Primary and Secondry Care- First Aid Course
Other skills
Choking
Unconscious
3. Look into patient's mouth to remove visible obstructions
2. CPR
1. Call EMS
Conscious
Or try chest thrusts, put your arms under the persons armpits, similar to abdominal thrust, but this time in the notch on the lower half of the breastbone.
After back blows try abdominal thrusts, put your hands around the waist of a person, make a first and wrap your other hand around it, thrust into 2 finger widths above the navel, thumb side towards you
Deliver Back blows by striking between the shoulder blades with the heel of your hand 5 times
Stop these blows if the person becomes unconscious
Protective Barriers
Barriers
Scrub and wash after exposure with soap or wipes.
Eye/Face Shields- Glasses, goggles, face masks
Ventilation masks/ Face Shields
Gloves
Bloodborne Pathogens
HIV
Hepatitis B virus
Hepatitis C virus
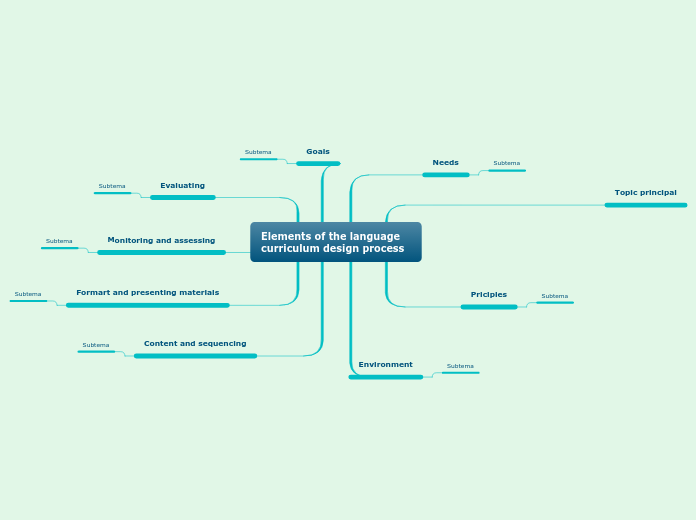
Chain of Survival
4. Early Professional Care and Followup
3. Early Defibrillation
2. Early CPR- Cardiopulmonary Resuscitation
1. Early Recognition, Call for Help
Recognizing Life-Threatening Problems
Complete Airway Obstruction
Deliver Back Blows/ Abdominal Thrusts/Chest Thrusts
Can't speak, clutching throat, leaving area
Choking on food/ object
Stroke
Numbness, weakness, speechless, facial droop, headaches, blurred vision
Blood vessel blocked or bursts in the brain
Cardiac Arrest
CPR, defibrillation quickly
No response from patient, no circulation, heart quivers ventricular fibrillation
Oxygen flow to heart stops or is reduced
Heart Attack
Calling EMS immediately, transport to medical facility
Complain of chest pain, dizziness, breathlessness
Blood flow to heart stops or is reduced.
Emotional Aspects of Being an Emergency Responder
3. Relax, avoid caffeine, alcohol, talk to others after providing emergency care, it might be stressful.
2. CPR only helps support a patient by forcing oxygen-rich blood to the vital body organs from the heart, it does not restart the heart.
1. A person without a heartbeat or who isn't breathing is already in the worst state of health, you can't worsen the condition...
Definitions
Symptom
Something the patient tells you is wrong
Sign
The responder sees, hears or feels
Injury
Physical Harm: cuts, burns, dislocations...
Illness
Unhealthy condition: diabetes, allergies...
Helping Others in Need
Good Samaritan Laws
6. Don't abandon a patient, unless you are protecting yourself from danger.
5. Act prudently.
4. Do not be reckless or negligent.
3. Act in good faith.
2. Ask for permission to help.
1. Only provide care that you have been qualified for as a Emergency Responder.
Protect individuals who voluntarily aid those in need, immunity against liability.
Why do some people NOT HELP?
Fear of infection
Responsibility
Fear of imperfect performance
Guilt
Anxiety
Why Help?
You can make the difference between a patient having a temporary or lifelong disability.
You can help reduce a patient's recovery time.
You can save or restore a patient's life.
Why Time is important?
Irreversible brain damage can occur
Chances of a successful resuscitation diminish with time
Differences When Providing Care to Children
Mental state and willingness to cooperate
Ability to understand what is going on or to communicate effectively
Size
Age
Secondary Care
Splinting for Dislocations and Fractures
Use a donut bandage to wrap around a jutting out bone before wrapping it
Use roller bandages to wrap around the splint to hold it in place
Put leg or arm into splint
Put padding onto a straight surface bending surface (splint)
Bandaging
Triangle Bandages: to hold up arm, tie around neck
Tuck bandage into place
Apply sterile pad on wound, apply bandage over pad
Illness Assessment
SAMPLE
Events
Before illness
What happened
Last Meal
What
When
Alcohol if taken
Preexisting Medical Conditions
Heart condtions, diabetes...
Medications
Did you take it today
What medication they take
Allergies
Ask for what they are allergic to
Signs and Symptoms
Checking temperature and moisture
Check Color of skin
Find pulse rate and breathing rate
Ask how they feel
Injury Assessment
Ask the patient to use his eyes to follow your finger
Check ears for body fluid
Check from head to toe, feel the bones to find any dislocations or fractures
What is Normal?
Infant
100-160 beats per minute
30-60 breaths per minute
Child
70-150 beats per minute
18-40 breaths per minute
Adult
60-80 beats per minute
12 and 20 breaths per minute
Primary Care
S
Spinal Injury Management
Move patient as a unit, don't turn spine... use a log roll
Don't let the patient move
Hold neck still even if you are not moving the patient
Never move a patient unless absolutely necessary
Shock Management
3. Elevate the legs 15-30 cm if no spinal injuries or leg fractures
2. Maintain patient's body temperature based on climate
1. Hold the patient's head to keep the neck from moving, do not move patient
Shock occurs when only one or more vital organs get blood, others don't get adequate blood, organs need oxygen from blood
Shocked people a weak pulse, pale moist skin, mental confusion, nausea, thirst, lackluster eyes, labored breathing
Treat anyone who does not need CPR with the shock management procedure
Serious Bleeding Management
How to treat
NEVER remove blood soaked bandages- blood clots more easily
Place pressure, wrap bandages around
Put a sterile pad over wound and apply pressure
Capillary Bleeding
Can stop on its own or stopped easily with direct pressure
Blood slowly oozes from the wound
Venous Bleeding
Can be life-threatening and must be controlled quickly
Dark red blood steadily flows from the wound
Arterial Bleeding
Most serious type of bleeding, blood loss occurs quickly
Bright red blood spurts from a wound in rhythm with heartbeat
D
Defillibration
Use an AED, stick pads on patient and listen to the machine's instructions, remember to ask everyone to move back from the patient. Use a Child AED for children, no AED use on infants.
Administering an electric shock which disrupts the abnormal twitching (fillibration) is called Defillibration.
C
Circulation & Chest compressions
7. Repeat 2 rescue breaths and 30 compressions procedure until there is an AED or EMS comes
6. Compression site: Between the two nipples, center of chest Give 30 compressions, straight down, straight arms
Infant- 2 fingers
Children- one hand
Adult- two hands
5. Give 2 rescue breaths to make the chest rise
4. Pinch nose close, tilt head to lift chin
3. Put ventilation barrier on patients mouth and nose
2. Remove obstructions from mouth
1. Put patient on his back
B
Breathing
Unconscious Patient: Put ear to patient's mouth and look towards chest to see see rise and fall, if not, go to C.
Check patient for Breathing, periodic gasping is not regular breathing
A
Airway
Unconscious Patient: Tilt chin backwards to open airway
Conscious Patient: Ask him to speak/ cough, go to S.
Asking for Permission
No= No, I'm fine, don't help me, just talk to me...
No answer/ Yes= Go and help me!!!
"Hello, my name is Michelle, I'm an Emergency Responder, may I help you?"
Applying Barriers
Serious Bleeding- Put on face shield/ eye shield/ goggles/ glasses
CPR- Put ventilation mask on patient's mouth
Wear gloves before touching the patient
Alerting EMS
Respiratory problem- 2 minutes of CPR and then alert EMS
If there is a bystander nearby, ask them to do so, or do so yourself unless respiratory problem or the patient is a child
Assessing the Scene
Check for what might be a danger to the patient or yourself
Check for what might have caused the accident