arabera Erica Zeitz 6 years ago
215
Ankylosing Spondylitis1 (Erica Zeitz)
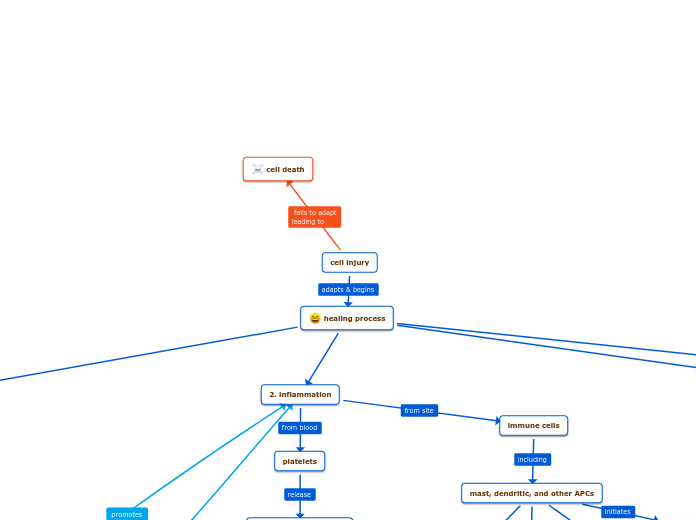
Ankylosing Spondylitis (AS) is a chronic inflammatory disease primarily affecting the axial skeleton, leading to progressive joint fusion over time. The exact trigger for the inflammation is unknown, but it involves the activation of inflammatory cytokines.