arabera Tiye Nesbith 5 years ago
225
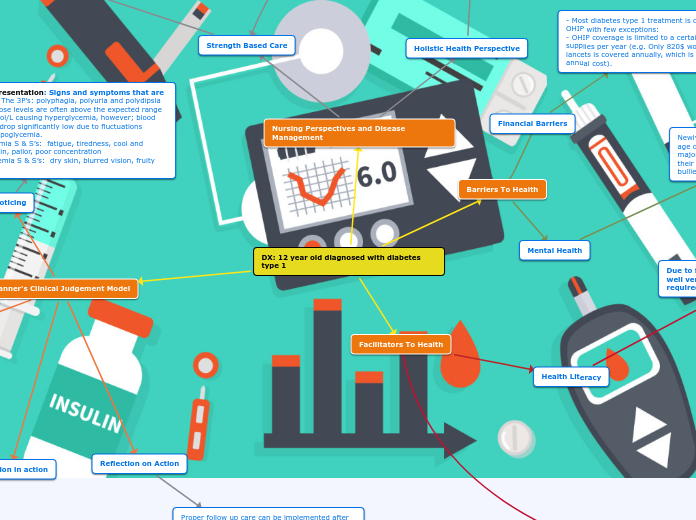
DX: 12 year old diagnosed with diabetes type 1
A 12-year-old patient has been diagnosed with type 1 diabetes, necessitating a comprehensive approach to disease management and care. The nursing perspective emphasizes a holistic health approach, addressing the patient'