Diuretics
Natriuretic
drugs which alter renal hemodynamics
do NOT alter transporterscaffeine
dopamine
MOA: DA and beta 1 receptor agonist
frequently combined with dobutamine (beta 1 agonist) in treating post-MI pts w/ poor renal blood floweffects:
renal vasodilatorincreases GFRincreases renin productioncarbonic anhydrase inhib
site 1
acetazolamide
MOA: inhibits both isoforms of carbonic anhydrase, thus inhibiting HCO3 reabsorbtion which also decreases Na reabsorbtion
indications:
NOT useful as diuretics!glaucoma (decreases movement of Na and water in aq humor)second line drug for epilepsyacute mountain sickness (d/t pulm or cranial edema)dissolusion of uric acid stones (b/c of alkanization of urine)metabolic acidosis
b/c it lowers plasma HCO3
K-sparing
site 4
competition with aldosterone
seldom used alone
contraindicated in pt with renal insufficiency
if pt. hypertensive or post-MI
epleronone
MOA: same as spironolactone, except...
specific for the mineralocorticoid receptor (does not bind androgen or progesterone receptors)
spironolactone
MOA: aldosterone receptor competitive antagonist
inhibs ability of aldosterone to increase the Na/K exchange
NOT specific for the mineralocorticoid receptor (also binds glucocorticoid receptors)
effects:
slight diuresis, slight incr Na excretiongreater effect is to inhibit K lossSLOW onset and offset
contraindications
pts w/ impaired renal function
pts w/ diabetes
anti-androgenic effects/hypoandrogenism
menstrual irregularities
impotence
gynecomastia
elevated aldosterone level (in those w/ HF)
hyperkalemia
disruption of electrical gradients
ENaC
triamterene
oral
some hepatic metabolism
shorter t1/2
amiloride
MOA: removes the drive to transport K across the cell (for excretion) -- by inhibiting Na influx thru ENaC, so less Na for the NaK ATPase
oral
unmetabolized (excreted uncharged by the kidney!)
direct inhibition of Na transport
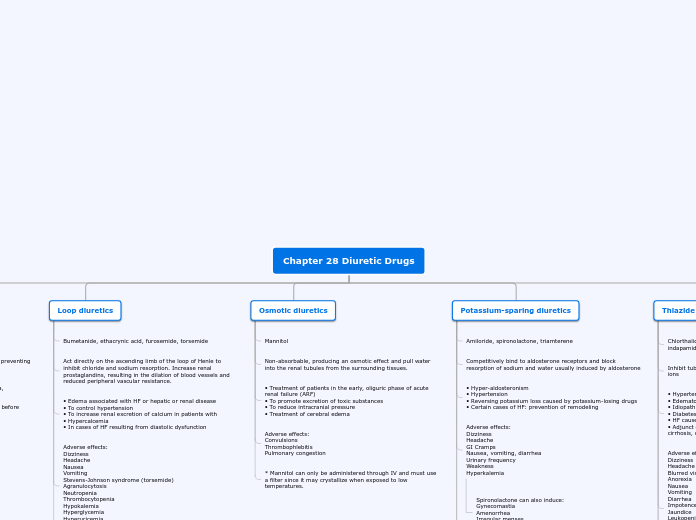
thiazides
site 3
MOA: inhibits NCC (Na/Cl contransporter) -- inhibs NaCl reabsorbtion at DCT
unlike site 2 diuretics, DO NOT LEAD TO COUNTERCURRENT WASHOUT
contraindicated in pts with renal insufficiency!
indications
- essential HT
- CHF (w/ NORMAL renal fxn)
- mild edema
- hypocalcemia & hypercalciuria)
- diabetes insipidus (lack of ADNH)
increased urinary excretion of: Na, K, H
decreased urinary excretion of: Ca, urate, Lo
if pt has high cholesterol or diabetes...
metolazone & indapamide
don't cause hyperglycemia
don't alter lipids
exception to thiazide rule!: effective in renal failure when combined with a loop diuretic
better AE profile
drug interactions
hypokalemia increases digitalis toxicity!!!
glucocorticoids
Li
site 2 diuretics
K-sparing diuretics
may prevent K loss - a useful interaction
AE
hypersensitivity reactions
increased serum lipoproteins, TG, LDL
chlorthalidolone
cholorthizide & hydrocholrothiazide
ineffective when GFR < 30ml/min (low renal fxn)
(loop) high-ceiling diuretics
site 2
torsemide
longer t1/2 permits qd dosing
2x bioavailability as furosemide
if diabetic pt...
ethacrynic acid and bumetanide have lower incidence of hyperglycemia
ethacrynic acid
no sulfonamide group!
bumetanide
potency differs from furosemide
drug of choice
furosemide
MOA: inhibits NKCC2 (by plugging up the Cl site) and also causes 'counter-current' washout
Increases urinary excretion of: Na, K, H, Cl, Mg, CaDecreases urinary excretion of: Urate, LiAlso a vasodilaor (will decr, L ventricular filling pressure and pulm. congestions)worsens gout
GI disturbances
hypertriglyceridemia
hyperglycemia
hyperaldosteronism
ototoxicity
hypokalemia
Osmotic
MOA: trap water in filtrate and osmotically prevent water reabsorbtion + cause diuresis by countercurrent washout
basically, they increase GFR by redistributing water from some place in the periphery to the kidney so that it can be eliminated
Contraindications:
Dehydration
need some water in your body for an osmotic diuretic to redistribute it! osmotic diuretics would make dehydration worse
Heart failure
osmotic diuretics will increase the circulating [pre]load
Natriuretic diuretics are ok to use though b/c they don't increase preload - they alter renal dynamics at the nephron instead of throughout vasculature
Peripheral edema
increasing the vascular volume with an osmotic diuretic will make the peripheral edema worse -- backs up into lungs and can lead to pulmonary edema!
Anuria
need at least SOME urine flow to get the osmotic diuretic out of your system
AE:
n/v
HA
cerebral edema
eventually the osmotic diuretics will diffuse from the plasma compartment out into the CSF -- the excess CSF volume can cause cerebral edema
Uses:
prophylaxis for acute renal failure
as long as there is SOME urine production though
pre-surgery, can reduce intracranial and intraocular pressure
must have at least SOME urine production
Isosorbide
greatest effect on the eye
used mostly prior to ocular surgery
Glycerol
Mannitol