arabera Daniel Case 4 years ago
1126
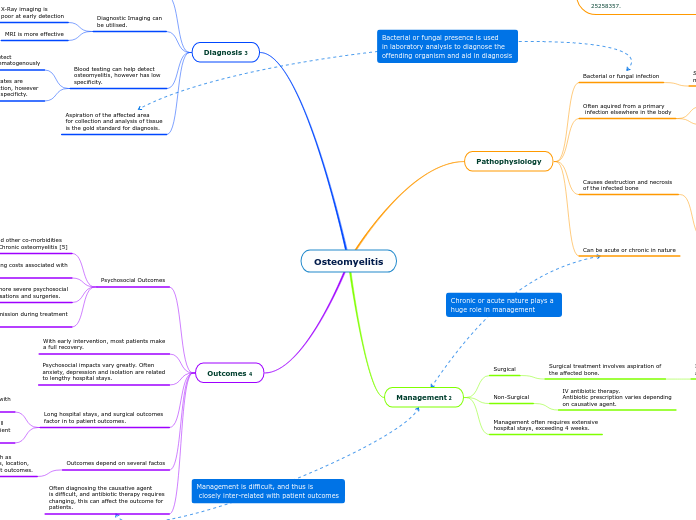
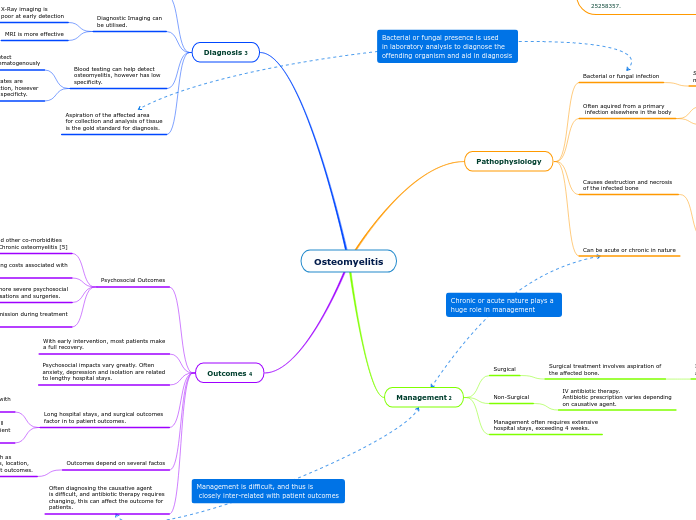
Osteomyelitis
arabera Daniel Case 4 years ago
1126
Honelako gehiago
Fever, local pain and refusal to use affected limb are all common presentations.
Includes removal of dead tissue, purulent matter and amputation.