy can be monitored with quantitative PCR. A negative NAT (nucleic acid amplification test) result following a positive serological test result is usually indicative of a resolved infection. However, intermittent or low-level viremia may occur during chronic infection and for this reason clinicians should perform a second NAT from 6 to 12 months later.
Detection of viral RNA in blood is useful in early diagnosis before seroconversion.
Antibodies detection:
Diagnosis of hepatitis C is done with antibody EIA using genetically engineered viral proteins.
Consequences of infection:
Chronic infection is associated with the risk of inflammatory hepatitis, and, over a period of years, end-stage liver failure due to cirrhosis. It also predisposes to the development of hepatocellular carcinoma.
The majority (> 75%) of HCV infections, whether in children or adults, are not cleared by the host, resulting in chronic infection. The reason for the high level of viral persistence is thought to be a pronounced mutability facilitating evasion of the immune defenses (quasispecies of RNA viruses).
Most infections are asymptomatic. Acute hepatitis may occur, but this is unusual.
Epidemiology
The transmission route is not apparent in many cases, giving rise to the expression “community- acquired infection".
The rate of transmission from carrier mother to baby is much less than for HBVcarrier mothers
In contrast to HBV, there is very little evidence that HCV spreads sexually.
HCV is classified as a blood-borne virus, and this explains the routes of transmission of the virus (transmission is mainly parenteral as HBV). Most HCV infections are acquired by injecting drug-users through sharing of blood contaminated needles, and/or syringes. Another important route is via receipt of contaminated blood or blood products
Not all HCV genome sequences are identical. HCV is now classified into six genotypes (denoted by Arabic numerals). In addition, there are subtypes within genotypes, denoted by alphabet letters. More than 100 subtypes have been described. Genotype 4a constitutes the majority of infections in Egypt.
HCV is an enveloped +ve single-stranded RNA virus and belongs to the Flaviviridae family (genus Hepacivirus).
HCV accounts for the majority of the hepatitis cases previously referred to as nonA, non-B hepatitis.
Hepatitis A virus (HAV)
Prophylaxis can be administered before exposure (pre-exposure prophylaxis) or after exposure (post-exposure prophylaxis):
Active immunization:
HAV vaccine only: as Havrix
The 1st is given at one to two years and the second 6 months later. It is given I.M in the deltoid region.
Also, it is recommended for all children in two doses.
The vaccine is recommended for people who travel abroad to endemic countries, and others at high risk (e.g. sewage workers).
A booster dose one year later will protect for several years
A single dose induces protective levels of antibody after ~ 2 weeks, which last for several months
An effective vaccine is composed of whole killed virus
Passive immunoprophylaxis:
IgG given within 2 weeks of exposure to HAV is up to 90% effective in preventing acute HAV infection.
By administration of normal human immunoglobulin, i.e. passive immunization.
The management of a patient with acute HAV infection is with bed rest and appropriate support. Only those severely affected will require hospitalization.
J
Identification of HAV in stools by immunoelectron microscopy.
IgG appears early in the convalescent phase and in individuals with past exposure giving a life-long immunity.
Detection of IgM which is consistent with acute HAV infection. It could be detected in serum or saliva.
HAV infection is diagnosed by demonstration of IgM anti-HAV in a serum sample. Two classes of anti-HAV are detectable: IgM and IgG.
Consequences of infection:
Fulminant hepatitis:
Chromic infection has not been reported to occur following HAV infection.
In about 0.1-1.0% of patients, the degree of liver damage is so overwhelming that the patient goes into acute liver failure or fulminant hepatitis.
Acute hepatitis:
As liver functions are impaired, the pigments (e.g. bilirubin) remain in the bloodstream, giving rise to jaundice seen as a yellowing of the skin and sclera of the eyes. Once the patient has become jaundiced, he/she often feels much better.
Clinically, acute hepatitis presents nonspecifically. Symptoms and signs include lethargy, loss of appetite (anorexia), nausea, fever, alcohol and cigarette intolerance (adults), right upper quadrant abdominal pain (arises as the inflamed liver swells and stretches its innervated capsule).
The incubation period is 2–6 weeks. The illness may last for several days, and it may be weeks or even months before the individual returns to full fitness.
Asymptomatic infection: this is age-related; children (who represent the vast majority of infected individuals worldwide) are very unlikely to present with clinical illness, whereas over half of adults infected will be jaundiced.
Epidemiology and pathogenesis:
The virus being highly resistant to the low pH found in the stomach. Excretion in the feces occurs 2 weeks before and 2 weeks after the appearance of jaundice. But some virus enters the bloodstream (i.e. there is a viremia) and thereby gains access to the liver.
Hepatitis A may rarely be transmitted through blood transfusion as there is a viremic phase in the infection.
Transmission of virus is via the fecal-oral route.
The virus is stable to treatment with ether, acids and heat (60°C for one hour) and is destroyed by boiling in water for 5 minutes or treatment with formalin or chlorine.
Only one serotype has been described.
HAV is a non-enveloped positive ssRNA genome, a 27-nm RNA and belongs to the family Picornaviridae genus Hepatovirus.
The commonest cause in the Egypt is viral infections of the liver (i.e. viral hepatitis).
Other hepatotropic viruses (CMV, EBV, Herpes & Rubella).
Bacterial: T.B., typhoid fever, syphilis.
Definition: Inflammation of hepatocytes and cell injury.
Diarrhea
Anemia if blood is also being lost due to damaged epithelium Complications of specific cause e.g. systemic infection
Dehydration
Microbial infections of GIT
Viral causes of diarrhea
Coronaviruses (Covid 19)
Adenovirus
Prevention:
A live non attenuated vaccine was used for the military recruits in the past, in the form of enteric coated capsules for serotypes 4,7 and 21, but it was stopped. Recently, another one is in its way to replace it.
Good hygiene including hand washing is the best way to avoid adenovirus infections.
Diseases
Gastrointestinal diseases: Gastroenteritis in infants (by types 40 and 41)
Most infections are self-limited, asymptomatic or mild and give long life immunity.
Transmission occurs by
swimming pool water
direct contact
feco-oral
respiratory droplets
Properties
There are about 52 serotypes
Replicates in the nucleus of the host cell causing cell lysis with viral release from the cell.
Has a unique fiber protruding from each of 12 vertices of its capsid, this fiber helps in the attachment of the virus to the host cell.
Icosahedral nucleocapsid.
Non-enveloped double stranded DNA virus.
Some adenovirus serotypes are oncogenic to lab animals, but oncogenesis has never been seen in humans.
Adenoviruses can infect several organs in the human body and causes latent infection in the adenoids, tonsils and lymphoid tissues.
Adenovirus was first isolated from adenoid tissue derived cell cultures, hence the name
Astrovirus
Most adult have antibodies against Astroviruses, suggesting that infection is common.
They cause watery diarrhea in infant and children. They are transmitted by the fecaloral route through contaminated food or water, person-to-person contact or contaminated surfaces.
There are at least 8 serotypes of human viruses recognized by immune electron microscope.
They contain single stranded positive sense RNA genome.
They exhibit a distinctive star like morphology in electron microscope (EM).
They are non-enveloped RNA viruses.
Norwalk virus
Treatment is symptomatic treatment. There is no vaccine.
Symptoms include diarrhea, nausea, vomiting, low grad fever, abdominal cramps headache and malaise. Dehydration is the most common complication.
Norwalk viruses are the most common cause of non-bacterial gastroenteritis that is occur in multiple setting as restaurants, nursing home, schools, cruise ships daycare centers and camps.
Norwalk is a small round non enveloped virus. It is containing linear, positive sense and non-segmented, single stranded RNA genome.
Rota virus
Vaccination
Rotateq is a new vaccine. It is live oral pentavalent human/bovine reassortant vaccine containing 5 reassortant rotaviruses. It is given to infants in USA in 3 oral doses 2ml each at 2, 4, 6 months.
Rotarix is live attenuated monovalent vaccine. It is given in 2 doses 1ml each in the first 6 months of life.
In 2006, two new vaccines against rotavirus A infection were shown to be safe and effective in children, and in June 2009 the World Health Organization recommended that rotavirus vaccination be included in all national immunization programs to provide protection against this virus
Reoviridae (Rotavirus)
Diagnosis and detection:
Detection of rising antibody titer by ELISA.
Polymerase chain reaction RT-PCR to detect virus nucleic acid in stools.
ELISA or RIA on stools for detection of the virus antigens.
Demonstration of the virus in stools by immune electron microscope.
Rotavirus infections rarely cause other complications and for a well-managed child the prognosis is excellent. There are rare reports of complications involving encephalitis and meningitis and recent studies have confirmed that rotavirus infection can cause viremia.
Symptoms often start with vomiting followed by four to eight days of profuse diarrhea. Dehydration is more common in rotavirus infection than in most of those caused by bacterial pathogens and is the most common cause of death related to rotavirus infection.
Once a child is infected by the virus, there is an incubation period of about two days before symptoms appear.
It infects and damages the cells that line the small intestine and causes gastroenteritis as a result of destruction of gut cells called "enterocytes". Also, the virus releases a unique protein that acts as enterotoxin which enhances the secretion of fluids from the intestinal cells.
Rotaviruses are stable in the environment. Sanitary measures adequate for eliminating bacteria and parasites seem to be ineffective in control of rotavirus, as the incidence of rotavirus infection in countries with high and low health standards is similar.
The virus is transmitted by the fecal-oral route via contact with contaminated hands, surfaces and objects, and possibly by the respiratory route.
Serotypes and epidemiology:
Rotavirus is usually an easily managed disease of childhood, but worldwide more than 500,000 children under five years of age still die from rotavirus infection each year and almost two million more become severely ill.
By the age of five, nearly every child in the world has been infected with rotavirus at least once. However, with each infection, immunity develops, and subsequent infections are less severe; adults are rarely affected.
There are five species of this virus, referred to as A, B, C, D, and E. Rotavirus A, the most common, causes more than 90% of infections in humans.
General properties:
It is a genus of non-enveloped, double-stranded, segmented RNA viruses, which is icosahedral and has double-layered capsid. It has wheel-like distinct appearance under EM. The virus belongs to the family Reoviridae.
Rotavirus is the most common cause of severe diarrhea among infants and young children.
Bacterial causes of diarehea
Food poisoning
For tracing the source of food poisoning: isolated organisms from food, patients and food handlers are identified by typing methods: e.g Phage typing
It depends on the manifestations, type of food, as well as detection of the organism or toxin in food remnants, vomitus or stools.
Differential Diagnosis of food poisoning
V. parahemolyticus
Sea food
Hemolysis
6-36 hrs
B. cereus
Recovery in few days
Reheated rice
2-6 hrs
Cl. botulinum
Fatal
Canned food
Neurotoxin
Neurological
12-24 hrs
Cl. perfringens
Meat
6-18 hrs
Salmonella
Recovery after treatment
Meat and eggs
Proliferation in gut
Vomiting, diarrhea, fever
12-48 hrs
Staph. Aureus most common cause
Outcome
Recovery in 1-2 days
Food type
Carbohydrate, milk, milk products
Enterotoxin
C/P clincal picture
Vomiting, diarrhea
IP incupation period
1-6 hrs
It is characterized by acute onset, usually < 10 day, and usually is self-limiting.
Occurs due to consumption of food contaminated by microorganisms or their toxins.
Salmonellae
Enteric (Typhoid and Paratyphoid) Fever
Septicemia with metastatic abscesses
Blood culture is positive and antibiotic treatment is as typhoid fever.
Infection occurs by ingestion and the organism reaches via blood stream to many organs especially the periosteum, lungs or meninges. Metastatic abscesses frequently occur on top of damaged tissues e.g. infarcts and aortic aneurysms.
Mainly caused by S. choleraesuis in patients with underlying chronic disease such as cancer or child with enterocolitis.
Salmonella food poisoning
Laboratory diagnosis: isolation of the organism from the stools, vomitus and food remnants. Blood culture and serological tests is of no value (no blood invasion).
Clinical picture: the disease is characterized by nausea, vomiting, abdominal pain, severe diarrhea and mild fever. The disease is self-limited, and recovery occurs within one week.
Incubation period: 12 - 48 hours. This type of food poisoning is an infection (enteritis). That is why the incubation period is relatively long compared to other types caused by preformed toxins.
Infection is confined to the intestine with no blood invasion.
Mode of transmission: ingestion of improperly cooked meat of infected animals, improperly cooked eggs of infected birds or food contaminated with animal excreta.
Reservoir of infection: animals and poultry. Humans can be a source of infection
It is caused by Salmonella typhimurium and Salmonella enteritidis.
Immunoprophylaxis
The older killed whole-cell vaccine:
although this vaccine is no longer recommended, because of higher rate of side effects (mainly pain and inflammation at the site of the injection), it is still used in countries where the newer preparations are not available.
The injectable typhoid polysaccharide vaccine:
N. B.:
Both are between 50% to 80% protective.
Boosters are recommended every five years for the oral vaccine and every two years for the injectable form.
not given to children below 2 years.
Given by IM injection of 0.5 ml 2 weeks before travel to endemic areas
The live, oral Ty21a vaccine:
Not all recipients of this vaccine will be fully protected against typhoid fever, so should continue to take necessary personal precautions.
Should not be given to children less than 6 years.
Contains the attenuated strain Salmonella typhi Ty21a (1,2). It will not afford protection against species other than Salmonella typhi.
Live attenuated vaccine for oral administration only.
Generally: sanitary measures like water sanitation, and proper sewage disposal should be done. Carriers are excluded from food handling and treated.
Cholecystectomy is needed in those having gall bladder problems.
For chronic carriers, ampicillin, trimethoprim-sulfamethoxazole, and ciprofloxacin may be effective.
However, definitive treatment of typhoid fever (enteric fever) is based on susceptibility tests, as multiple drug resistance (MDR); transmitted genetically by plasmids is a major problem.
Drugs commonly used are chloramphenicol, ampicillin and trimethoprimsulfamethoxazole, fluoroquinolones, or 3rd generation cephalosporins.
Diagnosis of carriers: high titer of anti-Vi antibodies is detected in carriers of Salmonella typhi
Urinary carriers are diagnosed by isolating the organism from the urine. Note that excretion of bacteria in stool and urine is intermittent, so repeated examination is necessary.
Gall bladder carriers are diagnosed by isolating the organism from the stool. The patient is given first a cholagogue to empty the gall bladder followed by saline purge.
During the second week of fever and onwards:
Serologic diagnosis: can be done by Widal test and more sensitive methods as ELISA and immunoblot assay.
Widal test: a tube agglutination test designed to detect anti-salmonella antibodies titer in the patient’s serum.
Interpretations of Widal test:
If only one serum sample is available, the following facts should be considered:
False negative results may occur
Early antibiotic treatment lowers antibody titer due to reduction of the antigenic mass.
If the test is done very early in the first week of illness.
Non-enteric infection: false positive results may be seen in some non-enteric infections by other Salmonellae or autoimmune diseases due to the presence of cross reacting antibodies.
Past vaccinated or past infected individuals: high anti-H titer is only important, as anti-O antibodies appear and disappear earlier than anti-H antibodies.
The endemicity of the disease: in endemic areas, e. g., Egypt, high titer of O and H ≥ 1 /160 is indicative of recent infection. Titers ≤ 1/80 are not significant due to repeated exposure to subclinical infection (community titer).
For proper interpretation a rising titer is measured. It is 4-fold rise of titer in second serum samples collected one week after the first one.
Urine culture: urine is centrifuged. Deposit is cultured on MacConkey or DCA medium. Identification is carried out as mentioned before. Repeated examination is needed.
Stools culture: stool sample is inoculated first in selenite broth or tetrathionate broth overnight. Then subcultured on MacConkey or DCA media. Identification is done as before. Excretion of bacteria in the stool may be intermittent. Repeated examination is needed.
During the first week of fever:
Subculture is done on MacConkey or DCA medium. Identification is done by:
Slide agglutination test with specific antisera.
Biochemical reactions.
Microscopic (wet film and Gram stain).
colony morphology
Clot culture: blood is allowed to clot. Clot is used for culture and the serum is separated for serological test.
Bone marrow cultures: always positive, versus about 66% positivity of regular blood culture.
Blood culture. It is done by adding 5 – 10 ml blood of the patient to 50 – 100 ml trypticase soy broth.
Specimen: blood, stool, urine and serum depending on the stage.
Complications: include intestinal hemorrhage and perforation. When untreated, enteric fever persists for three weeks to a month. Death occurs in between 10% and 30% of untreated cases.
Symptoms: appear after the incubation period in the form of fever, headache, malaise, tender abdomen, constipation, enlarged spleen and rose spots on the abdomen.
Incubation period: 1 – 2 weeks.
The patient may recover or become chronic carrier of Salmonella either in the gall bladder or in the urinary tract:
If in the urinary tract, it will be excreted in urine. The prevalence of urinary bilharziasis among Egyptians favors the occurrence of urinary carriers.
If in the gall bladder, it will be excreted in the stool intermittently. The carriage of Salmonella in the gall bladder is favored by the presence of gall bladder stones.
From the gall bladder, it reinvades the intestine where the organism multiplies in Peyer's patches and gut lymphoid tissues. It may rarely reach the periosteum, lungs or meninges.
The organism spreads in the phagocytic cells to the liver, gall bladder, spleen, kidney and bone marrow where it multiplies and passes again to the blood causing secondary bacteremia leading to fever and other clinical manifestations of enteric fever.
The primary site of infection is the small intestine where M cells; specialized epithelial cells take up and transcytoses the organism to the phagocytic cells in the Peyer's patches that spread the organism to the mesenteric lymph nodes where it multiplies and then passes through the lymphatics to the blood stream causing primary bacteremia for 1-2 weeks (incubation period).
Lower dose is sufficient with the presence of Vi antigen.
Infectious dose of about 10^6 organisms are needed
Feco-oral route after ingestion of contaminated food or drinks e.g. raw vegetables, fruits, raw shellfish and milk products.
Source of infection:
Cases or carriers who discharge the organism with their feces or urine.
Enteric fever is strictly, human disease. It is endemic in Egypt and caused by serotypes typhi, paratyphi A, B and C.
Capsular Vi antigen in Salmonella typhi can retard phagocytosis by PMN cells favoring uptake by macrophages in which these serotypes can multiply extensively.
Persistence in macrophages (facultative intracellular). Genes for macrophage survival are present in another pathogenicity island.
Two pathogenicity islands that code for a contact secretion system and effector proteins.
Pili: mediate adherence with host cells.
All salmonellae are indole, and urease negative.
Salmonella typhi and Salmonella paratyphi B and C produce H2S
ferment glucose, maltose and mannite with production of acid only in Salmonella typhi or acid and gas in Salmonella paratyphi.
On MacConkey agar, they produce pale yellow non-lactose fermenting colonies.
They can grow on nutrient agar.
facultative anaerobe
In carriers of Salmonella typhi, the bacteria usually acquire a capsule that possess Vi antigen.
Gram negative bacilli, motile and non-capsulated.
Molecular and antigenic classification:
The most important serotypes are:
Serotype that cause septicemia with metastatic abscesses; Salmonella choleraesuis belongs to group C.
Serotypes that cause food poisoning; Salmonella typhimurium and Salmonella enteritidis belong to groups B and D; respectively.
N.B.: There is minor antigenic sharing of O between Salmonella typhi and paratyphi organisms. However, H antigen is specific for each of them.
Serotypes that cause enteric fever (paratyphoid and typhoid fever) are:
Salmonella typhi belongs to group D.
Salmonella paratyphi A, B and C belong to groups A, B and C; respectively.
Group I include the species Salmonella enterica that includes more than 1400 serotypes that, nearly all, cause human infections. These serotypes are grouped by somatic O antigen into 9 groups (A-I).
Salmonellae are classified according to DNA-DNA hybridization into 7 groups.
Antigenic structure:
Virulent strains have virulence (Vi) or capsular antigen.
They are divided into serogroups according to the O antigen and into serotypes according to the specific H antigen
Salmonellae have somatic (O) and flagellar (H) antigens.
Salmonellae are often pathogenic to humans and animals. Some types have broad host range, while others are restricted only to humans.
Clostridium difficile (Pseudomembranous enterocolitis)
Treatment: ▪ Discontinuing the initial antibiotics and oral administration of metronidazole or vancomycin.
Stool samples are examined for C. difficile exotoxins by ELISA or latex assay
Examination by colonoscopy can reveal red inflamed mucosa and areas of white exudates called pseudomembranes on the surface of the large intestine. Necrosis of the mucosal surface occurs underneath the pseudomembranes.
Reservoir and mode of infection:
Symptoms typically develop 5-10 days after initiation of antibiotic therapy. However, they can develop after a single day of antibiotic use or can occur as late as 10 weeks after antibiotic cessation.
This disease is characterized by profuse, mucoid, greenish, malodorous watery stools, abdominal cramping and fever.
C. difficile is responsible for antibiotic associated pseudomembranous enterocolitis, which can follow the use of broad-spectrum antibiotics, e. g., fluoroquinolones, macrolides, clindamycin, beta-lactam/beta-lactamase inhibitors, and all generations of cephalosporins. These antibiotics can wipe out part of the normal intestinal flora, allowing the pathogenic and drug resistant C. difficile to multiply and superinfect the colon releasing its exotoxins.
C. difficile is transmitted by feco-oral route. The hands of hospital personnel are important vehicle.
C. difficile endospores are found in hospitals. The organism is carried in the intestinal tract of 3% of general population and 30% of hospitalized patients.
Toxins
Toxin B is cytotoxic to colonic mucosal cells leading to pseudomembrane formation.
Toxin A is enterotoxin that causes watery diarrhea.
Yersinia enterocolitica and Yersinia pseudotuberculosis
Clinical findings:
Yersiniosis
Yersinosis is self- limiting and does not require treatment. Severe infections are treated by doxycycline in combination with aminoglycosides.
Is a food-borne illness is primarily caused by Yersinia enterocolitica and less frequently by Yersinia pseudotuberculosis. Infection is usually self- limiting
In adult infection is usually accompanied by lower abdominal pain, fever and leukocytosis. Sources of human infections include dogs, pigs and cats.
In infants and young children, infection usually produces a watery diarrhea without dysentery.
Some strains of Y. enterocolitica are invasive and toxigenic (producing heat-stable enterotoxin).
Causes gastroenteritis and occasionally acute mesenteric lymphadenitis.
Y. pseudotuberculosis:
Occasionally Y. pseudotuberculosis invades the blood causing septicemia which is usually fatal
Causes acute mesenteric lymphadenitis with severe lower abdominal pain.
Person-to-person transmission with either of these organisms is probably rare.
Transmission to humans by eating contaminated raw or inadequately cooked pork products.
They occur in domestic animals, farm animals and water.
SHIGELLAE
Endotoxin (LPS): similar to other Gram negative bacilli. It contributes to the irritation of the bowel wall.
Shigella dysenteriae type I (Shiga bacillus) exotoxin:
It is similar to EHEC E. coli verotoxin.
The toxin has enterotoxic, cytotoxic and neurotoxic effects where:
It acts as cytotoxic; cause necrosis and ulceration of mucosa, with formation of pseudomembrane.
It acts as neurotoxic; causes meningism, convulsions and coma in severe fatal infections when it is absorbed in the blood.
It acts as enterotoxin that causes watery diarrhea observed in early cases.
It is heat labile.
Invasiveness: by a contact secretion system that injects a set of invasion antigens into enterocytes to facilitate the invasion process. They are encoded by a very large plasmid that has also other genes for attachment.
All Shigellae are anaerogenic i.e. do not produce gas upon sugar fermentation and are H2S and urease negative.
Other Shigella species ferment glucose and mannite with acid production only. Shigella sonnei is a late lactose fermenter.
Shigella dysenteriae ferments glucose only with production of acid only.
Cultural characters: on MacConkey or DCA media, it produces pale yellow, nonlactose fermenting colonies.
Morphology: Gram negative bacilli, non-motile, non-capsulated.
Serological classification:
Shigella lacks H antigen. It is divided into four serogroups according to O antigen:
Group D: S. sonnei which includes one serotype.
Group C: S. boydii which includes 18 serotypes.
Group B: S. flexneri which includes 8 serotypes.
Group A: S. dysenteriae which includes 13 serotypes.
They are strict human pathogens causing bacillary dysentery.
Bacillary dysentery
Antimicrobials are used to shorten the period of illness, e. g., ampicillin, ciprofloxacin or 3rd generation cephalosporins.
Fluid and electrolyte replacement are very important.
Good observation of food handlers.
Good hygienic measures for personal habits, food preparation and flies’ control.
Proper water sanitation and sewage disposal.
Antibiotic susceptibility tests should be done as antibiotic resistance is very high.
Identification of the growing colonies is done according to
latex agglutination with specific antisera.
biochemical reactions
Gram stain
wet film
morphology
Selenite broth for 24 hours
Subculture is done on MacConkey’s medium or DCA.
Microscopic examination: demonstrates pus cells and red blood cells.
Specimen: stools. It usually contains visible blood and mucous.
Clinical picture:
Recovery occurs spontaneously in most cases. However, in children and elderly, dehydration, acidosis and death may occur. Few cases remain as chronic carriers.
Symptoms: fever, abdominal pain, diarrhea which starts watery and profuse then become small volume, bloody with mucous. This represents dysentery syndrome which has a triad of
frequent, small-volume, bloody, mucoid stools
painful straining to pass stools (tenesmus)
abdominal cramps,
No blood invasion occurs in healthy individuals. If shiga toxin is produced, it is absorbed in the blood leading to severe form of the disease.
The organism then reaches the submucosa where it evokes a severe inflammatory response.
Invaded cells undergo apoptosis and sloughing which causes ulceration of the mucosal layer.
The organism invades the intestinal M cells. Then, it multiplies in the cytoplasm and starts to invade epithelial cells via their basolateral pole and subsequently to spread laterally from one enterocyte to other adjacent cells.
Infection starts in the distal ileum and colonic mucosa.
Infectious dose: very low as few as 100 organisms can cause the disease. This is attributed to its acid resistance which allows it to survive passage through the stomach to reach the intestine.
Four (F) help in transmission of the organism; flies, feces, fingers and food.
Feco-oral route through person to person contact or by ingestion of contaminated food or water.
Reservoir of infection: infected humans are the only reservoirs. No animal reservoir.
Escherichia coli
Selected antibiotics can be helpful.
Treatment depends on correction of dehydration and electrolyte imbalance.
E. coli from feces should be further tested serologically and for virulence to confirm its enteric pathogenicity as follows:
DNA probe or PCR to detect genes of toxin production.
ELISA can be used also to test for toxin production.
Tissue culture methods for toxin production (ETEC, EHEC), invasiveness (EIEC), and adherence (EPEC, EaggEC).
Slide agglutination using specific antisera.
Identification: After 24h incubation, colonies should be examined for morphology, Gram stain, oxidase, and other biochemical reactions.
Culture: on MacConkey agar as well as blood agar and incubated at 37°C.
Specimens: feces
Diarrheagenic E. coli include the following types:
Enteroaggregative E. coli (EaggEC)
adheres to intestinal mucosa in patches and produce heat-stable enterotoxin, causing persistent diarrhea in children. A novel strain of E. coli O104:H4 bacteria caused a serious outbreak of foodborne illness (fresh vegetables were the source of infection) focused in northern Germany in May through June 2011. The illness was characterized by bloody diarrhea, with a high frequency of serious complications, including hemolytic uremic syndrome (HUS), a condition that requires urgent treatment. The outbreak has caused by an enteroaggregative E. coli (EAEC) strain that had acquired the genes to produce Shiga toxins.
Enteroinvasive E. coli (EIEC)
EIEC strains cause a disease identical to that caused by Shigella spp. but do not produce shiga toxin.
Enteropathogenic E. coli (EPEC)
EPEC strains adhere tightly to the intestinal mucosa and interfere with water absorption by mucosal cells. They are a common cause of infantile diarrhea.
Enterohaemorrhagic E. coli (EHEC)
Ground beef (hamburger) has caused many outbreaks. Six new strains of potentially lethal E. coli bacteria should also be checked for especially in meat. They have the ability to produce the same deadly toxins that can lead to bloody diarrheal illness, kidney failure and death as E. coli O157. They are known as Shiga toxin-producing E. coli, or STECs, the group includes the strains O26, O111, O103, O121, O45 and O145.
Owing to production of shiga toxin, EHEC strains cause bloody diarrhea or hemorrhagic colitis (a disease similar to shigella dysentery) and also hemolytic uremic syndrome (HUS) as a potentially fatal complication. E. coli serotype O157:H7 is the most common strain associated with this disease.
Verotoxin enzymatically modifies the ribosome site (28S-RNA of 60S subunit) where amino acyl tRNA binds. This alteration blocks protein synthesis, leading to cell death.
Also known as verotoxigenic E. coli they produce a toxin known as verotoxin (because it is toxic to vero cells in tissue culture) or shiga toxin-producing E. coli.
Enterotoxigenic E. coli (ETEC)
Enterotoxigenic E. coli (ETEC) strains cause severe diarrhea in infants and children and traveler’s diarrhea in adults. Infection is acquired through ingestion of contaminated food and water and can occur in an epidemic form.
The ST stimulates the activity of guanylate cyclase in intestinal epithelial cells leading to formation of cGMP, resulting also in loss of fluids from Ife intestine.
The labile toxin (LT) consists of 2 subunits A and B. It attaches via its B subunit to the gut mucosa, then the A subunit enters the cell and activates adenylate cyclase resulting in conversion of ATP to cAMP. Increased level of cAMP induces the active secretion of CL and inhibits the absorption of Na+, creating an electrolyte imbalance and loss of copious amounts of fluids from the intestine. LT has a mode of action similar to cholera toxin.
Gram-negative bacilli, usually motile and some are capsulated.
E. coli is the major facultative anaerobe in the bowel and is part of its normal flora.
Non-halophilic vibrios
Non O1 V. cholerae (NCV or NAG)
V. cholera O1: classical, El Tor biotype
Halophilic vibrios
is another aquatic organism that produces a very small number of septic infections, mainly in immunosuppressed patients.
Vibrio parahemolyticus is a halophilic (salt-friendly) species found in warm oceans. These bacteria can cause gastroenteritis epidemics.
The pathogen is transmitted to humans with food (seafood, raw fish). The illness is transient in most cases and symptomatic therapy is sufficient. Virulent strains produce a hemolysin. It grows on TCBS producing green colonies (do not ferment sucrose).
Some members can cause disease in man or animal. The most clinically important species is V. cholerae.
Vibrio cholerae
Prevention
Specific measures
Vaccines
Oral
Recombinant oral live vaccine: Gene of V. CholeraeO1 has been inserted to Salmonella typhi Ty21a.
Cholera Toxin B subunit vaccine.
B subunit-whole cell vaccine (BS-WC): Oral vaccine containing killed cells and purified subunit B is used in some countries.
Advantages: it induces the formation of antibacterial and antitoxin antibodies. Because it is given orally, it induces production of IgA in the intestinal mucosa which plays the major role in providing immunity against infection.
Parenteral: A killed whole cell vaccine is available (Koll's vaccine): killed bacteria given in 2 intramuscular doses with one-week interval. It usually gives low level of protection, about 50%, that lasts only for 6 months.
Disadvantages: it induces formation of antibacterial not antitoxin antibodies. In addition, as it is given intramuscularly, it induces production of IgM and IgG antibodies in the blood of the patient while immunity against V. cholerae is mainly mediated by IgA in the intestine.
Chemoprophylaxis by tetracyclines for exposed persons.
General measures
Quarantine measures: Cholera is a quarantinable disease. As cholera is a highly infectious disease, during an epidemic, any newly discovered cases of cholera should be quarantined until the disease is controlled
Proper washing of foods before eating and good observation of food handlers.
Increased sanitation and purification of water and isolation of patients.
Tetracyclines can be used to shorten the period of excretion of the organism in convalescence. However, tetracycline resistant strains have emerged.
The most important part in the treatment of cholera is intravenous fluids to correct fluid and electrolyte imbalance.
Laboratory diagnosis:
Diagnosis of secondary cases during an epidemic: Cases are diagnosed just by microscopic examination of stools for comma shaped bacilli with darting motility which can be immobilized by specific anti-O sera.
Diagnosis of the first case in a non-endemic area and carrier state: Full lab. diagnosis must be done before reporting the case as positive for V. cholera.
Direct methods for detection of V. cholerae O1 and O139 in stool include
immunofluorescence and immunoassay for antigen detection and PCR for detection of cholera toxin gene.
Culture: Stool is inoculated in alkaline peptone water for 6-8h. On alkaline peptone water, V. cholera forms a surface pellicle. Subculture is done from surface pellicle on TCBS where it produces yellow colonies. Yellow colonies are further identified by:
Agglutination tests with specific anti-O1 and 139 sera.
Gram stained smears: Gram negative comma shaped bacilli.
cholera red reaction and string test positive and TSI inoculation.
String test: when a colony is emulsified in a drop of 0.5% sodium deoxycholate in distilled water, within one minute, the cells lyse and DNA strings when a loopful is lifted from the slide. This test differentiates Vibrio cholerae from Aeromonas hydrophila which is string test negative.
Cholera red reaction: when Vibrio cholerae is inoculated in nitrate peptone medium, nitrate is reduced to nitrite and indole is produced from decomposition of tryptophan into peptone. Nitrite combines with indole producing nitroso-indole compound which gives red color on addition of few drops of strong sulphuric acid (H2SO4).
positive oxidase and indole tests,
sugar fermentation (glucose, maltose, mannite & sucrose),
Biochemical reactions:
Wet mount film: Darting motility.
Specimen: Rice watery stools and rectal swabs from carrier
Mode of transmission:
Carrier state: Convalescent carrier can harbor the organism in the gall bladder and secrete it for about 4 to 5 weeks.
Chronic carrier state is rarely observed only with El Tor biotype.
Infectious dose: Infectious dose of cholera is high. As many as 10^10 organisms or more are needed to produce disease in normal healthy individual. Ingestion of food may lower the infectious dose due to its buffering capacity as well as the decrease in gastric acidity as with antacid uptake. Infection starts in the ileum where the organism attaches to the intestinal microvilli and starts to produce its exotoxin. The infection remains localized with no invasion into the blood.
Ingestion of inadequately cooked marine shellfish which may function as reservoirs of infection.
By ingestion of water or food that has been fecally contaminated by patients’ or carriers’ excreta.
Disease caused by Vibrio cholerae:
Cholera
Complications include dehydration, hypokalemia, metabolic acidosis, shock and death.
Clinical picture of cholera: Sudden onset of severe vomiting, rice watery diarrhea with abdominal cramps. Diarrhea is severe; the patient may lose up to 20 liters fluid per day.
Incubation period: 1-4 days.
Cholera disease is endemic in Indian subcontinent, but it may occur in epidemics and even worldwide pandemics.
Resistance
El Tor biotype survives longer periods than the classical type.
It is susceptible to many disinfectants, including 0.05% sodium hypochlorite, 70% ethanol, 2% glutaraldehyde, 8% formaldehyde, 10% hydrogen peroxide and iodine–based disinfectants.
V. cholerae is tolerant for alkaline conditions but are sensitive to acids and cold temperatures
Virulence factors:
Mucinase: It degrades the mucous layer covering the intestinal cells and it is said to play a role in the pathogenesis.
Enterotoxin [cholera toxin CT] or choleragen Toxins:
The net result is excessive secretion of chloride, potassium, bicarbonate, sodium and water molecules out of cell into the lumen leading to a severe form of diarrhea.
Subunit A1 activates adenylate cyclase enzyme which in turn increases the level of cAMP.
The B subunits bind to receptor on cell surface of enterocytes enabling subunit A1 to enter the cells and perform its activity.
Itis formed of two toxic (A1, A2) and five binding (B) subunits
The genes for cholera toxin are carried by a temperate bacteriophage.
CT is a heat labile exotoxin, antigenically and pharmacologically identical in all sero and bio types
Heat stable endotoxin.
A colonizing factor known as the toxin-coregulated pilus (TCP). It is encoded on a VPI pathogenicity island and its expression is regulated together with cholera toxin (CT). It helps the organism colonizing the intestinal mucosa.
El Tor
Resistant
Positive
Clasical
Sensitivity to phage IV
Sensitive
Polymyxin B susceptibility
Susceptible
V.P reaction
Hemagglutination of chicken RBC
Hemolysis of sheep RBC
Negative
There are three distinct O1 serotypes, named Ogawa, Inaba and Hikojima, and each type may display the "classical" or El Tor biotype.
O1 serogroup is also divided according to biochemical reactions into 2 biotypes: the classic V. cholerae and El Tor.
Non O1/non-O 139 cause sporadic cholera - like disease.
Strains designated (O1) and (O139) are known to be responsible for epidemic cholera.
O antigens distinguish strains of V. cholerae into not less than 139 known serogroups, almost all are non-virulent
Cultural characters:
On thiosulphate citrate bile sucrose agar (TCBS), it produces yellow colonies.
It grows on alkaline peptone water, forming a surface pellicle.
Growth is favored by alkaline pH (8.5-9.5).
It can grow on simple media.
Highly aerobic organism.
They are motile with single polar flagellum. Motility is characteristic and appears in darting form.
On prolonged cultivation, they become straight rods.
Gram negative curved bacilli on primary isolation.
Vibrios are comma shaped Gram-negative rods. They are commonly found as saprophytes in surface water, mainly saltwater, and soil.
C. fetus, C. lari are rare causes of systemic infections such as bacteremia, meningitis and pneumonia.
Campylobacter coli: also causes diarrhea in humans.
Campylobacter jejuni: considered the most important clinically. It causes 95% of Campylobacter enterocolitis especially in children.
Antibiotics are needed only in severe cases. C. jejuni is sensitive to erythromycin and ciprofloxacin.
Fluid and electrolyte replacement are necessary (if indicated).
Laboratory diagnosis:
Serologic diagnosis for antibodies detection in serum is useful in cases of autoimmune complications.
Culture
Biochemical reactions: oxidase and catalase positive, while urease is negative. The later differentiates the organism from Helicobacter spp. As helicobacter is urease positive
Growing colonies are identified by Gram staining, biochemical reactions and sensitivity to antibiotics.
Stool sample is cultured on Skirrow’s medium and incubated at 42 ˚C for 2-4 days.
Direct detection by:
ELISA or PCR.
Staining with 1% basic fuchsin is a sensitive and inexpensive method for rapid diagnosis of acutely ill patients without waiting for culture results in order to start treatment.
Gram stained smears to show the characteristic morphology.
Wet smears examination shows the characteristic motility.
Specimen: stools
Clinical picture:
Infections may be complicated two weeks later, or more by:
Reactive arthritis which is also autoimmune
Guillian-Barré syndrome: an autoimmune disease due to formation of cross reacting antibodies that attacks the axons or the myelin sheath of neurons.
Bacteremia rarely occur in immunocompromised and neonates.
The condition is usually self-limited within 7-10 days.
Enterocolitis begins as watery foul-smelling diarrhea followed by bloody stools, fever and severe abdominal pain.
Infection starts in the jejunum.
Infectious dose is relatively low; just a few hundreds of the organism is needed.
Children are the most commonly affected worldwide.
Infection is acquired by consumption of water and foods like unpasteurized milk, meat and poultry contaminated with feces of domestic animals.
Campylobacter jejuni infection is a zoonotic disease. Animal reservoirs include domestic animals (dogs, cats, cattle) and poultry.
Virulence factors:
Cytolethal distending toxin (CDT) that arrests cell division and may destroy the mucosal cells.
Enterotoxin production that irritates the intestine leading to secretory diarrhea.
Invasiveness of the lining mucosa of the small intestine (jejunum) leading to cell damage and inflammatory diarrhea.
Characteristic darting or cork-screw motility.
Cultural characters:
It takes 2-4 days to grow.
Skirrow’s medium is selective and enriched media for Campylobacter. It is a blood containing medium that contains vancomycin, polymyxin and trimethoprim as selective agents.
It is also thermophilic as it grows best at 42 ˚C.
Campylobacter is microaerophilic and capnophilic organism. This means that it grows better in presence of 5% oxygen and 10% CO2.
Morphology
They have darting motility using a single flagellum at one or both poles.
Campylobacter jejuni are small Gram negative, comma, S or gull wing shaped rods.
noninflammatory (watery, non-bloody) or inflammatory (bloody).
Differences between watery and bloody diarrhea:
Bloody Diarrhea:
Bacterial causes of bloody diarrhea:
Y. enterocolitica
Shigella
Salmonella (nontyphoidal)
Enteroinvasive E. coli
Enterohemorrhagic E. coli; O157:H7
Campylobacter
Infection typically in colon
Both red blood cells and white blood cells in stool, i.e., inflammatory response - Often febrile
Watery Diarrhea:
Bacterial causing watery diarrhea:
V. cholerae
VIBRIOS
Non-halophilic vibrios
Halophilic vibrios
V. mimicus
V. vulnificus
V. alginolyticus
V. parahaemolyticus
Some members can cause disease in man or animal. The most clinically important species is V. cholerae.
Vibrios are comma shaped Gram-negative rods. They are commonly found as saprophytes in surface water, mainly saltwater, and soil.
C. difficile
Enterotoxigenic E. coli
Infection typically in small intestine
Typically, afebrile
No red blood cells or white blood cells in stool, i.e., no inflammation
acute (up to 4 weeks), persistent (between 2 and 4 weeks), and chronic (longer than 4 weeks).
Inflammatory diarrhea (dysentery) is defined as inflammation of the intestine with passage of frequent stools containing blood and pus in addition to fever and abdominal cramps.
Relative diarrhea is defined as increase in the number of bowel movements per day or an increase in the looseness of stools compared with an individual usual bowel habit.
Absolute diarrhea is defined as more than five bowel movements per day or liquid stools.
Diarrhea: increase in the frequency of bowel movements, an increase in the looseness of stool or both.
Para
Urinary Schistosomiasis
Schistosomiasis is caused by blood trematodes.
The three main species infecting humans are
In addition, other species of schistosomes, which parasitize birds and mammals, can cause cercarial dermatitis in humans.
S. japonicum
S. mansoni
cause intestinal schistosomiasis.
Schistosoma haematobium
Life cycle:
Transmission
Infective stage: bifurcate cercaria swimming in water; Fig. (5.7) Fig. (5.4)
Hosts
Intermediate host (snail): Bulinus truncatus; Fig. (5.5).
Definitive host: man is the only final host for adult S. haematobium Fig. (5.4); (No animal reservoir host).
Habitat
S. haematobium adult worms most often occur in the perivesical & pelvic venous plexuses of urinary bladder, but it can also be found in the rectal venules.
Geographical distribution: Schistosoma haematobium is found in:
Middle East – Africa.
Nile Valley (Upper Egypt-Sudan- Ethiopia).
causes urinary schistosomiasis.
- intestinal protozoa
Protozoa of the small intestine
Intestinal Coccidia
They share the following common characters:
All are obligatory intracellular parasites.
They all produce oocyst in their life cycle, the infective stage.
They are opportunistic parasites: which are parasites that usually don’t cause the disease in immunocompetent individuals, but they cause severe manifestations in immunocompromised hosts.
Members of this class (Cryptosporidium spp., Isospora belli, Cyclospora cayetanensis)
Cryptosporidium
Swallowing the oocyst in food or water contaminated with calves' feces.
N.B. There are two types of oocysts:
Thick-walled resulting in external autoinfection.
Thin-walled resulting in internal autoinfection.
Infective stage: Oocyst containing four sporozoites.
Diagnostic stage: Oocyst.
Habitat: Small intestine. The parasite is intracellular, extracytoplasmic. In immunocompromised hosts, it may be present in other sites like; lung, liver, gall bladder, and pancreas.
Hosts: Both calves and man act as definitive and intermediate hosts.
Cryptosporidium is a coccidian parasite found worldwide, especially in tropical areas. It infects many mammalian hosts, mainly calves (new born cows). The species which infects man is called C. parvum.
Mastigophora (Flagellates)
These are group of protozoa which move by flagellae (mastigote).
Intestinal flagellates
Giardia lamblia (Giardia intestinalis)
Prevention and Control:
Treatment of both symptomatic and asymptomatic patients to reduce transmission.
Sanitary disposal of human feces.
Safe water supply.
Careful washing of fruits and vegetables.
Personal cleanliness and hygiene.
Tinidazole (Fasigyn): 2gm (4 tablets) as a single oral dose
Treatment should be repeated after 7-10 days to avoid autoinfection.
Metronidazole (Flagyl): 250 mg tablet (three times daily) for 5-10 days. Children receive 5mg/kg three times daily for five days.
Entero-test (string test): Aspiration of duodenal fluid to detect the diagnostic stages.
Molecular diagnosis (PCR).
Serodiagnosis: Antibodies to Giardia are detected by IFA and ELISA.
Detection of the parasite antigen in the stools (coproantigen) by ELISA immunochromatographic strip tests and indirect immunofluorescent tests (IIF) using monoclonal antibodies.
Stools examination:
N.B. Repeated stools examination for three times is recommended as the parasite is intermittently shed
Microscopy: Detection of cyst or trophozoite in the stools sample by direct smear, eosin and iodine smears, and concentration methods.
Macroscopy: Fecal specimens containing G. lamblia may have an offensive odor, are pale in color and are fatty.
Clinical picture
Occasionally, the gall bladder may be involved causing biliary colic and jaundice. N.B. The main hazard of Giardia is functional, as it causes marked impairment in digestion and absorption of food, particularly fat substances. This is attributed mainly to inhibiting intestinal and pancreatic enzymes and bile salt consumption by trophozoites.
Malabsorption is characteristic of giardiasis, mainly steatorrhea (excessive loss of fat in stool). This may lead to weight loss and debilitation.
Chronic giardiasis: Recurrent attacks of diarrhea alternating with constipation.
Acute giardiasis: Sudden onset of explosive watery, foul-smelling diarrhea. Fat malabsorption (steatorrhea) and flatulence are common. The stools is loose, bulky, fatty, frothy but without blood. Severe symptoms in immunocompromised patients are persistent diarrhea (steatorrhea), hypoproteinemia, fat-soluble vitamin deficiency, lactose intolerance, weight loss, biliary colic, and jaundice.
Many cases are asymptomatic passing cysts in feces.
The prepatent period is usually two weeks.
Mode(s) of infection:
Encystation is the final stage of the life cycle in which trophozoite withdraws its flagellae and turns into a cyst.
Excystation is the dissolving of the outer cyst wall to give rise to trophozoite.
The cyst is the dormant infective form and the only form that can survive outside the human body.
The trophozoite is the active vegetative, dividing form that colonizes the proximal intestine and never invades the intestinal wall, grows on bile salts resulting in impairment of fat absorption and digestion (steatorrhea).
Mechanical transmission by flies.
Person-to-person transmission occurs especially in nurseries, male homosexuals, mentally ill persons, and school children. Giardia is considered one of the nosocomial (hospital-transmitted) infections.
External autoinfection (handto-mouth transmission) may occur.
Swallowing the cyst in contaminated food or water.
Infective stage: Mature quadrinucleated cyst.
Diagnostic stage: Cyst or trophozoite.
Habitat: Small intestine (duodenum and jejunum). The parasite sometimes inhabits the gall bladder and biliary tract.
Definitive host: Man.
Reservoir hosts: Many animals (e.g. dogs, rodents, monkeys). Giardia is considered one of the most known zoonotic diseases.
Geographical distribution: Worldwide. Giardia is one of the most common parasites incriminated in water-borne outbreaks, especially children.
The structure of the protozoan cell is formed of a cytoplasmic body and a nucleus.
Protozoa have a wide range of sizes (1-150µ).
Each protozoan is a complete unit capable of performing all functions.
Protozoal infections of the intestine Protozoa are unicellular organisms that occur singly or in colony formation.
platyhelminthes
- intestinal nematode
- Strongyloides stercoralis (Dwarf thread worm)
Mass treatment: Periodic mass treatment of the population.
Sanitary disposal of human feces: Usage as fertilizer should be after storage or chemical disinfection of feces.
Abstinence from walking barefooted.
Personal prophylaxis: Wearing shoes and other protective clothes as gloves for people handling mud or working in mines, gardening
Treatment: Thiabendazole: 25 mg/kg twice daily for 2-3 days. A 5-7 days course for disseminated infection.
Serological tests as IHAT and ELISA.
Eosinophilia (blood picture).
Stools culture.
Baermann's technique increase the chance of detection of larvae.
Rhabditiform larvae in stools (diagnostic) or the sputum by direct simple smear.
N.B. It has two types of cycles; free-living and parasitic.
Free-living cycle: If the external environmental conditions are favorable for freeliving, the rhabditiform larvae molt in two days to free-living males and females
Strongyloidiasis in individuals receiving immunosuppressive therapy, which reduces the body's natural resistance, is considered an opportunistic helminthic infection due to the extensive invasion by the adult worms.
Sometimes the filariform larvae reaching the lung may stay for a few days and develop to adults (in cases of immunosuppression of man). Adults mate, so worms, eggs, and rhabditiform larvae may be detected in the bronchial epithelium and may be found in the sputum.
So, larvae join the venous circulation by auto-infection and complete their direct life cycle. More and more adults are formed in the intestine until they reach the state of hyper-infection.
Parasitic cycle: When the external environmental conditions are unfavorable for free-living, rhabditiform larvae grow and molt in 2-3 days to filariform larvae that infect man
Mode(s) of infection:
Autoinfection: If the rhabditiform larvae change into filariform larvae in the lumen of the intestine and penetrate the intestinal mucosa (Internal autoinfection). In other cases, these larvae come out and penetrate the perianal skin (External autoinfection).
Filariform larvae penetrate the skin of hands and the feet, getting in contact with contaminated soils.
The infective stage: Filariform larvae.
RH: Dogs and Chimpanzees have been found infected with strains like those of man.
Diagnostic stage: The rhabditiform larvae.
Habitat: The parasitic males and females live in the small intestine of man (duodenum and jejunum).
It depends on the intensity of infection and the host immunity, so:
In immunosuppressed case, massive penetration of the perianal skin by the filariform larvae causes linear urticarial lesions over the thigh and trunk; this is called larva currens (racing larvae). The filariform larvae in the lung alveoli gain access to the general circulation and may invade the brain, intestine, lymph glands, liver, and rarely the myocardium.
During the intestinal phase:
Skin manifestations during the chronic course of infection are linear tortuous urticarial lesions over thighs, back, and trunk resembling cutaneous larva migrans (CLM).
Anorexia, loss of weight and weakness.
Epigastric pain and tenderness due to duodenitis.
Nausea, vomiting, and diarrhea (cochin-china diarrhea) alternating with constipation.
The mature females invade and penetrate the intestinal mucosa to lay eggs then larvae, leading to acute mucosal inflammation, sloughing, secondary infection, and necrosis.
Mucosa heals by fibrosis which affects the intestine's physiological functions.
On the migration phase: fever, cough, expectoration, hemoptysis, leukocytosis, and eosinophilia due to petechial hemorrhage in the pulmonary tissue caused by the metabolites and end products of the larvae in the lungs. In severe infection, lobar pneumonitis and consolidation may result.
During the invasive stage, skin irritation and creeping eruption sometimes ground itching, occurs due to the secretory products of the penetrating filariform larvae. There may be dermatitis, papular, vesicular, or pustular eruption.
Geographical distribution: Worldwide.
Hook worms
Mass treatment of cases.
Abstinence from defecation on the ground.
Abstinence from walking barefooted
Personal prophylaxis: People work in mines or handling mud as farmers must wear shoes and gloves.
Treatment:
Treatment of anemia: Replacement therapy of iron by ferrous sulphate or gluconate 200 mg tds and folic acid 5 mg for three months.
Elimination of adult worms by Albendazole (zentol), the drug of choice in a single oral dose of 400 mg (80% cure); or 200mg daily for three successive days (100% cure).
Detection of anemia by blood iron level, hemoglobin, and ferritin analysis.
Detection of larvae in soil by Baermann`s technique.
Estimation of the intensity of infection by Stoll`s technique.
Detection of eggs in the stools.
Physical and mental retardation is caused by toxins secreted by the worms. These toxins affect the endocrine glands.
Edema and ascites are caused by hypoalbuminemia.
Myocarditis and cardiac dilatation are due to anemia.
Intestinal stage: The adult attaches to intestinal wall by its buccal capsule causing inflammation, malabsorption and sucks blood for feeding.
Hook worm anemia (Egyptian chlorosis, Miner’s anemia): hypochromic iron deficiency anemia as the adult sucks blood for feeding (each worm sucks about 0.5 ml/day). Anaemia is also due to decreased iron intake and depletion of iron stores. Dyspnea on mild exertion, weakness, apathyلامبالاه, pallor, tachycardia, and heart failure commonly occur.
Mechanisms of anemia:
Enteritis (due to 2ry infection) decrease absorption of iron.
Toxic bone marrow depression.
Anticoagulant secretion by cephalic glands (continued bleeding after detachment).
Tear by buccal capsule.
There is malabsorption, hypoalbuminemia, and edema due to reversible changes of villi.
Hook worm enteropathy: Epigastric pain, abdominal discomfort, nausea, vomiting, loss of appetite, sometimes there is geophagy or pica, diarrhea with occult blood in stools.
Migration stage (Loffler’s syndrome): due to migration of the infective larvae to the lung leads to pneumonia. There is fever, dry cough, bronchitis, lung infiltration, and asthma.
Invasion stage: due to penetrating the skin by the infective larvae. There is dermatitis, itching, erythema, papules, and pustules (ground itch). The most affected site is the feet and hands.
Larval tropisms:
The infective larvae are attracted to the host by different tropisms:
Positive phototropism: Larva moves toward light.
Negative geotropism: larva moves against gravity.
Positive histotropism: larvae move toward host tissues
Positive chemotropism: larva moves toward O2.
Positive hygrotropism: larva moves toward moist.
Positive thermotropism: Larva is drawn toward heat or warmth.
N.B
Some A. duodenale larvae, following penetration of the host skin, can become dormant (in the intestine or muscle).
In addition, infection by A. duodenale may probably also occur by the oral and transmammary routes.
Most adult worms are eliminated in 1 to 2 years, but longevity records can reach several years
Adult worms live in the small intestine lumen, where they attach to the intestinal wall with resultant blood loss by the host
The larvae reach the small intestine, where they reside and mature into adults.
They penetrate the pulmonary alveoli, ascend the bronchial tree to the pharynx, and are swallowed.
On contact with the human host, the larvae penetrate the skin and are carried through the veins to the heart and then to the lungs.
These infective larvae can survive 3 to 4 weeks in favorable environmental conditions.
The released rhabditiform larvae grow in the feces and/or the soil, and after 5 to 10 days (and two molts), they become filariform (third-stage) larvae that are infective.
Under favorable conditions (moisture, warmth, shade), larvae hatch in 1 to 2 days.
Immature eggs pass in the feces (20,000 eggs/female/day in Ancylostoma and 10,000 eggs/female/ day in Necator americanus).
Trans-mammary: Larva passes to suckling baby through milk.
Via mucous membrane penetration when infective larvae are eaten with contaminated vegetables.
Percutaneous route: filariform larva penetrates the skin.
Infective stage: Third stage filariform larva in soil.
Diagnostic stage: Egg containing 4-cell stage in stools.
Habitat: Small intestine of man (jejunum).
Geographical distribution: Tropical and subtropical countries, including Egypt. Necator Americanus is common in Africa, America, and Southern Asia.
- Anclystoma dudenale
- Necxator americanus
Capillaria philippinensis
Health education:
Avoid eating undercooked fish.
Proper cooking of fish.
Treatment and follow-up of cases.
Mebendazole: 200 mg twice daily for 20 days (less effective against larvae).
Albendazole: 200 mg twice daily for 10 days.
Detection of larvae or adults in stools or intestinal biopsies.
Detection of eggs in stools: Thick shelled with polar plugs 40x20µ in size.
Clinical picture in endemic areas gives a clue to the diagnosis.
Symptomatic:
Death due to heart failure, pneumonia or hyperkalemia in severe infection.
Severe protein-losing enteropathy leads to malabsorption, severe weight loss (cachexia), edema, and muscle wasting.
Abdominal pain, watery diarrhea, and vomiting lead to excessive fluid loss and dehydration.
Maybe asymptomatic.
Pathogenesis: - Direct mucosal invasion of adult worms results in inflammatory response, ulcerative and degenerative changes leading to protein-losing enteropathy.
Modes of infection:
Internal autoinfection commonly leads to hyper-infection (massive number of adult worms).
Ingestion of undercooked fish containing larvae.
Infective stage: Larvae in fish.
RH: Fish and birds.
IH: Fish.
Diagnostic stage: Eggs, larvae, and adults in stools.
Habitat: Burrowing in the mucosa of the small intestine.
Geographical distribution: South Asia and Middle East.
Trichostrongylus colubriformis
Clinical picture (Trichostrongyliasis)
Sanitary disposal of human excreta.
Proper water purification.
Proper washing of raw vegetables.
Treatment: - Levamisole is the drug of choice in a single oral dose of 2.5 mg/kg.
Diagnosis: Detection of eggs in stools.
In heavy infection, there is gastrointestinal disturbance and mild anemia.
Asymptomatic in light infection.
Pathogenicity
Anterior end of the worm is embedded in intestinal mucosa causing inflammation which results in gastrointestinal disturbance.
Mode of infection: Ingestion of filariform larvae in contaminated raw vegetables.
Infective stage: Third stage filariform larva. It is sheathed, has a filariform esophagus, and its tail is pointed.
RH: Herbivorous animals.
Diagnostic stage: Trichostrongylus egg.
Geographical distribution: Egypt, Central Africa, India, Japan, and Indonesia.
- Enterobious vermicularis (Oxyuris, thread worm, pinworm, seat-worm)
Food and drink must be protected from contamination.
Infected children must wear tight trouser at night.
Boiling bed linen and cloths.
Avoid thumb suckling and finger nail biting.
Keeping nails short.
Washing hands before meal.
Mass treatment to all members of the family.
Local application of Mercurial ointment (white precipitate ointment) to perianal skin at night to relieve itching, kill adult females and prevent egg deposition.
Albendazole (zentol) is the drug of choice as a single dose of 400 mg/kg and repeated after two weeks.
All the family must be treated.
Detection of adult at the perianal skin at night.
Detection of eggs in stools: + ve in 5% only.
Detection of eggs at the perianal skin in the morning, before bathing and defecation by:
Camel hairbrush of Khalil.
Toilet paper.
Scotch adhesive tape.
National Institute of Health (NIH) swab.
Complications:
Vaginits with mucoid vaginal discharge.
Vulvitis with pruritis vulvae.
Secondary bacterial dermatitis of perianal region.
General symptoms: - Insomnia, restlessness, and nocturnal enuresis.
Local symptoms:
Appendicitis
Enterocolitis (inflammation of mucosa) as the adult attaches itself to intestinal mucosa causing minute ulcerations in caecal and appendicular mucosa, hemorrhage with submucosal abscess due to secondary bacterial infection. There is nausea, vomiting, and diarrhea.
Pruritis ani at night (migration of gravid female out of the anus to lay eggs in perianal skin). Itching causes excoriation of the skin and secondary infection.
May be asymptomatic
Mode of infection: Household transmission is common:
Retro infection: eggs hatch in the perianal region, and the newly hatched larvae ascend through the anus to the large intestine.
Airborne through inhalation of dust contaminated with eggs.
Handling contaminated cloths (night cloths) or bed linen as the eggs remain viable for three weeks.
Ingestion of food and drink contaminated with eggs
Auto infection e.g., during finger biting or thumb suckling.
Infective stage: Embryonated egg (Egg containing larva).
Diagnostic stage: Mature egg (containing larva) and adult female in perianal skin or stools.
Habitat: Caecum and colon (large intestine).
DH: Man, common in children (5-14 years).
Geographical distribution: Worldwide. Mostly in children.
- Trichuris trichiura (Trichocephalus trichiuris or whipworm)
Proper disposal of human feces.
Avoid the use of human excreta as fertilizer to vegetables.
Personal hygiene:
Proper washing of raw vegetables.
Washing hands before meals.
Treatment: • Mebendazole (ivermox or antiver) is the drug of choice in a single oral dose of 100 mg.
Diagnosis:
N.B. Tricuris suis is a parasite of pig. Man dealing with pigs can be infected. Egg pass in human stool without any symptoms giving a false diagnosis of Trichuris trichiuria.
Proctoscopyمنظار لمنطقة المستقيم to detect the worms.
Detection of typical eggs in stools sample.
Heavy infection:
Megaloblastic (hyperchromic) anemia may occur (Trichocephalus pernicious anemia) due to toxins of the parasite.
Bleeding from friable mucosa leads to hypochromic iron deficiency anemia with clubbing of fingers and growth retardation in children.
Penetration of mucosa may predispose to 2ry bacterial infection, appendicitis, and peritonitis.
Dysentery with mucopurulent stools, pain in the right iliac fossa and paraumbilical region frequently lead to rectal prolapse.
Mild infection: Asymptomatic.
Mode of infection: Ingestion of soil, food or drinks contaminated with embryonated egg.
Infective stage: Embryonated egg with 2nd stage larva.
Reservoir hosts (RH): None.
Diagnostic stage: one cell immature egg in feces.
Habitat: Large intestine (caecum, appendix, colon, and rectum) with anterior end embedded in the intestinal wall
Definitive host (DH): Man
Geographical distribution: Worldwide, especially in humid tropical and subtropical countries including Egypt.
- Ascaris lumbricoides (Giant intestinal roundworm)
Treatment of patients.
Avoid the use of human excreta as fertilizer for vegetables
Avoid playing in the soil.
Vegetable washing.
Hand washing.
Treatment is to be followed by purge to avoid allergic manifestation.
Mebendazole (vermox or antiver) is the drug of choice as 100 mg bid (twice daily) for three days. It acts on adult only.
Indirect methods:
X-ray with Barium meal: filling defects (string sign).
Chest x-ray (lung infiltration).
Eosinophilia
Direct methods:
Detection of larvae and Charcot leyen crystals in sputum.
Egg count by Stoll’s technique is needed to estimate worm burden.
Detection of eggs or adults in feces.
The erratic movement of the adult:
Adult migrates from typical habitat through any opening and can even perforate the intestinal wall to:
Biliary ducts: biliary ascariasis with recurrent cholangitis.
Liver: granulomas around eggs and adult ♀.
Peritoneum: peritonitis due to intestinal bacteria after perforation of the intestinal wall.
Appendix: acute appendicitis.
Common Biliary Duct (CBD): obstructive jaundice.
Ampulla of Vater: acute pancreatitis.
occurs due to its irritation by
drugs
anesthesia
Intestinal stage:
Intestinal obstruction due to intussusception and volvulus may occur.
Heavy infection: nausea, vomiting, diarrhea, and abdominal pain. The adult worm metabolites cause gastrointestinal irritation and suppression of digestive enzymes.
Asymptomatic in light infection.
Migratory phase: It is caused by the passage of migrating larvae either to the lung or other viscera.
Loffler’s syndrome:
fever
eosinophilia
Occasionally, some larvae reach the general circulation and are distributed to various organs such as lymph nodes, brain, spleen & kidneys, leading to granuloma formation around the larvae with abnormal clinical manifestations resulting from visceral larva migrans (VLM).
lung infiltration (during prepatent period)
cough
cellular infiltrate with polymorphonuclear cells and eosinophils, cellular exudates and formation of Charcot leyden crystals.
Passing larvae from pulmonary capillaries to the alveoli leads to peticheal haemorrhage,
Life cycle and transmission:
Between 2 and 3 months are required from ingestion of the infective eggs to oviposition by the adult female. Adult worms can live for 1 to 2 years.
In soil, fertilized eggs embryonate optimally in moist, warm, shaded soil and develop infective larva in 2 – 5 weeks
After infective eggs are swallowed,
the larvae hatch,
invade the intestinal mucosa
and are carried via the portal, then systemic circulation
to the lungs.
The larvae mature further in the lungs (10 to 14 days),
penetrate the alveolar walls
ascend the bronchial tree to the throat,
and are swallowed
Upon reaching the small intestine,
they develop into adult worms.
Mode of infection: Ingestion of foods, mainly vegetables and carrots, contaminated by eggs with 2nd stage larvae (embryonated eggs). Contaminated hands with polluted soil are another source of infection.
Infective stage: Egg containing 2nd stage larva (embryonated egg).
Reservoir hosts (RH): None; human is the only host.
Intermediate host (IH): None.
Diagnostic stage: Fertilized and unfertilized immature eggs pass in the feces (200,000 eggs/female/day).
- Habitat: Lumen of the small intestine.
Definitive host (DH): Man, especially children
Geographical distribution: cosmopolitan, especially in tropical and subtropical countries (moist warm climates and temperate zones) with inadequate sanitation. It’s common in Egypt.
- Intestinal cestodes
Diphyllobothrium latum (Broad fish tapeworm)
Sanitary disposal of sewage.
Avoid fishing from heavily infected lakes.
Good fish cooking (temperature above 56°C) or freezing at -18°C for 24 hours kills the plerocercoid stage inside fish.
Vitamin B12 supplements improve anemia and neurological manifestations.
Praziquantel is the drug of choice in a single oral dose of 10 mg/kg BW.
Diagnosis:
Diphyllobothrium anemia: macrocytic = hyperchromic = megaloblastic. It should be differentiated from pernicious anemia where vitamin B12 level is normal while free HCl in gastric juice is absent (achlorhydria).
Detection of eggs in stools by direct or concentration methods (sedimentation by formol ether).
Nervous manifestations as numbness of extremities and disturbance of movements and coordination due to vitamin B12 deficiency.
Diphyllobothrium anemia: The worm consumes 80%-100% of the host's vitamin B12 leading to anemia (macrocytic = hyperchromic = megaloblastic). Pallor, dyspnea, easy fatigability, and tachycardia are common symptoms.
Gastrointestinal symptoms as hunger pains, diarrhea or vomiting.
Cases may be asymptomatic.
Following ingestion of cyclop by Salmon fish (2nd IH), the procercoid larvae migrate into the fish muscles where they develop into plerocercoid larvae (sparganum).
N.B. After ingestion by the cyclops (1st IH), the coracidia develop into procercoid larvae.
Ingestion of raw or imperfectly cooked infected fish containing viable plerocercoid larvae.
Infective stage: Plerocercoid larva.
IH: Two intermediate hosts: 1st IH : Cyclops. 2nd IH: Salmon fish.
RH: Fish-eating animals (e.g., dogs, cats, sea lions, bears).
Geographical distribution: Commonly found in Scandinavia, Russia, Japan, Australia, the great lakes of Canada, and Alaska.
Dipylidium caninum (Dog tapeworm)
Flea control measures.
Treatment of infected household pets.
Treatment: - Praziquantel in a single oral dose of 10 mg/kg BW.
Detection of gravid segments in stools samples.
Detection of egg capsules in stools samples, each containing 8 – 25 eggs.
Clinical Picture
As no more than one parasite can infect man, slight abdominal discomfort and toxic nervous manifestations can be present.
The worms affect mainly children that may suffer abdominal pain.
Mode of infection: - Ingestion of cereals contaminated with insects containing the cysticercoid. - Accidental swallowing of the infected fleas.
Infective stage: Cysticercoid (cystic larva) inside dog and cat fleas.
RH: Dogs and cats.
IH: Dog and cat fleas. Their larvae ingest the eggs passed in the feces. The eggs release onchospheres that develop into cysticercoids in the adults' body cavity (haemocele).
Diagnostic stage: Eggs in feces within egg capsules.
RH: Dogs and cats.
Geographical Distribution: Common parasite of dogs, cats. Accidental in humans especially children.
Hymenolepis diminuta (Rat tapeworm)
Anti-rat and mice measures (rodent control).
Protection of cereals and food from insects (rat flea or beetles).
Treatment: - Praziquantel is the drug of choice in a single oral dose of 5-10 mg/kg BW.
Diagnosis: - Detection of the characteristic eggs in stools samples.
Clinical picture (as H. nana)
The disease affects mainly children and may suffer abdominal pain, diarrhea, insomnia, and convulsions.
Mode of infection: Ingestion of cereals, dried fruits contaminated with insects harboring the cysticercoid.
Infective stage: The cystic larva (cysticercoid).
RH: Rats and mice..
IH: Rat fleas, grain beetles, and cockroaches.
Geographical distribution: Common parasite of rats allover the world. Human is occasionally infected.
Hymenolepis nana (Dwarf tapeworm)
Rodents control.
Treatment of infected persons.
Personal hygiene.
N.B. Precautions during treatment:
Repeated stools examination after one month from treatment to assure complete cure.
Strict hygienic measures must be applied to patients to guard against autoinfection.
All members of the family must be treated simultaneously.
Praziquantel is the drug of choice in a single oral dose of 25 mg/kg BW. It is lethal to both the adult worm and the cysticercoid stage present in the submucosa.
Moderate eosinophilia (8-10%
By detection of eggs in stools sample.
Nervous symptoms such as insomnia, convulsions, or epileptiform fits can occur due to the toxic products of the worm.
Heavy infection may cause some ulceration of the mucosa resulting in abdominal pain and diarrhea.
Mild enteritis and allergy to the worm excretion.
Mode of infection:
Autoinfection, external or internal.
Swallowing of infected insects or their larvae containing cysticercoid. N.B. When eggs are ingested (in contaminated food or water or from hands contaminated with feces), the oncospheres (hexacanth larvae) contained in the eggs are released. The oncospheres penetrate the intestinal villus and develop into cysticercoid larvae. Upon rupture of the villus, the cysticercoids return to the intestinal lumen, evaginate their scolices, attach to the intestinal mucosa and develop into adults that reside in the ileal portion of the small intestine producing gravid proglottids.
Ingestion of foods and drinks contaminated with egg.
Infective stage: Mature eggs and cercocystic cysticercoid.
RH: Rodents (rats and mice).
When fleas larvae ingest the egg, fleas act as intermediate hosts, and cysticercoids develop within their body cavity.
IH: Man acts as an intermediate host because the larva (cysticercoid) develops in the villi of the intestines.
Diagnostic stage: Mature egg.
Habitat: Small intestine.
Geographical distribution: Cosmopolitan, more common in warm climate. It is the commonest tapeworm in children.
Order: Cyclophyllidea Intestinal taeniasis (Taenia saginata and T. solium)
Taenia solium (Pork tapeworm)
Abstaining from using human excreta as manure.
Treatment of infected persons as man is the only source of infection (no reservoir hosts).
Sanitary disposal of human excreta.
Meat inspection at slaughterhouses.
To kill cysticerci, properly cook beef/pork meat or freeze at -10 °c for 5-10 days.
Treatment: - Praziquantel in a single oral dose of 10 mg/kg. Follow up by repeated stool examination for two months after treatment to ensure complete expulsion of the worm.
Diagnosis of intestinal taeniasis:
Detection of coproantigen can differentiate between T. solium and T. saginata using capture ELISA technique.
Detection of gravid segments in stools and differentiate T. saginata from T. solium by compressing the segments between two slides and counting the main lateral uterine branches. Injection of India ink in the common genital pore can help this identification
Detection of Taenia eggs in stools by direct and concentration methods. N.B. Eggs of T. solium cannot be differentiated from those of T. saginata morphologically, but they do not take the Zeihl-Neelsen stain (acid fast).
Cysticercosis: - Man ingests egg of T. solium, that develops cysticercus cellulosa in the extraintestinal tissues. N.B. The egg of T. saginata is not infective to man. In contrast, the egg of T. solium is infective to man causing cysticercosis (infection of human tissue by cysticercus cellulosa the larval stages of T. solium). Thus, autoinfection occurs in T. solium (causing tissue cysticercosis and not intestinal taeniasis) and doesn’t occur in T. saginata.
Taeniasis solium: - Man ingests cysticercus cellulosa in pig's muscles, and the adult parasite develops. The disease is similar to taeniasis saginata.
Mode of infection: Eating pig meat containing viable cysticerci.
Infective stage: Cysticercus cellulosa in pig muscle.
RH: No.
IH: Pig.
Diagnostic stage: Taenia egg and/or gravid segment of Taenia solium in stools.
Geographical distribution: Cosmopolitan (all over the world) specially in pork eating countries. Thus, it is infrequent in Islamic countries.
Taenia saginata (Beef tapeworm)
Segments of T. saginata migrating out of the anus, cause irritation, itching, insomnia, and anxiety.
Intestinal obstruction.
Symptoms of gastrointestinal disturbance such as nausea, epigastric pain, colic, diarrhea, loss of appetite and hunger pain.
Infection may be asymptomatic.
Life cycle and transmission:
Mode of infection: Ingestion of infected beef containing viable cysticerci.
Infective stage: Cysticercus bovis in cattle muscle.
IH: Cattle.
Diagnostic stage:
Gravid segment of Taenia saginata in the stools or creeping around the anus.
Egg of Taenia in the stools.
Habitat: Small intestine of man.
Geographical distribution: Cosmopolitan, especially where beef is commonly eaten.
Nourishment of cestodes:
As they live freely in their adult stage in the small intestine of their definitive hosts attached to the mucosa by their suckers or bothria, already digested nutrients diffuse to the parasite tissues through the cuticle.
The body is divided into scolex, neck, and several segments (proglottids).
The segments (proglottids, strobila) are differentiated into immature, mature, and gravid (full of eggs) segments (according to the degree of maturity of the genital organs).
The neck is the region of growth comprising of actively dividing cells.
The scolex is provided with organs for attachment (fixation) in the form of grooves or suckers.
Members of Cestoda are characterized by being flattened dorsoventrally, ribbon or tape-like, segmented worms, devoid of body cavity or alimentary canal, and are hermaphrodite.
- trematode
Subtypes
- pulmonary fluke
- paragonimus wetermanni
- blood fluke
Blood flukes Schistosoma spp. Intestinal schistosomiasis
Stage of tissue proliferation, repair, and fibrosis:
Snail control measures:
Chemical control: using moullusicides like copper sulphate, sodium pentacholrophenate, and baylucide ”BAYER 73”.
Biological control: using fish and ducks for small canals.
Physical control: by covering canals.
Improving the sewage and drainage systems.
Sanitary disposal of human feces.
Mass treatment of all infected patients.
Health education programs.
Avoidance of contact with polluted water.
Surgical interference in portal hypertension. N.B. Stools examination should be done after three months of treatment for Schistosoma. The viability test should be done to decide whether the patient is cured or not.
Mirazid is an Egyptian oral drug used for treatment with promising efficacy.
Oxamniquine (vansil) is effective against S. mansoni in a single oral dose of 15 mg/kg
Praziquantel (biltricide or distocide) is the drug of choice for all Schistosoma species in a single oral dose of 40 mg/kg.
Indirect diagnosis:
Radiological diagnosis using plain X ray, ultrasonography, CT and MRI. Portal venography may be used for hepato-splenic schistosomiasis with portal hypertension.
Antigen detection is the most accurate method for serological diagnosis of schistosomiasis. The antigen level is correlated with clinical status, worm burden, and peri-portal fibrosis.
Antibody detection can be helpful in both clinical management (e.g., recent infections) and epidemiologic surveys. It indicates schistosome infection in patients who have traveled in schistosomiasis endemic areas and in whom eggs cannot be demonstrated in fecal or urine specimens. The presence of antibodies indicates only schistosome infection at some time and cannot be correlated with clinical status, worm burden, egg production, or prognosis.
Immunodiagnosis using serological tests for detection of antigen or antibody or both. Intradermal, complement fixation, IHA, indirect fluorescent antibody (IFA) tests, and ELISA are used for antibody detection. ELISA is used to detect circulating schistosomal antigens.
Direct diagnosis:
Sigmoidoscopy and rectal biopsy to visualize the mucosa of sigmoid colon for pathological lesions and Schistosoma eggs. It’s essential in chronic cases as fibrosis prevents the passage of eggs to the outside, so stools examination in these cases is negative despite the presence of infection.
Rectal swab using a gloved finger lubricated with soap to palpate the pathological lesion in the rectum and the fecal sample are then examined on a slide for Schistosoma mansoni eggs.
Stools examination detects the characteristic lateral spined eggs using direct smear, especially in heavy infection. Since eggs may be passed intermittently or in small amounts, their detection is enhanced by repeated examinations or concentration procedures (formol ether sedimentation). The egg output can be quantified using the Kato-Katz technique for field surveys and investigational purposes.
N.B. Eggs should be examined for viability by the hatching test to differentiate between living and dead eggs. Freshwater is added to the urine sediment and looked after 30 minutes by a hand lens to demonstrate swimming miracidia.
Dead egg
Does not hatch in freshwater (Negative hatching test)
No RBCs
Dead miracidium (not motile or silent)
Opaque
Living egg
Hatches in freshwater (Positive hatching test)
Surrounded by RBCs.
Intact moving miracidium Contracting and relaxing.
Translucent
History and clinical presentation: History of swimming in polluted water in endemic areas.
Renal involvement occurs due to the precipitation of immune complexes in the glomerular vascular bed leading to glomerulonephritis and end-stage renal failure.
Cardio-pulmonary Schistosomiasis (Bilharzial cor pulmonale): Portal hypertension allows some eggs to pass through collateral veins to the lungs, leading to pulmonary hypertension, right ventricular hypertrophy, and right-sided heart failure (bilharzial cor pulmonale). It presents with dyspnea, fatigue, and cough with hemoptysis.
Central nervous system involvement: due to granuloma formation around eggs embolised to CNS. S. mansoni generally causes spinal cord affection leading to transverse myelitis with flaccid paraplegia. In contrast, brain affection is usually caused by S. japonicum, leading to headache, poor vision, epileptic fits with paresthesia.
Embolic lesions: Female S. mansoni produces about 300 eggs/day. 50% are swept by blood and reach the liver. They block the pre-sinusoidal capillaries and the soluble egg antigen (SEA) elicits T-cell dependent granulomas around each egg leading to Symmers’ pipe stem periportal fibrosis and portal hypertension resulting in marked enlargement of the spleen (Egyptian splenomegaly), hemolytic anemia, ascites and bleeding esophageal varices. Hematemesis (vomiting of blood due to ruptured esophageal varices) and melena (black tarry stools due to digestion of blood after ruptured esophageal varices) are common.
Chronic (late) schistosomiasis:
It’s caused by granulomas (aggregation of inflammatory cells around the eggs trapped in the wall of the intestine) and fibrosis of S. mansoni and S. japonicum leading to the formation of sandy patches, nodules, and papillomata (colonic polyposis) with tissue damage (erosion of the submucosa and the villous tissue), and hemorrhage. The wall becomes thickened, fibrotic, and complicated with strictures, sinuses, fistulae, and prolapse. The patient presents with abdominal pain, dysentery with the passage of blood and mucous in the stools, and hepatomegaly.
Stage of egg deposition and extrusion:
Acute (early) schistosomiasis (Katayama fever): It’s an immune reaction that occurs due to the active deposition (release) of a large number of eggs in the pelvic colon and rectum, leading to inflammation of the submucosa and the villous tissue. It usually occurs weeks after the initial infection. The patient suffers from fever, cough, abdominal pain, diarrhea, hepatosplenomegaly, and eosinophilia.
Stage of migration:
It occurs due to circulating schistosomules.
Metabolic products of maturing parasites: toxic and allergic manifestations e.g. urticaria, fever, headache, cough, wheezes, muscle pain, leucocytosis, and eosinophilia.
Liver and spleen: Hepatosplenomegaly.
Lungs: Verminous pneumonitis (small patches of inflammation) and hemorrhage, with cough, sputum, and hemoptysis (coughing of blood).
Stage of invasion: • Cercarial dermatitis (swimmer’s itch) (bather's itch): Local dermatitis due to skin penetration by cercariae of non-human schistosomes. It usually appears within a few hours and disappears in 7-10 days. It presents with erythema, macule, papule, and itching.
Immune response
Many eggs laid by schistosomes are carried in the blood to the liver where they lodge, leaking antigens and initiating a cell-mediated, delayed-type hypersensitivity reaction. The formation of granulomas around the eggs eventually slows down blood flow through the liver, causing fibrosis and portal hypertension. The disease itself is considered an immune response disease as the body defense mechanism (granulomas) is the disease itself.
During the course of infection, some protective immunity to super-infection is elicited, either by repeated exposures to the cercariae or by the presence of the adults, (although the adult worms themselves are not affected by the immune response). This type of immunity is called concomitant immunity.
Adult schistosomes adsorb host antigens on their surface. The host immune system considers them not foreign and consequently does not recognize the parasite as foreign.
Since the parasites are constantly bathed in blood, we would expect that they are vulnerable to the range of host defense, but they have evolved fascinating mechanisms for evasion.
Mode of infection: Skin penetration by furcocercous cercaria during swimming, walking, or coming in contact with polluted water for some time. Drinking water may be a source of infection if the cercaria penetrates the buccal mucosa of the mouth.
N.B.
Upon release from the snail
the infective cercariae swim
penetrate the human host's skin, and shed their forked tail,becoming schistosomulae
The schistosomulae migrate and enter the venous circulation to reach the right side of the heart, lung, and left side of the heart to reach the systemic circulation
They mature to adults in the portal vein.
The male carries female against blood stream going to its final destination.
The females deposit eggs in the small venules of the portal systems.
The eggs are moved progressively toward the lumen of the intestine (S. mansoni and S. japonicum), and are eliminated with feces.
Infective stage: Furcocercous (bifid tail) cercaria.
IH:
N.B. The stages in the snail include two generations of sporocysts and the production of cercariae.
Onchomelania hupensis snail for S. japonicum.
Biomphalaria alexanderina snail for S. mansoni
Diagnostic stage: Egg in stools.
Habitat: adult worms in humans reside in the radicals of the mesenteric venules in various locations. S. mansoni occurs in the inferior mesenteric veins draining the large intestine, while S. japonicum is found in the superior mesenteric veins draining the small intestine. However, both species can occupy either location, and they can move between sites.
RH: Monkeys and rodents for S. mansoni; and domestic animals (dogs, cats, rodents, pigs, horses, and goats) for S. japonicum.
Geographical distribution: S. mansoni is found mainly in Nile Delta, the Middle East, Africa, and South America, while S. japonicum is principally found in the Far East.
- schistosoma japonicum
- schistosoma mansoni
- schistosma haematobium
- intestinal fluke
- fasciolopsis buski
- heterophyes heterophyes
Sanitary disposal of human feces interrupts disease transmission from feces to snails.
Health education for proper salting and grilling of fish. Avoid eating raw, insufficiently cooked fish or under-salted fish, salted less than ten days (sweet fessekh). Fried fish is safe as the temperature needed for frying is high enough to kill metacercariae.
Periodic examination and mass treatment of fishermen, the main source of infection to the snail intermediate host.
Treatment: • Praziquantel is the drug of choice in a dose of 10-20mg/kg.
Immunodiagnostic tests for antibody detection using ELISA and Immunoblot tests.
Direct stools examination for detection of eggs. The egg output is usually low, especially in light infection, which is easily missed. So, concentration methods give good results.
Extra-intestinal manifestations: The eggs may reach the general circulation to different organs and form parasitic granuloma and fibrosis. Migrating eggs to the heart can cause heterophyid myocarditis, dyspnoea, cyanosis, palpitation with abnormal heart sound. Eggs in the brain may cause neurological manifestations. Eggs in the lungs cause miliary nodular shadows, mistaken for tuberculosis (TB).
Heavy infection: Colicky mucoid diarrhea due to attachment of the parasite to the mucosal membranes leading to inflammation with superficial ulcers and necrosis.
Light infection may pass unnoticed.
It depends on the intensity of the infection:
Mode of infection: Man gets infection by ingesting encysted metacercaria in raw or undercooked or lightly salted (sweet fesekh) fish.
Infective stage: Encysted metacercaria in-between fish muscles (2nd IH).
IH
2nd IH: Freshwater fish; Bolty (Tilapia nilotica) and Bory (Mugil cephalus).
1st IH: Pirenella conica snail.
Diagnostic stage: Egg (containing mature miracidium) in stools.
Habitat: Small intestine (jejunum and ileum) deeply embedded in-between intestinal villi. The deeply embedded eggs and sometimes adults may enter the nearby lymphatic and blood vessels to be transported like emboli to other ectopic sites, mainly heart, lungs, liver, spleen, or brain.
RH: Cats, dogs, and other fish-eating animals.
DH: Man.
Geographical distribution: Common in Egypt in Nile Delta, especially around the lakes of Manzala and Borollos, Middle East (Turkey) and Far East (Japan, China, Korea, Philippine).
- liver fluke
- clonorchis sinensis
Hepatic/Liver Flukes Fasciola hepatica / Fasciola gigantica
Prevention and control:
Health education.
Sanitary disposal of human feces.
Snail control measures.
Proper washing or cooking of aquatic vegetation.
Pure filtered water supply.
Treatment is required to eliminate the long-lived parasite in human and animal reservoir.
Treatment
Surgical removal of ectopic flukes.
Halzoun can be treated by gargling with alcohol or by tracheostomy in severe cases.
Triclabendazole (fasinex, egitan) is the drug of choice for fascioliasis in a single oral dose of 10-20mg/kg.
Biochemical tests like high levels of serum bile acids and liver enzymes, especially alkaline phosphatase, and eosinophilia.
Immunodiagnostic tests by ELISA and indirect hemagglutination test (IHA) using execratory-secretory antigen are sensitive and practical during the migratory stage of the worms and ectopic infection for estimation of specific antibodies. Specific antibodies to Fasciola may be detectable within 2-4 weeks after infection, which is 5-6 weeks before eggs appear in the stools. Their levels decrease to normal 6-12 months after therapeutic cure. This can be used to predict the success of therapy.
Parasitological Diagnosis: Direct microscopic examination of eggs is valuable in the chronic stage. Eggs can be recovered in stools, aspirated duodenal contents, and biliary drainage. To avoid false fascioliasis, the patient should be asked to stop eating liver for a few days before the examination.
Clinical picture
Halzoun: It’s parasitic pharyngitis caused by eating infected raw liver. The worms attach themselves to the pharyngeal mucosa causing edema. This may result in dyspnea and suffocation.
Ectopic fascioliasis causes pulmonary, cardiac, gastric, caecal, cerebral, and neurological disorders.
Liver rot: Mechanical and toxic destruction of liver tissue by passage of large number of immature worms through the liver tissue leading to necrosis, fibrosis, hepatitis, and hepatomegaly. Severe infections can lead to death.
Chronic (obstructive) phase caused by adult flukes within the bile ducts. They begin producing eggs 3-4 months after ingestion of metacercariae. This worm may live around ten years. The patients presents with intermittent biliary obstruction, cholangitis, and cholecystitis leading to irregular fever, biliary colic, abdominal pain, and tender hepatomegaly. This may progress to an obstructive phase leading to jaundice. In children, severe anemia and high eosinophilia are common. Inflammation of the bile ducts leads to fibrosis, a condition called “pipe- stem liver”.
Acute (Invasive) phase due to the migration of the immature fluke through the duodenal wall, into the body cavity, then through Glisson's capsule across hepatic parenchyma reaching to the proximal bile duct. This phase continues for 6-7 weeks, through which the patient suffers from fever, abdominal pain, gastrointestinal disturbances (vomiting and diarrhea), hepatomegaly, anemia, and haemobilia.
Life cycle and transmission:
Mode of infection: Man gets infection by ingesting encysted metacercaria in fresh water plants especially watercress.
N.B. After ingestion, the metacercariae excyst in the duodenum and migrate through the intestinal wall, the peritoneal cavity, and the liver parenchyma into the biliary ducts, where they develop into adults. In humans, maturation from metacercariae into adult flukes takes approximately 3 to 4 months.
Infective stage: Encysted metacercaria on aquatic plants and green vegetation.
IH: Lymnaea truncatula snail for F. hepatica and Lymnaea cailliaudi snail for F.gigantica.
Diagnostic stage: Egg (bile- stained) in stools. N.B. Eggs are discharged with feces of infected host in freshwater of canals, drains, and River Nile, hatch within two weeks into miracidium.
Habitat: Intrahepatic bile duct and pancreatic duct of man, cattle, and sheep. The parasite sometimes has ectopic sites like liver parenchyma, subcutaneous tissue, blood vessels, and the brain.
RH: Sheep for F. hepatica and cattle for F.gigantica
DH: Man.
Geographical distribution: Worldwide, especially in sheep and cattle raising countries, including Egypt, Africa, Asia, and Europe.
All are hermaphrodite except Schistosoma spp.
The body is made up of systems.
They are covered externally by a cuticle that may be smooth, spiny, or tuberculated.
All trematodes possess two suckers (oral and ventral) as attachment organs except H. heterophyes (3rd genital).
Adults are leaf-like, pear-shaped, or elongated worms.
Pathology
Small & Large Intestinal Disorders
Inflammatory Bowel Diseases (I.B.D.)
Classification of inflammatory bowel diseases:
Idiopathic
Ulcerative colitis.
Unknown, may be: • Autoimmune. • Genetic. Infection
Idiopathic, chronic, ulcero-constrictive inflammatory bowel disease characterized by segmental, transmural non-caseating granuloma
Crohn's disease (Regional enteritis).
Gross
It starts in the rectum then extends to involve the whole colon. • The affected mucosa show broad – based ulcers separated by edematous, swollen mucosa → pseudo polyps.
Sex: More common in ♀.
Age: Young adults (20 – 25y).
Unknown, may be: • Autoimmune. • Genetic.
Definition
A recurrent, chronic, ulceroinflammatory disease of large intestine & affecting the mucosa & submucosa
Infectious: e.g. bacterial, mycobacterial, viral, fungal, fungal, protozoa, parasitic & helminthes
Non-infectious: e.g. Ischemia, radiation, uremia, cytotoxic drugs.
Nomenclature
Dysentery: Passage of mucoid bloody diarrhea with tenesmus (pain) (in cases of colitis).
Diarrhea: Change of bowel habits
Colitis: Inflammation of large intestine.
Enteritis: Inflammation of small intestine.
Definition: They are a group of inflammatory disorders affecting small & large intestines & characterized by abdominal pain & diarrhea.
Diseases of the Small Intestine
liver pathology
Liver Tumors
Classification
Secondary (metastasis): More common than primary.
Primary
Classification of primary liver tumors:
Malignant
Mesenchymal: -Angiosarcoma
Cholangiocarcinoma (Bile duct)
Microscopic picture: well differentiated adenocarcinoma composed of irregular and tubular structures lined by malignant cuboidal epithelium within abundant fibrous stroma (desmoplastic reaction). Bile pigment in the cytoplasm and Mallory bodies aren't found in the cells
Goss picture: firm, grayish white mass
Definition: carcinoma of the biliary tree arise from the bile duct epithelium
Hepatocellular Carcinoma (HCC) & Hepatoblastoma (Hepatocytes)
Hepatoblastoma
Microscopic picture: Contains mixture of immature hepatocytes with stroma showing mesenchymal differentiation (bone, cartilage, etc.). It associated with elevated serum level of AFP.
Goss picture: Large mass with extensive hemorrhage & necrosis.
Origin: Arises from multi-potential blastema that differentiate into epithelial & mesenchymal components
Incidence: Rare malignant tumor of infancy and childhood.
Hepatocellular Carcinoma (HCC)
Diagnosis
High level of alpha-fetoprotein (above 1000 I.U).
Liver biopsy is required.
Inferior vena cava obstruction causing edema of lower limbs.
Portal vein thrombosis
Hepatic failure and jaundice.
Enlarged, nodular liver.
Spread of HCC:
Blood spread:Through hepatic veins to Rt. side of the heart & lungs.
Lymphatic spread: To lymph nodes of porta hepatis.
Direct spread: To surroundings e.g. the ribs.
Intra-hepatic spread: Within the liver, by branches of portal vein
Fibrolamellar variant of HCC:
Miroscopic picture: large polygonal malignant cells separated by fibrous tissue.
Incidence: uncommon <5%, occur in children and young adults, no association with cirrhosis or viral hepatitis and has better prognosis.
Bile pigment in the cytoplasm and Mallory bodies may be found.
Poorly differentiated tumors: Consist of undifferentiated cells, spindle cells or large anaplastic cells and multinucleated giant cells.
Well differentiated tumors: Consist of polyhedral malignant epithelial cells forming cord, groups or acini (pseudo-glandular pattern) separated by little stroma.
Gross picture: The tumor mass is either:
Diffuse infiltrative tumor that may involve the entire liver. Soft consistency, yellow white, sometimes bile stained with areas of hemorrhage and necrosis.
Multi-focal with widely distributed nodules.
Unifocal, usually massive tumor.
Predisposing factors:
Contaminated food with Aflatoxin (Aspergillus flavus toxin).
Alcoholic liver disease
Chronic hepatitis: e.g. HBV & HCV.
Cirrhosis: post-necrotic or pigmented cirrhosis.
Incidence
It is common in males (40- 60 Y) than females.
It constitutes 90% of primary liver cancers
Benign
Mesenchymal: - Cavernous hemangioma
Epithelial
Bile duct adenoma (Bile duct)
Hepatic adenoma (Hepatocytes)
Cirrhosis
Clinical features:
Portal hypertension
Progressive liver failure
Portal tract: expanded by fibrosis, infiltrated by chronic inflammatory cells and show proliferating bile ducts.
Regenerating nodules: regenerating hepatocytes become surrounded by bridging fibrous bands to form nodules, central vein appear eccentric or absent.
Liver cells: degeneration and necrosis of hepatocytes
Loss of normal liver architecture
The color of regenerating nodules is green in biliary cirrhosis, dark brown in hemochromatosis and pale in alcoholic cirrhosis.
Cut section:Variable sized nodules, separated by whitish fibrous bands with variable thickness (Thin in micro-nodular & thick in macro-nodular cirrhosis).
Outer surface: Irregular and nodular.
Consistency: Firm consistency with sharp borders.
Size and weight: Decreased.
Pathogenesis of cirrhosis:
In cirrhosis, Type I and III collagen are deposited in all portions of the lobules and in the space of Disse, and the sinusoidal endothelial cells loose their fenestrations which impair the exchange of the solutes (albumin, lipoproteins, clotting factors) with the blood. The sinusoids are converted to high pressure vascular channels which contribute to the development of portal hypertension.
Ito cells, when activated by cytokines are transformed into myo-fibroblasts (collagen-forming cells) producing excess collagen and extracellular matrix.
The major source of excess collagen in cirrhosis is perisinusoidal Stellate cells (Ito cells) which are located in space of Disse and function as vitamin A and fat storage cells.
The process is initiated by hepatic injury that stimulates the release of cytokines (TGF-β, IL-1 and TNF) from damaged hepatocytes and sinusoidal endothelial cells.
Classifications of cirrhosis:
Morphological classification
According to the size of the regenerating nodules.
Mixed: Contains mixed micro and macronodular patterns.
Macronodular: The nodules are larger in size, ranging from 2-3 mm. It is seen in post-hepatitic and post-necrotic cirrhosis.
Micronodular: The size of the regenerating nodules ranges from 1-2 mm. in diameter. It is usually seen in alcholic and biliary cirrhosis.
Etiological classification
According to the cause into:
Secondary cirrhosis:
Syphilytic cirrhosis
Cirrhosis on top of metabolic disorders:
α1 antitrypsin deficiency.
Wilson’s Disease.
Hemochromatosis (Bronzed diabetes).
Cardiac cirrhosis: e.g., CVC liver
Biliary cirrhosis:
Secondary biliary cirrhosis.
Complications of cirrhosis:
Hepatocellular carcinoma (HCC
Ascites
Liver cell failure.
Portal hypertension.
Clinically: itching (due to bile salts retention), jaundice and hyperlipidemia, dark urine, light stool
Microscopic picture:
Progressive fibrosis with development of micro-nodular cirrhosis.
Cholangitis with neutrophilic infiltration around bile ducts
Proliferation, dilatation and rupture of bile ductules in portal areas
Bile stasis causes degeneration & focal areas of hepatocyte necrosis.
Extra-hepatic bile ducts cholestasis.
Gross picture: as primary biliary cirrhosis.
Causes: Extra-hepatic biliary obstruction by:
Congenital stenosis or fibrosis of bile duct.
Gall stone impacted in common bile duct.
Cancer of common bile duct or ampulla of Vater.
Cancer head of pancreas.
Choledochal cyst.
Primary biliary cirrhosis.
Portal hypertension.
Malabsorption
Obstructive jaundice
Clinical manifestations: Fatigue, itching (due to bile salts retention), jaundice and hyperlipidemia, dark urine, light stool
Microscopic picture:
Unrelieved obstruction leads to portal tract fibrosis that extends to and divide the parenchyma into nodules forming micro-nodular cirrhosis.
Distension of bile canaliculi with bile plugs. In portal tracts: obstruction of bile ducts causes bile stasis and backpressure that induce proliferation of bile ductules and portal inflammation.
Hepatocytes show accumulation of bile pigments (cholestasis) causing foamy degeneration and necrosis especially in the periportal hepatocytes.
Early: Chronic granulomatous inflammation, surrounding bile ducts destroying them.
Gross picture:
Shape: Micro-nodular.
Color: Dark green (bile stasis).
The liver size: Decreased
Pathogenesis
Destroyed intra-hepatic bile ducts interrupt the normal bile flow leading to retention of toxic substances in bile (bile acids and Copper) that causing further secondary destruction of bile ducts and hepatocytes. Fibrosis extends into lobules leading to further obstruction of bile flow and form micro-nodules and subsequent micro-nodular cirrhosis.
An autoimmune, progressive, cholestatic disorder characterized by granulomatous destruction of intra-hepatic bile ducts, portal inflammation and scarring with development of cirrhosis. It is mediated by activated CD4 & CD8 lymphocytes.
Cause: Intra-hepatic biliary obstruction. It commonly affects middle aged women (Female: Male = 9: 1).
Viral hepatitis.
Alcoholic cirrhosis.
Peri-central fibrosis that leads to obliteration of the central veins as well as formation of fibrous bridges followed by alcoholic cirrhosis.
Hepatocyte necrosis and recruitment of neutrophils.
Hepatocytes degeneration: Ballooning degeneration, steatosis and Mallory bodies.
Gross picture:
Cut section & outer surface: Micro-nodular cirrhosis.
Color: Yellowish.
Liver size: Shrunken.
Pathogenesis: toxic metabolites of ethanol and O2 free radicals cause hepatocyte injury and leads to steatosis and hepatocyte injury.
Causes: chronic ethanol consumption.
Primary (cryptogenic) cirrhosis.
Definition: Chronic, diffuse, progressive, and irreversible liver disease, characterized by:
Loss of normal liver architecture
Bridging fibrous septa that encircle the regenerating hepatocytes form nodules.
Repair by regeneration.
Degeneration and necrosis of hepatocytes.
Cirrhosis: end stage of chronic liver disease.
Hepatic Injury
Liver cell death: Any significant hepatic injury might cause:
Features of liver cell necrosis:
Diffuse and massive necrosis: Associated with collapse of the supporting reticulin framework, so leading to cirrhosis.
Focal and zonal necrosis: No collapse of reticulin framework of necrotic area. The hepatocytes will regenerate, and restoration of normal pattern occurs (2-3 weeks).
Types: Classified, according to the extent & distribution of necrosis into:
Massive hepatic necrosis (Fulminant hepatitis):
Effects
Post-necrotic cirrhosis
Death (within days).
Microscopic picture:
The portal tracts show inflammatory cellular infiltration formed mainly of lymphocytes and plasma cells.
The sinusoids are dilated and congested.
Most hepatic lobules reveal massive necrosis. Other lobules show intact peripheral hepatocytes.
Cut section: Yellow color of degenerative areas with red areas of hemorrhage.
Capsule: Wrinkled capsule with sub-capsular hemorrhages.
Consistency: Soft (massive necrosis).
Size & weight: Reduced.
Causes
Malignant infiltration.
Wilson disease and autoimmune hepatitis.
Hepatic vein obstruction
Drugs and chemicals: CCL4, chloroform, halothane, acetaminophen and αmethyldopa.
Infection: fulminant viral hepatitis & Herpsvirus.
Definition: Fulminant hepatitis denotes severe liver function impairment and clinical hepatic insufficiency that progress from onset of symptoms to hepatic encephalopathy within 2-3 weeks.
Diffuse necrosis
Zonal necrosis
Focal necrosis
Coagulative (ischemic) necrosis: involving part of hepatic tissue.
Apoptosis: Shrunken, isolated and eosinophilic hepatocytes with pyknotic nuclei are called “apoptotic bodies, acidophil bodies or councilman bodies”.
Liver cell degeneration and cellular accumulations:
Intracellular accumulation of substances:
Retained bile (cholestasis): e.g., biliary cirrhosis.
Accumulation of iron: e.g., hemochromatosis.
Steatosis: accumulation of fat" (e.g., HCV, Alcoholic hepatitis).
Hydropic degeneration: Accumulation of water in hepatocytes
.
Syllabus
adenocarcinoma
gross
path
CAUDATE LOBE HYPERTROPHY
doesn't atrophy because has a different outflow tract
centrilobular congestion
fibrous occlusion of small hepatic venules
PSC pathology
abnormally shaped liver on gross exam
degeneration of bile duct epithelium with PRESERVATION of basement membrane
onion skin fibrosis
PBC stages
jigsaw liver indicates biliary cirrhosis
stage 1: duct membrane lesion, granulomatous reaction
alpha-1 anti trypsin
immunostain shows presence of alpha-1 antitrypsin
round to oval cytoplasmic inclusions in periportal hepatocytes
on prussian blue, iron is blue
secondary hemochromatosis: ALSO see iron in Kupffer cells and macrophages
periportal iron deposition
heavy in periportal tracts, lighter toward central venule
vascular disorders
shock (ischemic necrosis of CENTRILOBULAR hepatocytes)
CHF (NUTMEG apperance)
veno-occlusive disease
from CHF, sickle cell disease
hepatic radiation
after bone marrow transplant
alkaloid ingestion
budd-chiari syndrome (LIVER OUTFLOW OBSTUCTION)
IBD, MULTIPLE MYELOMA
stasis or mass lesions
vascular injury (trauma, vasculitis
hypercoagulation
biliary tract disease
secondary sclerosing cholangitis
mechanical problem leading to cholangitis and biliary cirrhosis
primary sclerosing cholangitis
SMALL bile ducts
mostly MALE
"onion skin fibrosis"
primary biliary cirrhosis
LARGE bile ducts
pruritis, xanthelasma, osteoporosis
increased GGT and bilirubin
AMA+
middle-aged women
lymphocytic infiltration
destruction of bile duct basement membrane
chronic progressive
immune-mediated attack on pyruvate dehydrogenase of bile duct cells
cystic diseases of liver
benign tumors and tumor-like lesions
angiosarcoma
cholangiocarcinoma
hilar tumor (klatskin)
type of adenocarcinoma
arises from biliary epithelim
HCC
variable histology
NASH predisposes
anabolic steroids can cause
caused by Hep B, C, alcohol, contraceptives
metastatic tumor
focal nodular hyperplasia
hepatic adenoma
associated with ORAL CONTRACEPTIVES
portal tracts or central venules absent, but see arteries and veins traversing tumor
well-encapsulated
solitary
alcoholic liver disease
alcoholic hepatitis
micronodular cirrhosis
fibrosis
neutrophilic reaction
mallory bodies: cytokeratin filaments (not diagnostic)
ballooning degeneration
hepatic steatosis
accumulation of collagen over time that encapsulates hepatocytes
macro- or microvesicular steatosis, but reversible
metabolic liver diseases
alpha-1 anti-trypsin
most common pediatric liver disease
wilson's disease
atrophy of brain tissue and cavitation of basal ganglia
hepatic necrosis
copper in periportal hepatocytes
Keyser-Fleischer ring in iris
variable onset
defective biliary copper excretion
AR
excessive copper accumulation
cystic fibrosis
hereditary hemochromatosis
pathology
200x increased risk of HCC
SKIN PIGMENTATION (bronze skin)
DIABETES MELLITUS (iron deposition in pancreas)
MICRONODULAR CIRRHOSIS
AGE 40, males present before females
homozygous recessive
excessive iron deposition
Gall Stones (Cholelithiasis)
Complications of gallbladder stones:
Biliary colic: Radiating to the right shoulder (through the phrenic nerve).
Obstruction of ampulla of Vater: leading to acute hemorrhagic pancreatitis.
Common bile duct obstruction causes:
Secondary Biliary cirrhosis.
Cholangitis
Obstructive jaundice.
Cystic duct obstruction causes
Empyema
Mucocele
Gall bladder affection:
Squamous metaplasia of the surface epithelium due to chronic irritation predisposes to malignancy
Fistula formation with the duodenum which permit the stone to pass into the intestinal lumen causing acute intestinal obstruction.
Acute or chronic cholecystitis.
Types of gallstones:
Combined stones: pure gallstones nucleus with mixed gall stone shell or mixed gallstone nucleus with pure gall stone shell.
Firm
Mixture of colors C/S: Dark centre surrounded by white shell or vice versa
Irregular , rounded or oval
Single or multiple - large
10%
Mixed stones: combination of Cholesterol, bile pigment stone and calcium carbonate stones.
Mixture of colors- -C/S: Laminated alternating dark pigment layer and pale white layer
Faceted
Always multiple - 1- 2 cm
70-80%
Metabolic (pure) stones: Cholesterol, bile pigment stone and calcium carbonate stones.
Ca carbonate Stone
Hard
Grayish white
Smooth, rounded or oval
multiple -Small
10%
Pigment stone
Soft & friable
Homogenous, Black or green
Mammillated
Multiple small -
3%
Cholesterol stone
Consistency
Soft
Color & Cut section
Pale yellow C/S: Radiating glistening crystals
Surface & shape
Smooth surface, Oval or rounded
Numb.& Size
Solitary -large
Incidence
7%
Hormonal hypo-motility of gallbladder: as in pregnancy.
Bile stasis: Leading to: Infection --> Stone formation --> Stasis (vicious circle).
Inflammation of the gallbladder (cholecystitis)
Inflammation causes shedding of epithelial cells and formation of pus cells which act as nuclei for stone formation.
Inflammation decreases bile salts formation and decrease motility of gall bladder leading to cholesterol precipitation and subsequent stone formation.
Hypercalcemia: Predisposes calcium carbonate stone formation.
Abnormal bile composition (cholesterol & Bile pigment):
Increased bile pigment (bilirubin) in blood and bile in cases of hemolytic anemia.
Increased cholesterol concentration in blood or bile (e.g. pregnancy and increased fat intake or familial). Bile salts become unable to keep cholesterol in solution and some will precipitate.
Sites: Gall bladder & bile ducts.
Incidence: More common in females (2- 5 times as males). The affected Female is usually Fatty, Filthy, Fertile (parous), around the age of Forty (5F).
Diseases of Gall Bladder (Cholecystitis)
Chronic cholecystitis.
Squamous metaplasia predisposes to squamous cell carcinoma.
Formation of gall bladder stone in (80- 90%) of cases.
Recurrent acute attacks on top of chronic cholecystitis.
Wall: Fibrosis and chronic inflammatory cellular infiltrate.
Subepithelial tissue: Infiltrated by chronic inflammatory cells. Marked histiocytic infiltration "Xanthogranulomatous cholecystitis"
The mucosa:
Squamous metaplasia.
Hyperplastic
Flat and ulcerated
Surface: Fibrous adhesions.
Lumen: Either distended with clear bile (hydrops) or mucous (mucocele) or contains stones.
Wall: Thickened, fibrotic with or without calcifications.
Mucosal folds: Extends deep into the wall forming sinuses "Aschoff- Rokitansky sinuses"
Size of gall bladder: According to presence or absence of obstruction:
Obstructed: Large, with absent mucosal folds.
Non-obstructed: Small, fibrotic with exaggerated mucosal folds.
Etiology: either follows recurrent attacks of acute cholecystitis or arise de-novo.
Definition: Chronic inflammation of gallbladder.
Acute cholecystitis.
Complications
Chronicity: Passing to chronic cholecystitis.
Adhesions with the surroundings.
Ascending cholangitis.
Ruptured gall bladder leading to
Liver abscess.
Enteric fistula
Septic peritonitis.
Necrosis and gangrene: Due to ischemia of the distended bladder with superadded saprophytic infection and development of gangrene
Empyema: If the bladder neck is obstructed.
Microscopic picture:
Sub-epithelial tissue: Edematous and infiltrated by neutrophils and contain thinwalled, dilated and congested blood vessels.
Mucosa: Partially ulcerated.
Lumen: Shredded mucous cells, neutrophils and pus cells.
Gross picture:
Lumen: Distended with turbid bile.
The wall: Thick and edematous.
Gall bladder: Swollen with hyperemic surface.
Etiology
Ischemia: due to increased intraluminal pressure that decrease blood flow to mucosa: Inflammation occurs in ischemic areas.
Reflux of pancreatic enzymes.
Bacterial infection: Micro-organisms e.g. E.coli & salmonella typhi reach the gallbladder through blood or common bile duct (ascending cholangitis).
Chemical and mechanical irritation:
The irritation open the way to bacterial infection.
Abnormal concentrated bile due to obstruction of the cystic duct or common bile duct by stone.
Definition: Acute inflammation of the gall bladder.
Definition: Inflammation of gallbladder.
Bio
De novo synthesis of fatty
acids: fatty acid Synthase System
fatty acid synthesis 1
disorders of protein absorbtion
protein digestion
lipid and protein digestion
lipid digestion and absorbtion
Digestion and absorption of carbohydrates
Physiology
Control of food intake
Other Factors:
Cold: can increase food intake
voluntary control &psychological factors: can ↑ food intake or ↓food intake
Factors regulating food intake
Long term regulation • Aim to maintain nutrient store & blood level of nutrient constant
Peptide hormones
Peptides that decreased food intake
POMC (pro-opiomelanocortin)
CART (cocaine-and- amphetamine regulated transcript)
a-Melanocyte-stimulating hormone (a-MSH)
Corticotropin-releasing hormone (CRH)
leptin
Adipose tissue
PYY
Glucagon-like peptide-1 (GLP-1)
Small intestine
CCK
Site of seceretion
Small intestine, neurons
Peptides that increased food intake
Orexins (hypocretins)
Hypothalamus
NPY and Agouti-related protein (AgRP)
hypothalamus
Ghrelin
Source of secretion
lipostatic hypothesis
Leptin: discovered in 1994 (leptos, thin):
NB: majority of obese human have elevated leptin----leptin resistance---abnormal tissue response rather than too little hormone
Leptin acts as a negative feedback signal between adipose tissue brain Neuropeptide y (NPY): brain neurotransmitter-----stimulate food intake-- -Leptin inhibit NPY release----decrease food intake
Protein synthesized in adipocytes under control of ob gene-------provide evidence for a lipostatic theory
↓fat stores ----- ↑ food intake
↑fat stores → ↓food intake
Glucostatic hypothesis:
↑blood glucose level →-stimulate satiety center
↓blood glucose level → stimulate feeding center
Short term regulation
Humoral &hormonal factors: Presence of food in stomach &duodenum release many hormones CCK& GLP1 ➔ inhibit feeding center ➔↓food intake.
Afferent impulses from buccal &esophageal receptors: Certain amounts of food pass through these receptors (chewing and swallowing) ➔ send signals ➔ stimulate satiety center
Afferent impulses from GIT: Distension of stomach& duodenum ➔ vagus➔ Decrease food intake
Hypothalamic centers regulating food intake (Appestat center)
Appestat center:
Satiety center
Its destruction overeating (hyperphagia)
its stimulation decrease food intake by --- feeding center
site: ventromedial hypothalamic nuclei
Feeding center
Its destruction: anorexia
Its stimulation: eating behavior (food intake)
continuously (tonically) active But inhibited by activity of satiety center
site :lateral hypothalamic nuclei
Food intake is controlled by organic sensation
Satiety : (enough) sense of fulfillment in quest of food
Appetite: desire for a specific type of food
Hunger: need for food
Pancreas
Pancreatic secretion
The pancreas has both:
Exocrine gland:
Exocrine pancreatic secretion:
Comparison
Secretin
Increase Ca++
+ ve F.B between CCK and A.A as CCK causes more digestion of protein leading to production of amino acids which lead to restimulation of CCK
↑ Evacuation of bile from gall bladder (cholagogue).
↑ insulin H.
↑ Secretion of enzymes.
↑mucus secretion.
Acidic chime from stomach ↑ HCL pass to the duodenum with decrease its pH.
27 A.A
Cholecystokinin pancreozymi n (CCK)
Second messenger
cAMP
Control
-ve F.B as Hcl causes release of secretin which in turn inhibit HCl secretion from the stomach.
Effect on:
bile
↑Secretion of bile Na HCO3.
pancreas
↑ Insulin hormone.
↑ Secretion of alkaline juice.
Intestine
↑motility & enzymes secretion.
Stomach
Inhibition of gastric functions (motility and secretion).
Stimuli
Fats & F.A. in duodenum
Polypeptides & AA
Digestive products of protein and fat
Site
Upper part of small intestine
Structure
22 A.A
Control of exocrine pancreatic secretion:
Hormonal: Secretin →↑ aqueous alkaline secretion from duct. CCK. PZ →↑ enzymatic secretion from acini.
Nervous: as a part of conditioned & unconditioned reflexes → vagal stimulation of enzymatic secretion from acini.
There are 3 classes of enzymes:
Proteolytic enzymes:
They are secreted in inactive form and activated by enterokinase (in small intestine) and the active trypsin to prevent autodigestion of pancreas (also the pancreas has trypsin inhibitor).
Exopeptidases :Procarboxypeptidases.
Endopeptidases as trypsinogen & chymotrypsinogen.
Pancreatic lipolytic enzymes: Lipase and phospholipase (facilitated by bile).
Phospholipase A: act on lecithin → lysolecithin.
Triglycerides → FFA & monoglycerate.
Pancreatic amylase: starch → maltose.
Enzymatic juice:
Stimulated by cholecystokinin-pancreozymin (CCK – PZ) & vagus nerve.
Secreted by acinar cells.
Small in volume, rich in enzymes.
Mechanism of secretion:
Acid- tide: ↑ H+ concentration in venous blood drain the pancreas to neutralize alkaline tide of gastric secretion → acid – base balance.
H2O diffuses passively into the lumen by osmotic forces of Na+ & HCO3-.
H+ ion is pumped out to the plasma (acid tide) in exchange for sodium which is pumped into the cell then diffuses to lumen.
HCO3- is actively secreted in lumen.
Types
Aqueous alkaline juice:
Stimulated by secretin hormone & inhibited by sympathetic.
Large in volume, rich in bicarbonate & Secreted by duct cells.
Ions
CL- : lower concentration than plasma.
HCO3: higher than in plasma (140 mEq/L).
Na+ & K+: the same concentration of plasma.
Osmolarity: iso-osmotic with plasma.
PH : 7.8 – 8.3
Volume: 1 – 1.5 L/day.
The common opening is surrounded by sphincter of Oddi
consisted of blind secretory acini,ducts which drain in pancreatic duct which unites with common bile duct and open together at the ampulla of Vater in the duodenum
Endocrine gland:
Beta cells → insulin.
Alpha cells → glucagon
Gastric secretions and motility
Gastric secretion
Gastric secretion: is 2.5 – 3 L/day of acidic juice (pH may reach 1).It is secreted from the gastric glands:
Gastric glands:
Control of gastric secretion:
Nervous and hormonal:
Three phases:
Intestinal phase: The presence of food in the duodenum inhibit the gastric secretion
In the duodenum: presence of acid, fats or hyperosmotic solution in the duodenum will inhibit the gastric secretion via:
Hormonal mechanism (Enterogastric hormones):
It is stimulated by the presence of fats and fatty acids → the release of 4 hormones from the duodenum [cholecystokinin (CCK), secretin, gastric inhibitory peptide (GIP) & VIP] → hormonal feed – back inhibition of gastric secretion and motility for complete digestion of fat.
Nervous mechanism (Enterogastric reflex):
The response and the importance:
Prevent rapid electrolyte changes during intestinal absorption.
Insure protein digestion.
Protection of duodenum from hyperacidity (till neutralized by alkaline duodenal secretion).
Protection of duodenum from over distention by increase in the tone of pyloric sphincter → delays the emptying.
Inhibition of gastric secretion and motility
The reflex is conducted in the three ways: local, ganglionic or vago – vagal reflex.
It is stimulated by presence of acid, fats or hyperosmotic solution in the duodenum or distention of the duodenum will inhibit the gastric secretion.
Gastric phase : (70 %): The presence of food in the stomach → increase gastric secretion by mechanical, chemical and neural stimuli as the following:
N.B : hypoglycemia →↑ vagal stimuli →↑ secretion.
Vago-vagal long reflex: food in stomach → afferent vagus to vagal center & efferent vagal increase in gastric secretion so inhibited by atropine.
Local nerve plexus: by distension or polypeptides → stimulate Meissner’s plexus →↑secretion.
Gastrin secretion: by direct stimuli as polypeptides, alcohol and caffeine or via local and vago-vagal reflex to stimulate the vagal center.
Cephalic phase: (25 %):
It is a nervous phase activated by conditioned and unconditioned reflexes:
In the unconditioned reflex: direct contact of food stimulates taste buds which give afferent to the vagal center.
The role of unconditioned reflexes is proved by:
Sham feeding experiment: The esophagus of a dog is exposed and divided in the neck, so the food swallowed will pass to outside. At the same time a gastric fistula is inserted. Although no food reaches the stomach, Sham feeding increases gastric secretion.
In the conditioned reflex: Psychic stimulation of cerebral cortex will stimulate the vagal center.
The vagal nuclei stimulate gastric secretion by:
Release of gastrin hormone (Gastrin releasing peptide).
Direct stimulation of gastric glands (ACh).
In these glands, many types of cells are present:
Secretion of gastrin hormone:
Regulation of gastrin secretion:
Action of gastrin on:
Ileocecal sphincter→ Relaxation.
Sphincters: - Lower oesophageal sphincter → Contraction.
Pancreas: ↑ exocrine and endocrine secretion.
Stomach: ↑ growth & secretion & motility.
It is secreted from:
T.G cells: in mucosa of stomach and small intestine → G34.
G-cells: in pyloric antrum, flask–shaped cells and have microvilli contains receptors.
It is a polypeptide of 3 types according to number of amino acids G34, G17 (most important) and G14.
Secretion of Mucus:
There are two types of mucus:
Insoluble thick mucus: - Secreted by the surface epithelium. - Viscid alkaline mucus layer to protect gastric wall from digestion & acidity.
The gastric mucosa is protected by: mucosal barrier
Duodenum is protected by mucosal barrier + pancreatic alkaline secretion.
The mucosal cells are impermeable to H+ which is pumped to the lumen and Na+ which is pumped to interstitial fluid
Prostaglandins stimulate the secretion of this alkaline mucus and decrease HCL secretion
The insoluble thick alkaline mucus (1 mm layer).
Soluble thin mucus: secreted by mucus neck cells by vagal as mucoproteins to lubricate gastric chyme.
Secretion of intrinsic factor:
In gastritis → pernicious anemia (↓ B12 anemia).
It is essential for vit B12 absorption in ileum.
It is a glycoprotein secreted from oxyntic cells with HCL.
Secretion of enzymes:
Rennin: milk clotting enzymes (not present in humans).
Amylase (from saliva).
Gastric lipase: act on short chain fat. Its optimum pH = 3.
Gelatinase : which liquefies gelatin.
Pepsinogens (I & II)
HCL secretion:
Mechanism of HCl secretion:
Functions of HCL
↑ absorption of iron (by converting ferric state into ferrous) and calcium (by prevention of calcium salts precipitation).
Initiate enterogastric inhibitory reflex →↓ gastric secretion and evacuation.
Produces curdling of milk.
HCl enters the duodenum → ↑ secretin hormone →↑ bile and pancreatic secretion.
Digestion of protein by activation of pepsinogen → pepsin & give optimum pH of its effect and hydrolysis of protein.
Sterilization by acidity which kills bacteria.
Factors affecting HCL secretion (receptors on parietal cells):
Prostaglandin E2 causes ↓HCl secretion via ↓ cAMP (used in treatment of peptic ulcer).
Gastrin →↑ HCl secretion via special Gastrin Receptors by ↑ intra cellular Ca+2.
Acetyl choline →↑ HCl secretion via muscarinic M3 receptors by ↑ Ca+2 & this effect is blocked by atropin.
Histamine →↑ HCl secretion via stimulation of H2 receptors by ↑ cAMP(these receptors are blocked by cimetidine).
N.B: 3 & 4 (active) 1, 2, 5, 6 (passive).
Diffusion of HCO3 to blood → Na HCo3 → post prandial alkaline tide (↑ pH in blood and urine after gastric secretion).
Water diffused to lumen → iso-osmotic HCL acid.
CL- is actively secreted into the lumen to unite with H+ → HCL.
H2O in cytoplasm → H+ + OH-. The H+ is secreted in lumen in exchange with K+ by H+ - K+ pump and OH- form H2O with H+ from carbonic acid.
H2 CO3 → H+ + HCO3 .The bicarbonate diffuse to blood in exchange with CL
In parietal cell CO2 (from metabolism or blood) → CO2 + H2O
HCL secretion occurs in lumen of canaliculi inside oxyntic cells.
Concentration of H+ ions in gastric juice is one million times the conc. in plasma. So, H+ ions is secreted against a very high gradient.
HCl is secreted by the oxyntic (parietal) cells.
The antrum of pyloric area contains 1, 2, 4& 5 types of cells.
The body & fundus contain all types of cells except G. cells.
The pyloric canal and cardiac region contain goblet cells only.
Enterochromaffin like cells → histamine
D. cells → Somatostatin.
G. cells → Gastrin H.
Oxyntic (parietal) cells → Hcl & intrinsic factor (essential for life for absorption of vit.B12).
Chief cells → Pepsinogen & enzymes.
Mucous neck cells (Goblet) → Mucus.
Simple tubular glands open at the mucosal surface at the gastric pits.
Function of stomach:
Absorption of small amounts of water and alcohol.
Help defecation by gastrocolic reflex.
Secretion of HCl, enzymes,….
Sterilization of ingested food by high acidity.
Partial digestion of proteins and fats.
Slow evacuation of meal to allow good digestion and absorption.
Storage of food.
Mastication (chewing)
It is partly voluntary and partly reflexly by chewing reflex in which:
Presence of food in mouth → reflex relaxation of chewing muscles → drop of mandible and open the mouth → stretch on the muscles → reflex re-contraction and closure of the mouth and so on.(the mastication muscles are supplied by the motor branch of the trigeminal nerve.
Importance
Help digestion by break down of indigestive cellulose membrane around the digestive portion of fruits and vegetables also by increasing the exposed surface area to enzymatic effect.
Help swallowing by lubrication of food by saliva.
Stimulation of taste and smell receptors → sense of satiety.
Definition: It is the process of mechanical breakdown of large food particles into smaller ones in the mouth.
Histology
٢
١
Anatomy
Shaar records
Peritoneum
Subdivisions of the peritoneal cavity:
The peritoneal cavity is a completely closed sac subdivided in lesser and greater sacs, which communicate together through the epiploic foramen.
The lesser sac, or omental bursa, is situated behind the stomach & lesser omentum.
Above: caudate lobe of liver. Below: 1st inch of 1st part of duodenum.
Posterior: The peritoneum covering the I.V.C.
Anterior: The thickened right edge of the lesser omentum.
Contents of the right free border of lesser omentum:
It is 3 cm in height in adults
It leads into the greater sac.
The common bile duct (infront of portal v. & to the right of hepatic a.). Epiploic foramen (of Winslow) is a short, vertical slit in the upper part of the right border of the lesser sac .
Hepatic a. (infront of portal v. and to the left of common bile duct).
Portal v. (posteriorly)
Folds of the peritoneum:
As a role each peritoneal ligament irrespective to its name is formed from two layers except the greater omentum as it is reflected on itself hence formed of 4 layers
Ligaments
Lienorenal ligament.
Phrenicocolic ligament.
Gastrophrenic ligament.
Gastrosplenic ligament.
Falciform ligament.
Mesenteries
Pelvic (sigmoid) mesocolon
Transverse mesocolon.
Mesentery of small intestine.
Peritoneal folds:
Omenta: Lesser & Greater omentum.
Greater omentum:
The anterior one ascends on the anterior surface of pancreas and the posterior passes on its inferior surface.
The two layers descend in the abdominal cavity till the pelvis acting as a rope to protect the abdominal organs then reflected backwards and upwards forming posterior two layers up to the anterior border of the pancreas where they diverge.
It is formed by the peritoneum covering the anterior and the posterior surfaces of the stomach.
stretched between the greater curvature of the stomach and the transverse colon
Lesser omentum: stretched between the lesser curvature of the stomach and the margins of the porta hepatis of the liver. Its right border is free and forms the anterior boundary of the opening into the lesser sac.
These folds have different names according to the organ included as omentum, ligament or mesocolon but the structure is the same.
They function to allow free mobility of the included organs
These folds stretch between the organs covered by peritoneum and the abdominal wall or other organs.
Layers of the peritoneal sac
The peritoneum is a completely closed sac except the opening of the uterine tube in female
The 2 layers are separated from each other by a potential space called the peritoneal sac which contains a film of serous fluid called the peritoneal fluid.
that which lines the abdominal wall is called parietal peritoneum.
The peritoneum covering the organs is called visceral peritoneum
The invaginations by the organs have different forms:
Due to the invagination of the peritoneal sac by the organs and formation of peritoneal folds and the ligaments the peritoneal sac is divided into two sacs; greater and lesser sac, completely separated from each other except at an opening called epiploic foramen (of Winslow) or opening into lesser sac.
Some other organs don’t invaginate the peritoneal sac and covered by the peritoneum anteriorly only e.g., the duodenum.
Other organs invaginate the peritoneal sac to a lesser degree and become covered by peritoneum on the front and sides only.
Some organs invaginate the peritoneum and develop a peritoneal fold connecting them with the posterior abdominal wall. These organs become covered completely by peritoneum except at the line of attachment to the peritoneal fold.
Definition: is a large thin serous membrane, which lines the interior of the abdominopelvic cavity. It forms the largest serous sac of the body.
SMALL AND LARGE INTESTINE
The rectum
Ischiorectal fossa (Ischio-anal fossae)
Contents
Posterior scrotal (or labial) nerves and vessels.
Perineal branch of 4th sacral nerve
Inferior rectal nerves and vessels
Ischiorectal pad of fat.
Boundaries
Floor
Perineal skin.
Post
Sacrotuberous ligament & on post. surface of which is gluteus maximus.
Anteriorly
continuous with recesses that project into the urogenital triangle superior to the deep perineal pouch.
superiorly
The medial & lateral walls converge
Med. wall
external anal sphincter.
Fascia covering the levator ani muscle
Lat. wall
sacrotuberous ligament
ischium
Fascia covering the obturator internus muscle
Measurements: each is 5 cm length x 5 cm width x 5 cm depth
Functions: They help in dilatation of the anal canal, during defecation.
Site & shape: a wedge-shaped, fat-filled space situated on each side of the anal canal below the levator ani muscles. The 2 fossae communicate with each other behind anal canal.
The anal canal
Arterial supply of anal canal: The upper part is supplied by superior rectal a. & the lower part is supplied by inferior rectal a.
Lymph drainage of anal canal:
The lower 1/2 drains into superficial inguinal L.N.
upper ½ drains into pararectal L.Ns and finally into inferior mesenteric L.N.
Nerve supply: by the inferior rectal nerve and the perineal br. of S4 nerve.
The internal features of anal canal:
Features in the lower part of anal canal: The lower anal canal is further divided into two regions: upper and lower.
Anal sphincters:
External sphincter: surrounds the lower 2/3 of the canal. Thus, it overlaps the internal sphincter in the middle third. It is formed from striated voluntary muscle fibers arranged in three parts:
Subcutaneous part: surrounds the anal orifice and has no bony attachment.
Superficial part: arises from the tip of coccyx and anococcygeal body and passes forward around sides of the anus to be inserted into the perineal body.
Deep part: It is a thick annular band that forms the true sphincter and has no bony attachment.
The internal anal sphincter
Nerve supply: it’s involuntary and supplied by sympathetic and parasympathetic fibers. Both are distributed via the inferior hypogastric plexus.
It is a ring of circular smooth muscle fibers which surrounds the upper 2/3 of the anal canal. It is continuous with the circular muscle of the gut. It is thinner in females. It becomes thicker with age and in chronic constipation.
Lower region of lower anal canal: It is about 8 mm in extent and lined by the true skin containing sweat and sebaceous gland. It shows pigmentation. In adult male, coarse hairs are often found around the anal orifice. The junction between keratinized & the non-keratinized parts is indicated by a whitish line called (Hilton's white line).
Upper region (often called pecten): It is 15 mm long and extends from the pectinate line to Hilton’s line. It is lined by the non-keratinized stratified squamous epithelium. The mucous lining in this region appears bluish in colour due to underlying dense venous plexus and is adherent to the underlying structures.
Features in the upper part of anal canal: The upper part of the anal canal (15 mm long) presents the following features:
Anal sinuses: These are vertical recesses between the anal columns and above the anal valves. The ducts of tubular anal glands present in the submucosa open in the floor of anal sinuses.
Anal valves (valves of Morgagni): These are crescentic folds of the mucous membrane which connect the lower ends of adjacent anal columns. The free margins of these valves are directed upward. The position of these valves is indicated by the wavy pectinate line (also called dentate line).
Anal columns (columns of Morgagni): These are permanent longitudinal mucous folds numbering 6 to10. They contain radicles of the superior rectal vein.
The upper and lower parts of the anal canal are different in development, blood and nerve supply and lymphatic drainage.
The upper part extends from the anorectal junction to the pectinate line, while the lower part extends from the pectinate line to the anal verge.
The anal canal is divided into upper &lower parts by the pectinate line.
Relations: see practical
It has no peritoneal covering.
It extends in the anal triangle downwards and backwards between the ischiorectal fossae to end at the anal orifice. It forms a posterior acute angle about 80 degrees with the lower part of the rectum.
It begins at the anorectal junction one inch below and infront tip of coccyx.
It is the terminal part of the large intestine, it is about 2.5 to 4 cm.
Venous drainage of the rectum and anal canal: correspond to their arteries.
Inferior rectal vein: drain into the internal pudendal vein.
Middle rectal vein drains into internal iliac vein.
Superior rectal vein ends in the inferior mesenteric vein which ends in portal vein.
Arterial blood supply of rectum & anal canal:
Inferior rectal artery: branch from the internal pudendal artery, in the perineum, its anastomosis with the middle rectal a. at anorectal junction.
Middle rectal artery: branch from the anterior division of the internal iliac artery.
Superior rectal artery: continuation of the inferior mesenteric artery.
Relations: see practical
The mucosa of the rectum:
They contain circular muscle fibers to support the weight of fecal matter to prevent its descent toward the anal canal as its presence always excites a sensation demanding its discharge. In the empty state of the intestine these folds overlap each other.
These folds are about 12 mm. in width
There are 3 large transverse folds called rectal folds or shelves: known as Houston’s valves. One-fold lies opposite the concave side of the 3 lateral flexures.
It has longitudinal folds.
Flexures of the rectum
Lateral flexures: the rectum has three lateral flexures (curves). The upper &lower are convex to the right. The middle is the most prominent & convex to the left.
Anteroposterior flexures
Perineal or rectoanal flexure (Lower curve): convex forwards. The rectum bents backwards at the anorectal junction to form an acute angle of 80 degree. The rectum pierces the pelvic diaphragm to continue as the anal canal.
Sacral flexure (upper curve): concave forwards. It follows concavity of sacrum.
Peritoneal coverings
The lower third has no peritoneal coverings.
The upper third is covered by peritoneum on front and sides
Unlike other portions of the colon, the rectum does not have taeniae coli or sacculations
It is about 4 cm wide at its beginning (similar to that of the sigmoid colon) but it is dilated near its end to form the rectal ampulla.
It begins at the level of the third sacral vertebra as a continuation of the sigmoid colon and ends at the anorectal junction one inch in front of and below the tip of coccyx where it continues as the anal canal .
It is about 13 cm. (5 inches) long.
The rectum is the terminal part of the large intestine.